High Blood Pressure and Kidney Disease
High blood pressure, a pervasive health concern, emerges as a key contributor to chronic kidney disease (CKD). This article navigates the intricate connection between these two conditions, unveiling the profound impact of hypertension on renal health.
High blood pressure can worsen kidney disease, affecting kidney function. It is important to understand this connection to prevent and manage both conditions effectively.
Examining this relationship provides insights into comprehensive approaches that protect kidney function while effectively managing high blood pressure, promoting a pathway towards enhanced health outcomes.
Jump to:
- Key Takeaways
- Importance of Accurate Blood Pressure Measurement
- Technique for Home Blood Pressure Monitoring
- Interpreting Blood Pressure Measurements
- Consultation With a Doctor for Blood Pressure Targets
- Reporting Blood Pressure Measurements
- Understanding High Blood Pressure and Kidney Function
- Complications on Kidney Health and Beyond
- Prevalence of Hypertension and Kidney Disease
- Prevention Strategies for Kidney Disease Stemming From Hypertension
- Lifestyle and Dietary Recommendations for Maintaining Kidney Health
- Comprehensive Guidelines for Kidney-Friendly Eating Habits
- Overview of Stress Management Techniques to Support Kidney Health
- Frequently Asked Questions
- Controlling Your Blood Pressure Protects Your Kidneys
Key Takeaways
- High blood pressure can damage the blood vessels in the kidneys, leading to impaired waste and fluid removal and potentially a heart attack.
- Prolonged high blood pressure can ultimately result in kidney failure.
- Lowering blood pressure is key to preventing or slowing the progression of kidney disease.
- Lifestyle changes, such as being physically active, maintaining a healthy weight, and following a healthy diet, can help control blood pressure and protect the kidneys.
Importance of Accurate Blood Pressure Measurement
Accurate blood pressure measurements are crucial in managing high blood pressure and subsequent advanced kidney disease. You'll find that readings from home can differ significantly from those taken at the doctor's office.
Understand that the accuracy of these measurements hinges on correct techniques and consistency, which include using a recommended home monitor, preparing appropriately, and following the right steps during the process.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Distinction between Home and Doctor's Office Measurements
You may notice a distinction between home and doctor's office measurements of your blood pressure, highlighting the importance of accurate home measurements. This discrepancy could be due to factors such as the selection of appropriate monitor equipment or protocols for relaxation prior to measurement.
To enhance accuracy, invest in an arm cuff monitor, ensure it's correctly calibrated, and follow relaxation techniques before taking readings. Keep a detailed record, noting any fluctuations in your readings; it's vital for tracking progress and adjustments in blood pressure management.
To effectively record measurements at home, jot down your readings and any relevant circumstances surrounding them. Remember, accurate home monitoring can assist your healthcare provider in tailoring your treatment plan and serves as a crucial tool in managing your health.
Essential Techniques for Accurate Measurement
While it's essential for your health to monitor your blood pressure at home, it's equally crucial to ensure the measurements you're taking are accurate.
Selection of appropriate equipment is vital; ensure you're using a validated device and an appropriately sized blood pressure cuff. Remember the importance of relaxation techniques; ensure you're calm and rested prior to measurement.
Understanding your pulse rate and its relationship to your blood pressure can help you gauge your overall cardiovascular health.
Based on your health status, tailoring individual targets with your healthcare provider can optimize your blood pressure control.
Lastly, effective measurement documentation is key; always record the date, time and any unusual circumstances surrounding your reading.
- Choose the right equipment
- Practice relaxation techniques
- Understand your pulse rate
- Tailor your targets
- Document accurately
Technique for Home Blood Pressure Monitoring
To manage hypertension and prevent kidney damage, it's crucial to monitor your blood pressure accurately at home. You'll need to select an appropriate monitor, preferably one with an upper arm cuff, and adhere to pre-measurement relaxation protocols.
This technique ensures a clear record of your blood pressure extremes, helping to guide your doctor's recommendations for treatment.
Selection of Appropriate Monitor Equipment
Choosing the right home blood pressure monitor is a pivotal step in accurately tracking your blood pressure and managing your kidney health. You should consider the following selection criteria:
- Accuracy assessment: Ensure the device is clinically validated for accuracy. Ask your healthcare provider for a list of recommended models.
- User-friendly features: Look for a monitor that's easy to use, with readable numbers and simple instructions.
- Cost considerations: While price is a factor, it shouldn't compromise the quality or accuracy of the monitor.
- Long-term durability: Choose a monitor that's robust and offers reliable performance over time.
Protocols for Measurement
When you prepare to measure your blood pressure, make sure you are in a quiet place and not talking. Believe it or not, that increases your blood pressure. So don't talk to anyone while you are measuring your blood pressure. Remove tight clothing from your upper arm so as to not further constrict the area. And don't drink, eat, exercise or smoke within 30 minutes before you take the measurement. All of those affect your blood pressure.
Sit in a chair, don't stand. Sit upright and let your arm rest comfortably on the table with your feet on the floor. You want to have the cuff at the same level as your heart and your palm facing up. This allows the measurement to be the most accurate.
Before you press the start button, take a few breaths and relax. Then, once you press the button, continue to be calm and quiet. Once the machine is done, you can look at the measurement.
Looking at the monitor, you will usually see 3 lines of information.
SYS means systolic blood pressure, and that should be below 130 mmHg. That is the pressure when your heart is contracting and pushing blood through the arteries. It is the pressure about ⅓ of the time.
DIA means diastolic blood pressure and it should be below 90 mmHg. When your heart is relaxed and between beats, this is the pressure that is placed on your arteries. That is the pressure about ⅔ of the time.
The final number is usually Pulse - that is the number of beats per minute in your body. While there are no cut and dried rules about how high or low this number is, it is usually better if it is lower. Talk to your doctor about what your number should be.
Finally, if you need to take another measurement close together, wait 3 minutes between measurements. The wait time allows your blood vessels to recover and return to their original condition. Then follow the previous steps to ensure you are doing it properly.
Your blood pressure measurements should be recorded on a piece of paper and taken to your doctor's appointment. Make sure you record not only the numbers but the time of day and if you recognize any specific issues - you are not feeling well or didn't sleep well.
Interpreting Blood Pressure Measurements
Understanding your blood pressure readings can be crucial for managing both hypertension and kidney disease. When you take your blood pressure, you'll see two figures: the systolic (SYS) and diastolic (DIA) readings, which should ideally be below 130 mmHg and 90 mmHg respectively.
Monitoring your pulse rate, or the number of heartbeats per minute, is also significant as it can indicate your heart health and how hard it's working.
Clarification of Systolic (SYS) and Diastolic (DIA) Readings
Monitoring your blood pressure involves understanding the key readings, namely systolic (SYS) and diastolic (DIA) pressures. These represent the force exerted by your blood on your artery walls during (SYS) and between (DIA) heartbeats. Keeping track of these values is crucial for identifying abnormal blood pressure and setting blood pressure targets.
- SYS reflects the force when your heart contracts to push blood out, ideally below 130 mmHg.
- DIA indicates the pressure when your heart is at rest, ideally below 90 mmHg.
Pulse rate monitoring, the count of your heartbeats per minute, also provides important health data. Accurate measurement techniques and regular consultation with a doctor are essential.
Understanding these fundamentals empowers you to monitor your health effectively and contribute positively to others' well-being.
Significance of Monitoring Pulse Rate
While you're keeping track of your SYS and DIA readings, it's equally important to monitor your pulse rate as it gives additional crucial health data. Regular monitoring frequency can reveal long term effects on your health. High pulse rates can indicate risk factors for kidney disease and hypertension.
| Pulse Rate | Interpretation | Potential Actions |
| Below 60 bpm | May indicate a slow heartbeat | Consult a healthcare professional |
| 60-100 bpm | Generally healthy | Maintain lifestyle modifications |
| Above 100 bpm | May indicate a fast heartbeat | Explore treatment options |
Consultation With a Doctor for Blood Pressure Targets
Engaging in consultation with your doctor about blood pressure targets is an integral part of managing hypertension and associated kidney disease, even preventing end-stage kidney disease.
This process allows for the tailoring of individual blood pressure targets, thus providing a personalized approach to your health.
Regular check-ins with your doctor are also crucial, enabling the tracking of progress and necessary adjustments in your blood pressure management strategy.
Tailoring Individual Blood Pressure Targets
To manage your high blood pressure effectively, it's crucial to establish individual blood pressure targets through a consultation with your doctor. This process involves tailoring blood pressure targets, forming a personalized management approach, and developing individualized treatment plans to meet your specific needs. Your customized blood pressure goals will depend on various factors such as age, overall health status, and presence of other medical conditions.
In your personalized hypertension management:
- Your doctor will assess your current health status and your risk for cardiovascular disease.
- They'll consider the potential benefits and risks of different blood pressure targets.
- They'll look at your lifestyle habits, including diet and physical activity.
- They'll adjust your treatment plan as needed, based on your progress and any side effects from medications.
Tracking Progress and Adjustments in Blood Pressure Management
In managing your high blood pressure, it's crucial to regularly consult with your doctor for tracking progress and making necessary adjustments in your treatment plan. This will include medication adjustments, lifestyle modifications, stress management techniques, and dietary recommendations.
| Tracking Progress | Adjustments in Management |
| Regular consultations with your doctor | Medication adjustments as needed |
| Monitoring blood pressure at home | Emphasizing lifestyle modifications |
| Recording fluctuations in blood pressure | Incorporating stress management techniques |
| Reporting any unusual symptoms or side effects | Following dietary recommendations |
| Assessing the impact of changes on kidney health | Re-evaluating the plan regularly |
Reporting Blood Pressure Measurements
As you navigate your journey with high blood pressure and kidney disease, it's essential to become adept at reporting your blood pressure measurements accurately. Your focus on effective recording techniques at home and meticulous documentation of measurements can greatly aid in managing your condition.
Effective Recording Techniques for Home Monitoring
Maintaining accurate blood pressure records for future consultations involves various methods ensuring consistency and accessibility.
A dedicated notebook allows handwritten entries, noting readings, date, time, and any accompanying factors. Digital apps or spreadsheets offer convenience, enabling easy updates, trend analysis, and even reminders for measurements. Photographing readings with date and time displayed on the device provides visual documentation.
Whichever method chosen, consistency is key. Ensure legibility, accurate data entry, and a standardized format across recordings. Syncing digital records or storing photos in a secure location aids easy retrieval during consultations.
Choose a method that suits individual preferences and lifestyles, ensuring regular updates and sharing these comprehensive records with healthcare professionals, facilitating informed discussions, treatment adjustments, and tailored interventions based on the documented trends or patterns.
The Importance of Accurate Measurement Documentation
Accurate measurement documentation of blood pressure in CKD patients is pivotal for several reasons.
Firstly, hypertension is a common comorbidity in CKD and a significant contributor to its progression. Precise records establish trends, aiding in treatment assessment and adjustments.
Secondly, CKD often involves multiple medications; tracking blood pressure readings ensures medication efficacy and identifies potential adverse effects.
Thirdly, consistent documentation allows healthcare providers to assess the risk of cardiovascular events, shortness of breath, and chest pain, which are prevalent complications in CKD.
Moreover, accurate records facilitate personalized treatment plans, promoting optimal blood pressure control tailored to individual patient needs. It enables timely interventions, potentially preventing complications and slowing CKD progression.
Finally, documentation supports collaborative decision-making between patients and healthcare professionals, fostering proactive management and enhancing overall kidney health in CKD patients.
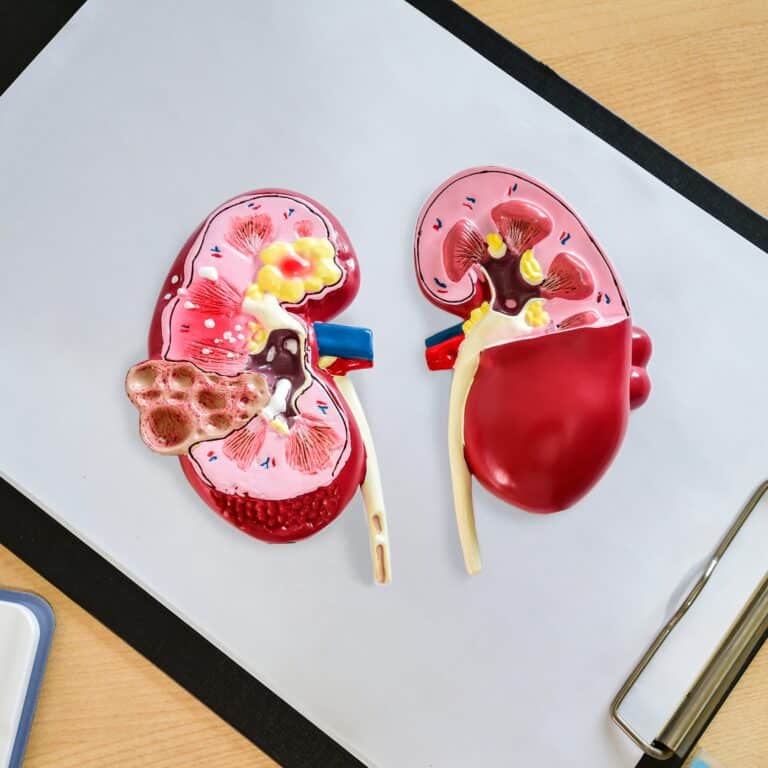
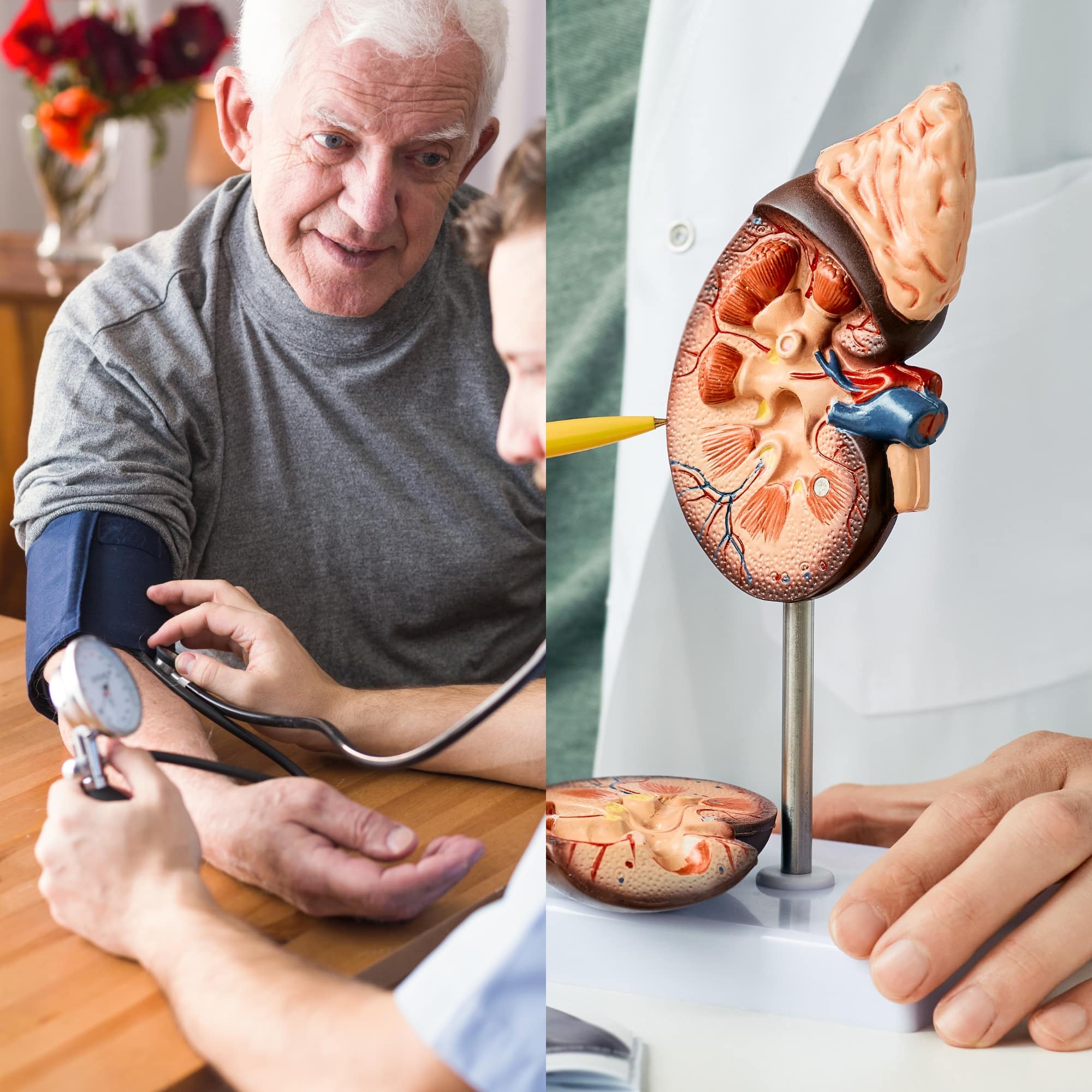
Understanding High Blood Pressure and Kidney Function
You need to understand that high blood pressure, or hypertension, exerts excessive force on your blood vessels, including those in your kidneys. This pressure can constrict and damage these vessels, impairing your kidneys' ability to filter waste from your blood.
Conversely, your kidneys play a vital role in regulating your blood pressure, creating a complex, interconnected relationship between these two critical health factors.
Investigating the Influence of Blood Pressure on Kidney Function
High blood pressure (hypertension) critically affects kidney function through several mechanisms. The sustained high pressure in the blood vessels leading to the kidneys causes damage to the delicate structures within the kidneys over time.
It specifically impacts the tiny blood vessels (glomeruli) responsible for filtering waste and excess fluid from the blood. The increased pressure strains these vessels, impairing their ability to function properly. Moreover, hypertension induces structural changes in the kidneys, leading to a reduction in blood flow.
This diminishes the kidneys' capacity to filter waste efficiently, causing a gradual decline in kidney function. Long-standing hypertension contributes to the development and exacerbation of conditions like diabetic nephropathy or glomerulonephritis, further escalating kidney damage.
The chronic strain imposed by high blood pressure accelerates the progression of chronic kidney disease, elevating the risk of kidney failure if hypertension remains uncontrolled.
Acknowledging the Role of Kidneys in Blood Pressure Regulation
The kidneys play a pivotal role in regulating blood pressure through various mechanisms. They manage blood pressure by controlling the body's fluid volume and maintaining a delicate balance of electrolytes.
Renin, an enzyme released by the kidneys, initiates a cascade that ultimately leads to the production of angiotensin II, a potent vasoconstrictor. This hormone prompts blood vessel constriction, elevating blood pressure. The kidneys also influence blood pressure by regulating sodium levels. Sodium retention can increase blood volume, raising pressure within the vessels.
Conversely, the kidneys respond to changes in blood pressure. They adjust the volume of urine produced, either conserving or expelling more fluids to maintain equilibrium. Additionally, they help regulate blood pressure by filtering blood through the glomeruli, influencing the body's overall fluid and electrolyte balance.
Disruptions in these intricate processes due to kidney damage or disease can lead to hypertension, creating a feedback loop where high blood pressure can further damage the kidneys, perpetuating the cycle of dysfunction.
Complications on Kidney Health and Beyond
Let us take a look at hypertension's far-reaching effects on both kidney health and systemic complications. Within this section, delve into the intricate relationship between high blood pressure and renal function, as well as its broader impact on various bodily systems. We will uncover the multifaceted implications of hypertension, unraveling its complex manifestations beyond the kidneys and into the broader landscape of health complications.
Complications of High Blood Pressure
Hypertension's impact extends beyond the kidneys, affecting various organs. Here's an overview:
| Body System | Complications |
| Cardiovascular | Increased risk of heart disease, stroke, and heart failure due to arterial damage and increased workload on the heart. |
| Brain | Greater susceptibility to stroke and cognitive impairment caused by reduced blood flow or hemorrhage. |
| Eyes | Vision problems or vision loss due to damage to blood vessels in the eyes (retinopathy). |
| Vascular System | Aneurysms, peripheral arterial disease, and endothelial dysfunction, which can lead to poor circulation. |
| Kidneys | Chronic kidney disease (CKD), renal artery stenosis, and reduced kidney function due to vascular damage. |
| Nervous System | Higher risk of dementia or cognitive decline. Elevated blood pressure affects brain health and neural function. |
These complications emphasize the systemic impact of hypertension, underscoring the necessity of managing blood pressure to mitigate its adverse effects on multiple bodily systems.
Analysis of the Feedback Loop Between Hypertension and Increased Kidney Pressure
Hypertension and kidney disease often fuel a relentless cycle. High blood pressure strains delicate kidney structures, impairing their function over time. Damaged kidneys struggle to regulate blood pressure effectively, causing it to rise further. This cyclical relationship compounds the risk of complications.
As hypertension persists, it damages blood vessels in the kidneys, reducing their ability to filter waste and excess fluid. The kidneys respond by retaining sodium and water, elevating blood pressure. This continual strain on the kidneys leads to chronic kidney disease, further exacerbating hypertension.
Complications arise from this intertwined relationship: increased protein in urine, electrolyte imbalances, and reduced urine output. CKD can progress to end-stage renal disease (ESRD), necessitating dialysis or transplant.
Additionally, this heightened strain on the cardiovascular system heightens the risk of heart disease, stroke, and ultimately raises the risk of mortality. Managing hypertension and kidney disease is crucial to break this detrimental cycle.

Prevalence of Hypertension and Kidney Disease
You might be surprised to learn that nearly half of U.S. adults (48.1%, 119.9 million),suffer from high blood pressure.
This condition, in turn, significantly impacts kidney health, with more than 37 million American adults possibly living with chronic kidney disease (CKD).
It's crucial to note that hypertension is the second leading cause of kidney failure in the country, following diabetes.
Examination of Current Statistics on Hypertension and CKD Prevalence
Hypertension stands as a critical health concern, contributing significantly to mortality rates in the United States.
In 2021, it was a primary or contributing factor in 691,095 deaths, highlighting its association with fatal conditions like heart disease and stroke. Alarmingly, nearly half of adults, around 119.9 million individuals, grapple with hypertension.
However, only 22.5% have their hypertension under control, leaving a staggering 37 million adults with uncontrolled high blood pressure, many with readings at or exceeding 140/90 mmHg.
Coupled with this, kidney diseases, often linked to uncontrolled hypertension, pose a substantial health burden. An estimated 37 million adults suffer from chronic kidney disease, with a startling 40% unaware of their condition.
Kidney failure rates reflect this crisis, with 360 people beginning dialysis treatment daily. Diabetes and high blood pressure, together, account for three-quarters of new kidney failure cases in the US.
These statistics underscore the interconnectedness of hypertension and CKD, emphasizing the urgent need for comprehensive awareness, early detection, and effective management to curb the escalating prevalence of these life-threatening conditions.
Identification and Discussion of Risk Factors for CKD
Understanding your risk factors for chronic kidney disease (CKD) is crucial, particularly given the prevalence of hypertension and kidney disease. The impact of lifestyle choices, genetics, and the importance of early detection all play a role in CKD.
| Risk Factors | Description | Prevention Strategies |
| Hypertension | Persistent high blood pressure | Regular exercise, healthy diet, limiting alcohol |
| Diabetes | High blood sugar over a long period | Regular checkups, diet control, exercise |
| Family History | Relatives with kidney disease | Regular screening, lifestyle changes |
| Age | Being over 60 years old | Regular health checkups |
| Ethnicity | African American, Asian, Hispanic, Indigenous | Regular screening, control of other risk factors |
These risk factors underline the importance of early detection and lifestyle changes for prevention. Understanding and managing these can significantly reduce your risk of developing CKD.
Prevention Strategies for Kidney Disease Stemming From Hypertension
To prevent kidney disease spurred by hypertension, it's crucial you consider both lifestyle modifications and medications.
Evaluating how changes in your daily habits influence your blood pressure and kidney health is an essential first step.
Concurrently, understanding the role of medications in preventing hypertension-related kidney damage will provide a comprehensive approach to your health management.
Evaluation of Lifestyle Modifications on Hypertension and Kidney Health
You can significantly improve your kidney health and manage hypertension by adopting various lifestyle modifications, which are crucial prevention strategies against kidney disease caused by high blood pressure.
Let's evaluate these lifestyle changes:
- Exercise: Regular physical activity lowers blood pressure and boosts kidney health. The benefits of exercise are significant and undeniable.
- Stress management: High stress levels can spike your blood pressure. Mindfulness and relaxation techniques help keep it under control.
- Weight loss: Shedding excess pounds has a positive effect on blood pressure, making weight management a key strategy.
- Dietary changes: Reducing sodium intake is vital for kidney health. It also helps manage hypertension effectively.
Review of Medications Used in the Prevention of Hypertension-Related Kidney Damage
Various blood pressure medications effectively manage blood pressure, mitigating the risk of hypertension-induced chronic kidney disease.
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are pivotal in controlling blood pressure and protecting kidney function. ACE inhibitors, like Lisinopril or Enalapril, hinder the production of angiotensin II, a potent vasoconstrictor, thereby dilating blood vessels and reducing blood pressure. ARBs, such as Losartan or Valsartan, function by blocking the action of angiotensin II on the blood vessels, resulting in relaxation and lowered blood pressure.
Calcium channel blockers (CCBs) like Amlodipine or Diltiazem relax and widen arteries, lessening the pressure against their walls. Diuretics, such as Hydrochlorothiazide, help the kidneys remove sodium and water, reducing blood volume and subsequently blood pressure. Beta-blockers, like Metoprolol or Atenolol, reduce the heart rate, lessening the heart's workload and decreasing blood pressure.
Combining medications or adjusting dosages based on individual needs is common practice to achieve optimal blood pressure control, thereby significantly reducing the risk of hypertension-related kidney damage and the onset or progression of CKD. Regular monitoring by healthcare professionals ensures the effectiveness and safety of these medications.
Lifestyle and Dietary Recommendations for Maintaining Kidney Health
Adopting the right lifestyle habits and dietary choices can make a significant difference in maintaining your kidney health. Lifestyle modifications and dietary recommendations include exercise benefits, stress management, and medication options.
Exercise regularly to maintain a healthy body weight. Regular physical activity can help control blood pressure levels and reduce the risk of chronic kidney disease.
Manage stress through relaxation techniques such as meditation, yoga, or deep breathing exercises. High stress levels can elevate blood pressure, negatively affecting kidney health.
Follow a balanced diet that's low in sodium and high in fruits and vegetables. This can help control blood pressure and thus, protect your kidneys.
Consider medication options if lifestyle changes aren't enough to control your blood pressure. Always consult your healthcare provider for the best treatment plan.
Comprehensive Guidelines for Kidney-Friendly Eating Habits
In maintaining your kidney health, the right dietary habits play an integral role, so let's delve into some comprehensive guidelines for kidney-friendly eating.
Firstly, limit your sodium intake. Excessive sodium can raise blood pressure, which is harmful to your kidneys. Aim for less than 2,300 milligrams per day. This means avoiding high-sodium foods like canned soups, fast food, and processed meats.
Next, regulate your protein consumption. While essential for body functions, excessive protein can burden your kidneys. It's advised to incorporate lean proteins, such as fish and poultry, in moderate quantities.
Thirdly, monitor your potassium and phosphorus levels. High amounts can cause issues for those with kidney disease, so it's crucial to keep intake in check. Opt for low-potassium foods like apples and berries, and avoid high-phosphorus foods like dairy and nuts.
Lastly, maintain a healthy weight through balanced eating. Obesity can lead to high blood pressure and diabetes, both risk factors for kidney disease. Implement a diet rich in fruits, vegetables, whole grains, and lean proteins.
Overview of Stress Management Techniques to Support Kidney Health
Dealing with high blood pressure and kidney disease, it's crucial that you're familiar with stress management techniques to support your overall kidney health. Chronic stress can aggravate your blood pressure levels, further straining your kidneys. Hence, learning effective coping strategies becomes essential.
To start, consider these four stress management techniques:
- Mindfulness Practices: Paying attention to the present moment without judgment can help you manage stress. Mindfulness-based stress reduction (MBSR) is a structured program that combines mindfulness meditation and yoga.
- Physical Activity: Regular exercise lowers stress hormones and helps you feel more relaxed and positive.
- Relaxation Methods: Techniques such as deep breathing, progressive muscle relaxation, and guided imagery can ease stress.
- Social Connection: Strengthening relationships and seeking support from loved ones can provide emotional relief and stress resiliency.
Adopting these coping strategies can significantly bolster your kidney health support. Over time, you'll notice improvements in your stress levels and overall health.
Frequently Asked Questions
Early signs of kidney disease due to high blood pressure may include persistent fatigue, trouble sleeping, decreased appetite, and muscle cramps. Additionally, experiencing difficulty concentrating, swelling in the feet or ankles, increased urination, or changes in urine frequency or color could indicate kidney involvement. High blood pressure often remains asymptomatic, underscoring the importance of regular check-ups to detect kidney-related issues early.
A family history of hypertension or kidney disease elevates an individual's risk due to genetic predispositions. Inherited traits may lead to a higher susceptibility to hypertension, kidney-related conditions, or impaired kidney function. Shared lifestyle habits and environmental factors within families also contribute. Understanding familial health history allows early monitoring and lifestyle adjustments, aiding in the prevention or early detection of hypertension and kidney-related issues in at-risk individuals. Regular screenings and lifestyle modifications become crucial in managing this increased risk.
Yes, doctors employ various tests to detect kidney damage caused by hypertension. These include blood tests to assess kidney function by measuring creatinine, blood urea nitrogen (BUN), and glomerular filtration rate (GFR). Urine tests examine protein levels, an indicator of kidney damage. Imaging tests like ultrasounds or MRIs visualize kidney structure, identifying abnormalities. Additionally, renal biopsies may be necessary in severe cases to examine kidney tissue for specific damage linked to hypertension. Regular monitoring with these tests aids in detecting and managing kidney damage due to hypertension.
High blood pressure exacerbates existing kidney disease by increasing strain on fragile blood vessels in the kidneys. Elevated pressure damages these vessels, impairing their ability to filter waste and fluids effectively. It accelerates kidney function decline, causing protein leakage and scarring of kidney tissue. Continuously high blood pressure restricts blood flow to the kidneys, leading to reduced oxygen supply, exacerbating kidney damage. Effectively managing blood pressure is crucial in slowing the progression of kidney disease and preserving renal function.
Controlling Your Blood Pressure Protects Your Kidneys
Accurate blood pressure measurement is pivotal in managing hypertension and preventing kidney disease. Discrepancies between home and clinical readings highlight the need for precise techniques. Effective measurement involves validated equipment, relaxation methods, and understanding pulse rate dynamics. Accurate documentation, whether in a notebook or app, is vital for future consultations.
High blood pressure creates a detrimental cycle damaging kidneys and exacerbating hypertension. This relationship emphasizes the kidneys' role in blood pressure regulation. Complications extend beyond kidneys, affecting cardiovascular and nervous systems, emphasizing hypertension's systemic consequences.
Prevalence statistics reveal millions affected by hypertension and kidney disease. Medications and lifestyle changes are vital in managing hypertension. Accurate reporting of blood pressure aids tailored treatments. Awareness, early detection, and proactive management are crucial. Adopting kidney-friendly habits and stress management techniques can help break the cycle of hypertension and kidney disease, empowering individuals to take control of their health.