Kidney Doctor: What Is A Nephrologist?
A nephrologist is a medical doctor who specializes in kidney health and diseases. They are trained to diagnose, treat, and manage conditions related to the kidneys such as high blood pressure, kidney stones, chronic kidney disease, acute renal failure, and end-stage renal disease (ESRD).

Nephrologists also work with other doctors (like your internal medicine doctor) to provide care for patients with complex medical issues that involve their kidneys. With their expertise, they can help people suffering from kidney problems lead healthy lives.
Jump to:
- What Type Of Doctor Treats Kidney Disease?
- What Is The Difference Between A Nephrologist And A Urologist?
- Another Name For Kidney Doctor
- What Kind Of Doctor Treats Kidney Disease
- Kidney Biopsy
- When Should I See A Nephrologist?
- Working With Other Medical Professionals
- Common Questions About Kidney Doctors
- The Nephrologist: Your Kidney Doctor
Nephrology or Renal Medicine requires extensive training and experience beyond what most general physicians possess; therefore it's important to know how a kidney specialist differs from a regular doctor so one can make informed decisions about treatment options when it comes to kidney health.
In this article we will explore what exactly makes a nephrologist different from other types of physicians, as well as discuss why someone might need specialized care from these experts.
What Type Of Doctor Treats Kidney Disease?
Nephrologists are medical professionals who specialize in diagnosing and treating kidney diseases. From providing positive lifestyle changes to utilizing gene testing, nephrologists offer comprehensive care for those suffering from chronic kidney conditions. Through the implementation of treatments such as kidney nutrition, hydration therapy, and medical management, a nephrologist can help their patients live healthier lives.
In addition to helping people manage existing health issues related to their kidneys, nephrologists also provide preventative advice on how to maintain good renal health. If you're concerned about your risk for developing a kidney disease or have family members with a history of one, it may be beneficial to consult with a nephrologist who can assess your situation and recommend preventive measures that could lower your chances of getting sick.
Nephrologists often prescribe medications specifically tailored towards improving overall renal function as well as make dietary recommendations that focus on reducing strain on the kidneys. For those already living with an advanced stage of kidney illness, seeing a nephrologist regularly is essential when it comes to managing symptoms, understanding prognosis and exploring available treatment options.
A specialized doctor will identify any underlying conditions contributing to the condition while working together with other healthcare practitioners like dieticians and physical therapists to create personalized strategies designed to improve patient quality of life.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
What Is The Difference Between A Nephrologist And A Urologist?
Nephrologists and urologists have different educational backgrounds, as nephrologists have specialized training in kidney diseases and urologists typically focus on urinary tract issues.
Both specializations have different sets of procedures they are qualified to perform, such as nephrologists performing kidney biopsies and urologists performing bladder surgeries.
Nephrologists often focus on diagnosing and treating complex kidney diseases, such as renal failure, kidney infections, nephrotic syndrome, vascular disorders, diabetic nephropathy, and autoimmune diseases, whereas urologists specialize in issues like kidney stones, prostate enlargement, or urinary tract infections.
Nephrologists also focus on understanding how kidney diseases interact with other medical conditions, such as diabetes, whereas urologists are typically experts in performing a wide range of procedures, including surgery.
Both specialties play important roles in diagnosing and treating kidney and urinary tract issues, but their respective specializations and procedures vary.
Education
A nephrologist is a medical doctor who specializes in the diagnosis and treatment of kidney diseases. Nephrologists are trained to diagnose illnesses related to kidneys using blood tests, dietary changes, exercise habits, and medication management. When compared to urologists, they often focus more on preventing or managing chronic medical conditions rather than performing surgical procedures.
Nephrologists take an active role in the prevention and management of kidney-related issues by providing patient education about lifestyle choices that can lead to healthy outcomes, like reviewing your smart goals for chronic kidney disease. They work closely with other healthcare professionals such as dietitians and physical therapists to coordinate treatments which involve dietary changes, exercise habits for a healthy heart, and medication management.
In addition to their preventive care duties, nephrologists also interpret diagnostic testing including urine analysis, imaging studies like CT scans or MRI’s, and understanding specialized lab tests for assessing the electrolyte balance in the body's system to better understand the current renal condition of the patient.
With these tools at hand, they are able to detect any abnormalities associated with renal function before it becomes severe enough to cause life-threatening consequences.
To become a nephrologist in the United States, one must go through a lot of training. After obtaining a medical degree, the doctor must undergo Internal Medicine training for three years. After which, one will undergo a two to three-year fellowship in Nephrology to be a specialist in this field.
Specializations
Apart from being a specialist in care of patients with kidney disease, especially chronic kidney disease, some nephrologists have sub-specializations that make them experts in a narrower line of kidney diseases. Some subspecialists include:
- Onconephrologist (cancer-related conditions e.g., kidney cancer)
- Critical care nephrologist
- Dialysis nephrologist (For Home Hemodialysis or In Center Dialysis)
- Interventional nephrologist (procedures)
- Kidney Transplantation Specialist
- Pediatric nephrologist
Procedures
Nephrologists take their specialized knowledge a step further by also being competent in performing certain procedures. Aside from monitoring kidney function, creating treatment plans, managing medications and treating any complications associated with the kidneys, they can also do or assist in procedures that aid in diagnosis and treatment of renal issues. Some of these are the following:
- Ultrasound
- CT Scan
- Biopsy
- Dialysis (Hemodialysis, Peritoneal Dialysis)
- Kidney Transplant
Another Name For Kidney Doctor
Diagnosing kidney diseases requires a nephrologist, who is a specialist in kidney diseases. The first step towards a diagnosis is a medical history that looks into your symptoms, previous illnesses, as well as family's medical history.
Aside from taking a detailed history and thorough physical examination, they'll need to run a few diagnostic tests to assess your kidney function. This includes blood and urine tests, to measure how well your kidneys are working.
Imaging tests are also necessary to check for abnormalities and signs of damage. Finally, a biopsy is sometimes necessary to be able to diagnose more complex renal diseases.
Medical History and Physical Examination
Prior to any testing, doctors take into account a patient's medical history when diagnosing kidney disease.
This includes genetic predisposition, previous illnesses, lifestyle choices, and diet management. Looking at diet changes by stage of chronic kidney disease is the responsibility of the Registered Dietitian. Understanding the individual’s personal health background can give healthcare professionals an idea of how their body responds to certain treatments and medications.
Early detection is key as it allows for more effective treatment plans since chronic illnesses often have several stages. Stages of chronic kidney disease range from just below normal functioning to full-on end-stage kidney failure. By getting ahead of the progression of kidney disease, doctors are better equipped to provide personalized care that maximizes quality of life for those affected by these health conditions.
After getting a complete history and performing physical examinations, the nephrologist will be able to determine priority diagnostic tests to request for better understanding of a patient’s kidney condition.
Diagnostic Tests
It can be intimidating when someone has to consider the possibility of having kidney disease. Thankfully, there are nephrologists who can help diagnose and treat it.
They use several diagnostic tests to determine if kidney diseases are present, including blood tests, urine tests, genetic testing, ultrasound imaging and kidney scans. All these tests have unique purposes that give insight into how the kidneys function or what caused their dysfunction in the first place.
For instance, blood tests measure levels of certain substances like serum creatinine and blood urea nitrogen that indicate whether something is wrong with the kidneys. Urine tests also look for signs of infection while genetic testing can detect genetic conditions like polycystic kidney disease.
Ultrasound imaging helps identify any blockages such as tumors or stones obstructing the urinary tract while a kidney scan looks at overall functioning by measuring how well each one filters out waste products from the body.
With all this data collected, your nephrologist is better equipped to find an effective treatment plan for managing any type of kidney disease.
Kidney Function Tests
When there is suspicion of a kidney disease, nephrologists employ different types of tests to measure how well the kidneys are functioning, usually starting with an eGFR blood test. This is because treatment will vary depending on the current capacity of the kidneys.
These include urinalysis and blood tests that look for albumin levels, blood creatinine levels, as well as other common tests like blood urea nitrogen levels in order to evaluate what's happening with a patient’s renal system. For more complex cases, specialized tests that may involve nuclear medicine as determined by a nephrology specialist may be needed on top of basic blood tests.
From the results of tests, your kidney doctor can determine your creatinine clearance rate as well as glomerular filtration rate. Both of which can reflect the degree of loss of kidney function, if any.
By using these tests, doctors can get an accurate picture of impaired kidney function present so they can create targeted treatment plans tailored to each individual's needs. The results from these tests also help monitor changes over time so healthcare professionals know if the treatment is working.
What Kind Of Doctor Treats Kidney Disease
For those with kidney disease, especially end-stage renal failure, kidney doctors may prescribe a number of treatments including medications (like CKD and Diabetes medications), dialysis treatments, and kidney transplantation, depending on many factors.
Nephrologists also monitor a patient's progress to ensure that their commonly prescribed medications for CKD and interventions are effective. Additionally, they will recommend lifestyle changes to help manage a patient's kidney disease symptoms and progression. Nephrologists may also refer their patients to other specialists if they need additional treatments.

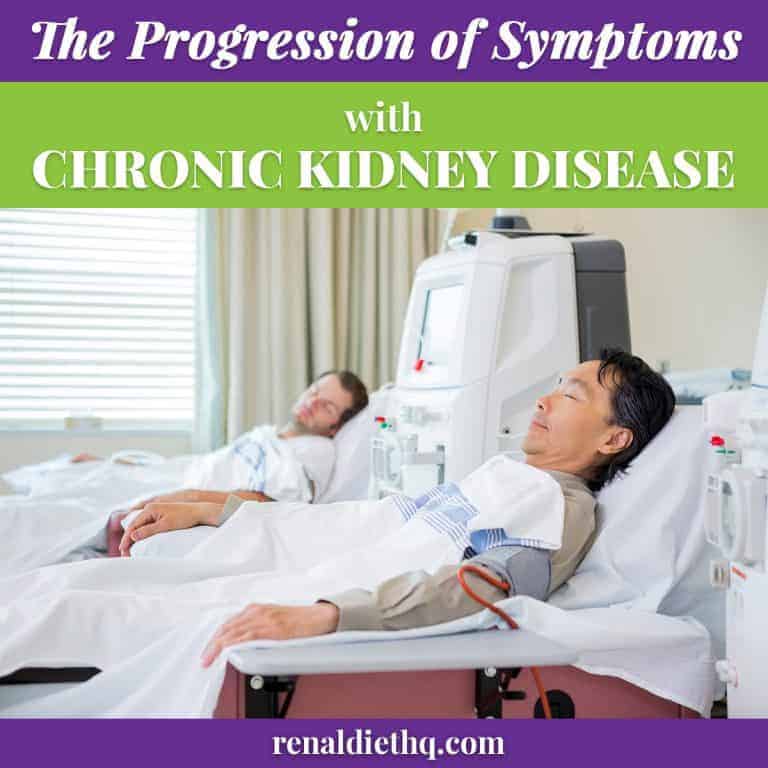
Dialysis
End-stage kidney failure is a devastating reality for so many individuals and dialysis can be the only hope for survival. Dialysis helps to maintain blood pressure, fluid intake, and kidney function when other treatments have failed. It acts as an artificial replacement of some of the functions that are normally done by healthy kidneys, allowing dialysis patients to continue living despite serious kidney damage or advanced kidney disease. With regular dialysis treatments, progression of symptoms for CKD associated with kidney failure can also improve significantly.
Dialysis is a process used to filter and remove waste from the body when kidneys are not able to do their job adequately. It can be done by either hemodialysis or peritoneal dialysis. Fluid management and hypertension control are two important aspects of successful dialysis treatment along with renal dieting that helps maintain proper nutrition while managing fluid restriction guidelines for CKD.
Dialysis also has certain side effects such as fatigue, cramping, headaches, and nausea in some people. However, these symptoms usually improve over time once patients become accustomed to the treatment regimen. Additionally, there are other medications which can help manage any discomfort associated with undergoing dialysis.
Other important aspects of dialysis include establishing an access to your blood system. This will require dialysis access insertion such as an intrajugular catheter, or in the long-term, fistula management for a more permanent access.
For patients who have no suitable donors or have other conditions that contraindicate receiving a renal transplantation, dialysis remains the mainstay of treatment for end stage kidney failure.
Successful long-term dialysis treatment requires dedication from both patient and provider, and fortunately there has been much advancement over the years which provide better care options than before, improving patient survival and quality of life. With more access to information about diet and lifestyle changes combined with dedicated healthcare teams around them, those on dialysis can look forward to being healthy for longer.
Transplantation
Transplantation is another treatment option for those suffering from kidney failure. This method involves the transfer of a donated organ, usually a kidney, to replace the failed one. Living donors make up an important part of this process, providing life-saving organs to their family or loved ones with end stage renal failure. It's an incredible gift that can provide superior outcomes over dialysis in terms of quality of life and cost effectiveness.
Nephrologists offer necessary support during this process by helping find living donors who can donate one of their kidneys, determining if potential recipients are medically suitable for a transplant procedure, and providing postoperative care following the transplant surgery. Their expertise ensures that these complex operations go smoothly so individuals can receive much needed treatment for end-stage kidney disease.
However, kidney transplant isn't always available as there are not enough suitable donors or patients may have medical contraindications that preclude considering renal transplantations. Moreover, transplant also requires immunosuppression management to prevent rejection.
Organ donation is essential for those with chronic kidney problems looking for a viable solution like transplantation. Unfortunately, due to issues on the availability of donor organs, many don't receive this potentially life-saving procedure.
To help increase these resources both nationally and globally organizations have been created to spread awareness about its importance and how individuals can become involved in donating their organs after death or even while still alive.
Medication Management
Medication management is an important part of treating kidney diseases, as it's necessary to control the underlying condition and manage any complications. Most patients will need medications to control high blood pressure or to prevent electrolyte disturbance.
Other medications include drugs for diabetes and cardiac medications such as blood thinners for those with heart disease. This is because systemic conditions like diabetes and cardiovascular disease common conditions also seen in patients with kidney disorders.
Medications are often prescribed to reduce inflammation or block processes that cause harm in the kidneys, but also come with potential side effects like headaches, nausea, dizziness, fatigue and more.
When these symptoms of kidney disease arise, consulting with your nephrologist can help reduce your discomfort and maximize the benefits from the medications.
Lifestyle changes like regular exercise (and exercise mistakes to avoid with CKD) and dietary modifications can also help minimize these side effects while promoting overall kidney health. In addition, frequent renal tests as directed by your attending doctor should be conducted to monitor how well drugs are working for a patient's particular case. These tests provide insight into whether medications need to be adjusted or changed to keep one's kidney functioning at its best.
Ultimately, being guided by your kidney doctor on what medications to take and when will ensure patients lead healthier lives despite having a chronic disease like CKD.
Kidney Biopsy
One important diagnostic tool used by nephrologists is the kidney biopsy – so let's take a look at how they use this procedure to detect impaired kidney function and identify the best possible treatment.
A kidney biopsy involves taking small samples from the organ itself, which are then analyzed under a microscope by a pathologist. This allows researchers to get an up-close view of any abnormalities present within the tissue, allowing them to make more accurate diagnoses about a patient’s condition.
For example, if there are signs of inflammation in the sample taken during the biopsy process, then doctors may suspect infection or other conditions like lupus or diabetes. The biopsy also helps detect cysts, tumors, blockages, and other issues that may affect one’s kidney function.
The results of these tests allow medical professionals to determine what type of treatment plan would best suit each individual case. Doctors might suggest dietary changes such as following a low sodium kidney diet or increasing water consumption; introducing medications; making lifestyle modifications like quitting smoking or increasing physical activity; undertaking surgery; or simply monitoring patients closely with regular follow-ups for early detection of future issues.
Ultimately, having access to detailed information provided by kidney biopsies gives physicians greater insight into determining how best to protect people’s long-term renal health and help them manage any existing risks before they become worse over time.
When Should I See A Nephrologist?
If you are experiencing symptoms such as fatigue, swelling, and increased or decreased urination, then you may benefit from a nephrology consult.
Risk factors for needing to see a nephrologist include having a family history of kidney disease, high blood pressure, diabetes, and obesity.
If you have any of these risk factors, it's best to consult a primary care physician to determine if you should see a nephrologist.
Symptoms
If you are experiencing any of the following in this list of symptoms, it's important to make an appointment with a nephrologist:
- fluid retention that causes swelling in your hands and feet
- edema symptoms such as puffiness around your eyes
- high blood pressure that doesn't respond to medication
- proteinuria which is when proteins show up in urine tests
These can be indicators of chronic kidney disease (CKD), renal failure, or other related disorders. It's also wise to see a nephrologist if you have any family history of CKD, experience frequent urination at night or feel tired all the time without explanation.
It’s key to catch these issues early before they become more serious or even lead to permanent kidney damage. Seeing a specialist like a nephrologist will help ensure proper diagnosis and treatment.
No matter what kind of symptoms you’re having, always consult with your primary care doctor first who may recommend further testing by a nephrologist for accurate results.
Don't ignore warning signs – getting checked out sooner rather than later could save you from greater health complications down the line.
Risk Factors
It's also important to be aware of any risk factors that could increase your chances of developing CKD or renal failure. These include smoking, diabetes, high blood pressure, and high cholesterol. If you have any of these conditions it's a good idea to get checked out by a nephrologist just in case.
Moreover, if you've already been diagnosed with one of these issues then getting monitored regularly is even more crucial.
Regular testing can help catch the onset of CKD early before the symptoms become too severe and cause kidney damage. It’s especially important for those who are at an increased risk due to their current medical condition – like diabetes or hypertension – as well as those who have family members with chronic kidney disease in their history.
Working With Other Medical Professionals
In order to prevent kidney disease, early detection, lifestyle changes, and supportive care are essential components.
In addition, it is important to seek out the help of other medical professionals who specialize in treating renal conditions. One such professional is a nephrologist who can provide advice on medications, stress management, dialysis or transplantation options for patients with chronic or acute kidney injury.
Nephrologists work closely with primary care providers like family physicians and internists to ensure that any underlying conditions affecting kidney health can be identified quickly. Additionally, they collaborate with specialists from other disciplines including renal dietitians, social workers, and mental health counselors when needed for holistic support of the patient's well-being.
By providing comprehensive treatment plans tailored to each patient’s specific needs, nephrologists always strive to achieve successful clinical outcomes and improve a patient’s quality life.
For individuals at risk of developing kidney disease due to genetic predisposition or environmental factors like diabetes or hypertension, seeking proactive advice from a nephrologist should not be overlooked.
Early diagnosis allows for timely intervention which may include lifestyle modifications such as physical activity and weight loss goals coupled with medication adjustments if necessary; all designed to reduce further damage to the kidneys and improve overall quality of life.
Common Questions About Kidney Doctors
Nephrologists must have completed specialized training in order to practice medicine, including medical school, residency, and fellowship. They should be knowledgeable about nutrition guidelines, risk factors, diagnostic tests, and treatment plans for nephrology cases. To become a certified nephrologist it is necessary to pass an exam from the American Board of Internal Medicine. Those who are successful will earn the title ‘nephrologist’ and gain licensure in their state.
Regular kidney checkups are important for early detection of any underlying issues, as well as to ensure your lifestyle changes and diet adjustments will help you maintain good kidney health. Depending on your risk factors, such as age or family history, your nephrologist may recommend having a monitoring test done every year or two to keep track of your kidney function.
By doing this regularly, it can also alert them to possible problems that could arise in the future so they can be treated quickly before they become more serious.
When it comes to preventing kidney damage, making lifestyle changes can be beneficial. Eating a balanced diet and knowing what foods to avoid with kidney disease like those that are high in sodium, fat, cholesterol, and sugar is key for keeping your kidneys healthy.
Increasing physical activity through exercise or other forms of movement can also help reduce the risk of developing kidney disease. Additionally, monitoring your blood pressure and drinking plenty of water throughout the day can help maintain strong kidney function.
By implementing these habits into your daily routine, you may be able to prevent any serious kidney damage.
The Nephrologist: Your Kidney Doctor
A nephrologist is a highly qualified physician trained in the diagnosis and treatment of kidney disease. As the kidney is a vital organ for bodily functions, their work can make a huge difference in people's lives.
It's ironic that although we depend so heavily on our kidneys for health, many of us don't think about them until there's something wrong. By being proactive with regular check-ups and healthy lifestyle changes, you can take control of your own kidney health. Even with kidney disease, you can still live a full life under the care and guidance of your trusted nephrologist.