Kidney Disease Lifestyle Changes
Chronic kidney disease is more than just a diagnosis, it is a condition that marks major changes. To live comfortably and maintain as much kidney function is possible, there are a lot of big lifestyle changes you will need to make.
The idea of making lifestyle changes can feel daunting, but really the changes you need to make are similar to any general healthy lifestyle.
By altering your diet, exercising regularly, and managing habits like smoking and alcohol consumption, you can significantly ease your kidneys' work.

It's not easy, but you're not alone. Let's explore how lifestyle changes can help manage your condition while improving overall well being.
Remember, every positive change counts!
Jump to:
- Key Takeaways
- Understanding Chronic Kidney Disease and the Need for Lifestyle Changes
- How Exercise Contributes to a Healthy Lifestyle with Chronic Kidney Disease
- The Impact of Smoking on Kidney Health
- The Effects of Alcohol Consumption on Ailing Kidneys
- Fluid Restrictions and Their Role in Chronic Kidney Disease Management
- Medical Management and Regular Follow-ups for Chronic Kidney Disease
- The Connection Between Chronic Kidney Disease and Other Metabolic Conditions
- Understanding the Risk of Heart Disease as a Chronic Kidney Disease Patient
- Ways to Keep Your Blood Pressure Under Control with Chronic Kidney Disease
- FAQs for Life Style Changes For People
- Lifestyle Changes Are Crucial When Managing Kidney Disease
Key Takeaways
- Changes to diet have the biggest impact on kidney health and can lower the risk of progression in patients with kidney disease.
- Physical activity is important for people with chronic kidney disease as it helps achieve and maintain a healthy weight, lowers blood pressure, and strengthens the body.
- Consumption habits such as smoking exposure and excessive alcohol consumption can have a significant negative impact on kidney health.
- Some individuals may need to limit their fluid intake as part of managing chronic kidney disease and individualized guidance from healthcare providers is important for fluid management.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding Chronic Kidney Disease and the Need for Lifestyle Changes
As we delve into our discussion on preventing chronic kidney disease (CKD) progression, it's crucial for you to understand the pivotal role your lifestyle choices play in this process. Particularly, your diet can significantly impact kidney disease by leading to a slower decline in kidney function.
The foods you consume can have a profound effect on your kidneys. We'll explore the intricacies of a kidney-friendly dietary regimen and discuss how specific dietary patterns can efficiently delay the progression of CKD to end-stage renal disease.
Improving kidney function is possible by making smart lifestyle modifications, like following a renal-friendly diet and maintaining regular physical activity. Exercise interventions benefit not only your kidney health but also assist in preventing chronic diseases in general. Besides, it's essential that you also consider quitting smoking and alcohol moderation (renal diet and alcohol).
| Lifestyle Modifications | Benefits |
| Renal Friendly Diet | Slows or stops the progression of CKD |
| Regular Exercise | Improves kidney function and quality of life |
| Quitting Smoking | Improves blood flow to important organs, including the kidneys; lowers the risk of heart attacks and strokes in people with hypertension |
| Alcohol Moderation | Avoids hypertension, which can lead to kidney damage. |
Always consult with your healthcare provider for personalized advice tailored to your condition.
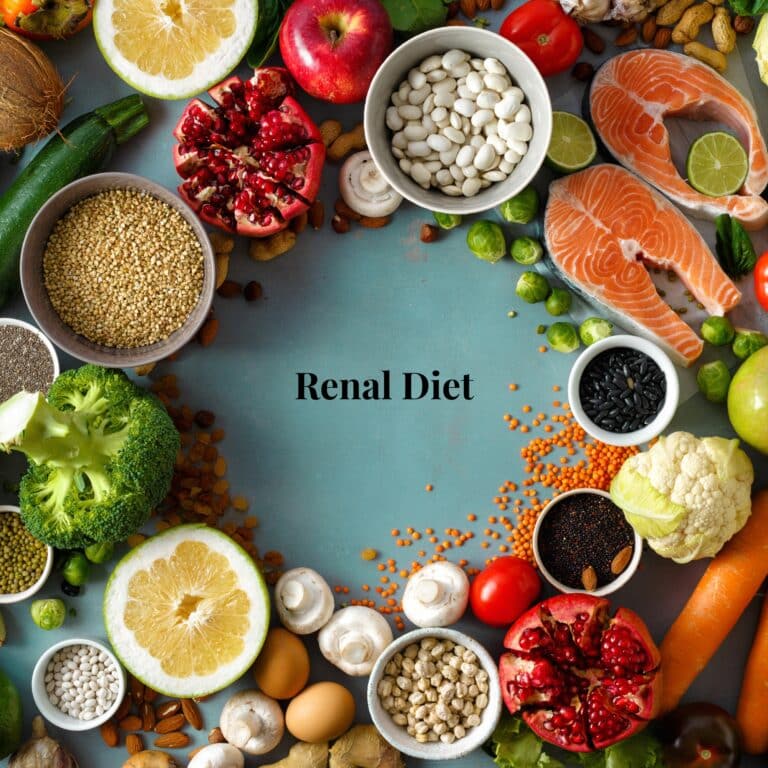
Healthy Diet for Kidneys
The biggest changes you will need to make are changes to your diet. Your diet has the biggest impact of all because what you eat or drink is ultimately filtered through your kidneys. This means that eating a kidney-friendly diet can put less stress on your kidneys.
Diet is so important that you can actually change the outcome of your chronic diseases by making healthy choices. A stringent kidney safe diet can help you slow or even potentially stop the progression of CKD. This means that you could potentially avoid end-stage kidney disease and avoid needing a kidney transplantation.
You're better off sticking to a balanced, nutritious diet for maintaining good health of your body's natural filtration system. Incorporating kidney friendly recipes into your meal prep can significantly impact your health.
Prioritize kidney safe foods such as fruits, vegetables, whole grains and lean proteins. Nutritional supplements may also aid in filling dietary gaps but should always be used under medical supervision.
Fluid intake management is crucial; keeping hydrated helps the kidneys clear waste products while preventing over-hydration helps avoid many problems, such as shortness of breath, and swelling.
Nutrition Guidelines for CKD
It's essential to understand that for individuals with CKD, adhering to nutritional guidelines can significantly improve their health and well being. Renal nutrition is incredibly important and involves several key aspects.
It's important to note that the dietary interventions for CKD may vary depending on the stage of the disease and individual factors, so it's important to work closely with a registered dietitian who specializes in kidney disease.
A registered dietitian can provide personalized renal diet tips that cater to your taste preferences while keeping your health parameters in check.
With this mind, here are some general nutritional management guidelines for CKD:
Restrict protein intake: In advanced stages of CKD, it is often recommended to limit protein intake to reduce the burden on the kidneys. This helps to slow down kidney disease progression.
Eating more plant-based proteins instead red meat intake can be beneficial for patients with CKD and patients with type II diabetes. Protein restriction is individualized based on the stage of CKD and other factors, so consult with a healthcare professional for specific recommendations.
Control sodium (salt) intake: High sodium intake can lead to fluid buildup and increased blood pressure, both of which can worsen kidney function. Limiting sodium in the diet can help manage blood pressure and fluid balance. Avoid adding salt to meals and minimize the consumption of processed and packaged foods, as these are usually high in sodium.
Regulate potassium intake: Potassium is a mineral that needs to be controlled in CKD, as kidney function decline in patients with CKD can lead to high potassium levels (hyperkalemia). High potassium intake can be dangerous for the heart and cause other complications.
Foods high in potassium, such as bananas, oranges, tomatoes, and potatoes, may need to be limited or avoided. Again, individual recommendations will depend on the stage of CKD and blood potassium levels.
Manage phosphorus intake: In addition to sodium and potassium intake, the kidneys may also struggle to eliminate excess phosphorus, leading to high levels in the blood. High phosphorus levels can cause bone weakness, bones, itchy skin and cardiovascular disease.
Foods rich in phosphorus, such as dairy products, chocolate, and dark colas, may need to be limited. Additionally, your healthcare professional might prescribe phosphate binders to help control phosphorus levels.
Generally speaking, you should aim for a kidney-friendly diet that's rich in essential nutrients but low in sodium, potassium, and phosphorus to protect your kidneys from further damage. Nutritional counseling plays a pivotal role in guiding you through this journey of diet modifications.
Remember, every small change you make towards a healthier lifestyle counts, be it reducing processed foods or incorporating more fresh fruits and vegetables into your meals.
How Exercise Contributes to a Healthy Lifestyle with Chronic Kidney Disease
You might be wondering how physical exercise fits into your lifestyle, especially when dealing with CKD. Well, engaging in moderate-intensity physical activity can significantly enhance your renal health.
It can do this by promoting healthy weight and preventing cardiovascular risks, both can be crucial to mitigating the risk of progression of symptoms for CKD, which can help you avoid the need for a kidney transplant.
Let's delve deeper into this topic to examine the benefits of incorporating exercise into your routine and how it could potentially transform your everyday life with CKD.
Benefits of Physical Activity
Benefiting from regular physical activity, it's possible to strengthen your heart and enhance overall stamina. This is especially crucial for kidney disease patients.
Physical exercise improves kidney function by regulating blood pressure and blood sugar levels in people with diabetes. High blood sugar levels in diabetic patients can damage the kidneys by damaging the vessels and the filtration units inside the kidneys, which are known as nephrons.
CKD patients often experience muscle wasting and weakness due to activation of protein degradation. Resistance training can help preserve and enhance muscle strength in people with kidney disease.
Patients with kidney disease may experience psychological challenges such as depression, anxiety, and stress. Exercise can help alleviate these symptoms by promoting the release of endorphins, the "feel-good" hormones, and improving overall mental well-being.
In essence, adopting healthier habits like regular exercise while avoiding detrimental ones such as smoking or excessive drinking can significantly promote kidney health. Always consult your healthcare provider before initiating any new regimen.
Recommended Exercises for Kidney Health
Incorporating even small changes in physical activity can strengthen your heart muscle and positively impact kidney health. Exercise benefits extend beyond just weight management; it improves blood pressure, glucose control, and overall stamina. It's important to understand more about high blood pressure and kidney disease.
Here are a few suggestions for exercise routines:
- Moderate intensity activity like walking or cycling can be easily incorporated into your daily routine.
- Resistance training exercises can build endurance and improve muscle function.
- Flexibility exercises such as Pilates can enhance your posture and can even improve your lower back pain.
According to the National Kidney Foundation, three days of activity per week is the bare minimum required to achieve the health benefits of your exercise. 30 minutes of exercise each session are recommended, but remember to stop your session if you feel light-headed, short of breath, or if you feel chest pain.
Remember, it's essential to consider exercise modifications based on your current health status. Always take precautions to avoid injury, start slow and gradually increase intensity. Most importantly, find an exercise you enjoy for sustained motivation.
Regular physical activity is a powerful tool in managing kidney health.
The Impact of Smoking on Kidney Health
You're probably aware that smoking can have detrimental effects on your lungs, but did you know it's also a risk factor for kidney disease?
When you smoke, the toxins introduced into your body can lead to reduced blood flow to the kidneys, causing them to function less effectively over time.
Smoking raises blood pressure levels, and high blood pressure is a leading cause of CKD. When combined with the already compromised kidney function in CKD, smoking can further increase the risk of developing hypertension and exacerbate kidney damage.
Smoking can interfere with the effectiveness of medications used to treat CKD. For example, certain blood pressure-lowering medications, such as angiotensin-converting enzyme (ACE) inhibitors, may be less effective in smokers compared to non-smokers.
Accordingly, you're encouraged to quit smoking. Engage in regular exercise to prevent vascular diseases and follow a balanced diet for overall health maintenance. Remember: Your efforts make a significant difference in preventing life-threatening conditions and promoting a healthier life.
The Effects of Alcohol Consumption on Ailing Kidneys
As you navigate your journey with kidney health, it's crucial to understand the potential impact of alcohol intake in patients with kidney disease.
Chronic alcohol consumption can pose significant risks to kidney health, including the alteration of kidney structure and impairment of its vital functions, leading to conditions like alcoholic nephropathy.
In our forthcoming discussion, we'll delve into how exactly alcohol affects your kidneys and why moderation or abstinence might be a key component in maintaining not only your renal health but overall well being.
Alcohol and Kidney Function
You'll want to watch your alcohol consumption as it can strain your kidneys, especially when coupled with high blood pressure. Similar to smoking, alcohol can cause high blood pressure, a leading cause of kidney disease.
Binge alcohol drinking can also cause liver damage, leading to alcoholic liver disease. Liver disease can affect the rate of blood flow that reaches the kidney, which affects how well the kidney works.
Alcohol is a diuretic, which means it increases urine production and can contribute to dehydration. According to the National Kidney Foundation, dehydration can be particularly harmful to individuals with CKD, as it can disrupt kidney function and can also lead to kidney stones and urinary tract infections.
Moderation in drinking aids in blood pressure management and maintaining liver health, which are vital for combating kidney disease. Remember, moderation isn't just a suggestion; it's crucial for those battling kidney disease. There is a 7 day meal plan for kidney disease you can check out to get a better idea of what to consume, food wise.
Other Risks of Alcohol Consumption
Excessive drinking isn't just bad for your kidney. It also puts you at risk of developing other serious health complications.
CKD patients already have an increased risk of cardiovascular disease. Excessive alcohol consumption can further raise this risk by contributing to the development of conditions such as heart disease and stroke.
Excessive alcohol use is associated with an increased risk of various types of cancer, including liver, mouth, throat, esophagus, breast, and colorectal cancer. The risk increases with higher alcohol consumption.
Excessive alcohol use can irritate and damage the digestive system, leading to many issues such as gastroesophageal reflux, stomach ulcers, intestinal injuries, and malabsorption of nutrients.
Chronic heavy drinking weakens the immune system, making the body more susceptible to infections such as pneumonia and other respiratory illnesses. It can also impair the body's ability to heal wounds.
So take care of yourself and those around you by making informed decisions about modifiable lifestyle factors like drinking and smoking.
Fluid Restrictions and Their Role in Chronic Kidney Disease Management
You've likely heard how crucial fluid control is when managing CKD, but do you understand why?
It's not just about avoiding excess fluid intake (fluids to hydrate with kidney disorder); patients with stage 1-2 of kidney disease may be advised to increase their fluid intake rather than decrease it.
We'll delve into the importance of fluid control and provide practical tips to effectively manage your water intake, aiding you in taking a proactive approach to your health.
Importance of Fluid Control
It's crucial to note that managing your fluid intake is often a necessary step when living with kidney disease. Fluid restrictions may be part of your personalized fluid guidelines provided by healthcare professionals. These guidelines assist in controlling the workload on your kidneys, allowing them to function more efficiently.
To make the process less daunting, consider these simple steps:
- Keep track of your daily fluid intake
- Be aware of hidden fluids in foods
- Follow professional advice on fluid restrictions
- Stay vigilant about changes in body weight
With these tips, you can learn about managing your kidney disease.
Medical Management and Regular Follow-ups for Chronic Kidney Disease
As you navigate your journey with CKD, understanding the importance of regular check-ups cannot be overstated. Regular consultations with healthcare professionals ensure timely detection and management of any complications that could arise, thus aiding in optimal disease control.
Additionally, adopting effective medication adherence strategies is crucial. This doesn't just involve taking your medications as prescribed, but also includes understanding their purpose, managing side effects, and knowing how they interact with other drugs or foods. Here is a list of of commonly prescribed medications for CKD.

Importance of Regular Check-Ups
Regular blood tests and urine tests may be required when you're dealing with kidney disease, as they allow your healthcare providers to track the progression of your condition and adjust your treatment plan accordingly.
Understanding kidney function is critical in managing this disease. Stress can negatively impact your kidneys, so it's essential to learn stress management techniques. Don't underestimate the importance of hydration for kidney health; drinking enough water helps flush toxins from your body.
Medication Adherence Strategies
You've got to stick to your prescribed medication routine, as it can play a key role in maintaining your overall health. Here are some medication adherence strategies for you:
- Understand Your Medication: Take the time to fully understand your medications. Ask your healthcare provider about the purpose, dosage, and potential side effects of each medication you are prescribed. This knowledge will help you recognize the importance of adhering to your prescribed regimen.
- Organize Your Medications: Keep your medications organized to avoid confusion and ensure you take the correct doses. Use pill organizers or blister packs to separate your medications by day and time. This will help you stay on track and prevent missed doses.
- Involve a Support System: Inform your family members or caregivers about your medication regimen. They can provide support by reminding you to take your medications, helping you organize them, and offering encouragement throughout the process.
- Communicate with Your Healthcare Provider: If you have concerns or questions about your medications, don't hesitate to reach out to your healthcare provider. Clear communication is essential for understanding your kidney disease treatment diet plan and addressing any issues that may arise.
Remember, medication adherence is a vital part of managing your health. By following these strategies and maintaining open communication with your healthcare provider, you can optimize the effectiveness of your treatment plan.
The Connection Between Chronic Kidney Disease and Other Metabolic Conditions
As you delve deeper into the complexities of CKD, it's crucial to understand its relationship with other metabolic conditions.
You'll find that certain shared risk factors, such as obesity and diabetes, form a link between CKD and these metabolic disorders.
This intricate connection necessitates a comprehensive approach to management, which includes patient-focused advice on lifestyle modifications, vigilant monitoring of your health status, and effective medical interventions.
Controlling Metabolic Conditions
Controlling metabolic conditions like diabetes and high blood pressure can lead to reduced risk of CKD. By implementing lifestyle modifications, you can manage metabolic syndrome and improve kidney health.
- Managing Diabetes: Keep your blood sugar levels in check with medications, diet, and regular exercise (ckd and diabetes medications).
- High Blood Pressure Control: Monitor this regularly; a healthy diet and physical activity play a vital role.
- Role of Diet: A balanced diet low in sodium, sugar, and unhealthy fats helps you control these metabolic diseases.
- Regular Exercise: Incorporating daily physical activities promotes weight management and helps control metabolic conditions.
Remember that managing these conditions is not only about prolonging life but also enhancing its quality. Always consult healthcare professionals for personalized advice regarding your condition.
Understanding the Risk of Heart Disease as a Chronic Kidney Disease Patient
As a patient managing CKD, you're likely well aware that your heart health is intrinsically connected to your renal wellness.
Therefore, adopting preventative strategies for heart disease is not just advisable; it's crucial.
Regular medical check-ups play an integral role in this prevention plan as they enable early detection and management of potential complications, ensuring that you're always one step ahead in maintaining optimal cardiovascular health.
Heart Disease Prevention Strategies
Heart disease prevention strategies can significantly improve kidney health, and they're often incorporated into lifestyle changes for kidney disease patients.
Including heart healthy recipes in your diet not only boosts cardiovascular health but also aids in managing kidney disease. Regular aerobic exercise is another preventive measure you can take to improve your cardiovascular health.
Stress management techniques are essential; stress negatively impacts blood pressure which, in turn, also affects your kidneys. The benefits of meditation should not be overlooked, it aids relaxation and stress reduction to maintain a healthy blood pressure level. Lastly, don't underestimate the importance of regular sleep, it's crucial for overall well-being including heart health.
Ways to Keep Your Blood Pressure Under Control with Chronic Kidney Disease
Navigating the complexities of hypertension as a patient with CKD can seem daunting, but you're not alone on this journey. Incorporating specific dietary strategies in your daily routine could significantly help manage your blood pressure levels, and it's essential to understand these tactics.
Furthermore, adhering strictly to prescribed medication regimens is paramount. It's not just about taking the right pills, but also about timing and consistency.
Dietary Strategies for Hypertension
Adjusting what's on your plate can significantly help in managing high blood pressure, a common issue for those with kidney disease. Adhering to specific dietary strategies to lower blood pressure can be transformative. These include the DASH diet, sodium reduction, and limiting alcohol intake.
Here are three key steps you should consider:
- DASH Diet: Embrace the Dietary Approaches to Stop Hypertension (DASH) diet, which is rich in fruits, vegetables, and low-fat dairy products. The dash diet for kidney disease is something you can learn more about.
- Sodium Reduction: Limit your dietary intake of sodium by avoiding processed foods and adopting home-cooked meals.
- Alcohol Monitoring: Keep a careful eye on your alcohol consumption to avoid hypertension.
FAQs for Life Style Changes For People
Stress can exacerbate chronic kidney disease, making management more challenging. It's vital you adopt stress management techniques like meditation or yoga (yoga and ckd). Regular exercise impacts positively on your overall mental well being as well.
Medications can play a crucial role too, so ensure you're taking them if prescribed by your healthcare provider. Strive for a work-life balance to reduce constant high-stress levels.
You'll find various support resources for chronic kidney disease lifestyle changes. Dialysis adjustment guidance can be provided by your healthcare team.
Nutritional counseling will help you with proper modification of diet to ensure it's kidney-friendly while physical activity recommendations will help you maintain overall health.
Online communities offer emotional and practical advice from those experiencing similar situations. Additionally, financial assistance programs exist to ease the burden of treatment costs.
It's critical to seek out these supports as they play a key role in managing your condition effectively.
While alternative therapies like acupuncture might be beneficial for people with kidney disease, you should consult your healthcare provider before deciding to use them.
Herbal supplements and traditional remedies might interact with your medications and worsen your condition.
Homeopathic approaches require careful consideration as studies are still needed to make sure they are safe in kidney disease management.
Always consult your healthcare provider before starting any new treatment strategy.
Chronic kidney disease can impact your mental health, leading to conditions like depression. Building emotional resilience is key.
Try incorporating mindfulness practices into your daily routine to help manage stress and improve mood. Cognitive therapy can provide useful tools for coping with the mental effects of this condition.
Prioritizing holistic wellness, which includes both physical and mental health, will make a significant difference in your journey with kidney disease.
Always remember, you're not alone in this fight.
Chronic kidney disease may alter your ability to travel or engage in social activities. Travel adjustments, like planning for medical needs and dialysis services, become necessary.
Social modifications might involve dietary changes at gatherings. Mobility concerns can affect sightseeing or outdoor activities during vacations. Thus, vacation planning requires extra thought and preparation.
Despite activity restrictions, remember it's still possible to enjoy life and maintain a social presence with careful management.
Lifestyle Changes Are Crucial When Managing Kidney Disease
Chronic kidney disease is definitely a condition that will require some major changes. Maintaining an appropriately healthy lifestyle is going to be key to longevity and maintaining your comfort.
Your lifestyle and diet especially will need to become whatever keeps you the healthiest. Regular exercise, and quitting smoking and alcohol can lessen kidney stress.
Talk to your healthcare provider about what lifestyle changes you need to make, and what changes you may face further down the road. Remember that these efforts do not just benefit your kidneys but also boost overall health and longevity.