Kidney Disease Treatment Diet
So, you have been diagnosed with kidney disease…now what? Treatment should begin right away to reduce symptoms and assist with slowing the progression of kidney function decline. The ways in which your kidney disease is treated will depend on the stage of the disease and your current kidney health.
Some types of kidney disease, if detected early on, can be treated. Your kidneys may regain optimal function once the cause has been found and treatment has begun. An example of this would be stopping medication that could be harming your kidneys.
For chronic kidney disease (CKD), however, the decline in kidney health has progressed over years and has likely caused damage that cannot be reversed. Currently, there is no cure for CKD. Still, treatment is very important to help slow the progression of this condition.
Jump to:
- Key Takeaways
- Understanding Chronic Kidney Disease and Treatment Options
- Exploring Natural Treatment Alternatives for Kidney Disease
- The Significance of a Comprehensive Treatment Plan in Managing Kidney Disease
- Key Facts About Kidney Disease and Its Management
- The Role of Sodium in Kidney Disease Treatment Diet
- Choosing the Right Protein Sources in a Kidney Disease Treatment Diet
- Heart-Healthy Cooking Techniques and Food Selections for Kidney Disease Patients
- The Importance of Monitoring Phosphorus Intake in Kidney Disease Treatment Diet
- Managing Potassium Levels in a Kidney Disease Treatment Diet
- Frequently Asked Questions
- Diet is Central in CKD Treatment
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Key Takeaways
- Sodium control is important in the kidney disease treatment diet.
- Balancing animal and plant proteins is essential in the kidney disease treatment diet.
- Monitoring phosphorus and potassium intake is crucial in the kidney disease treatment diet.
- Fluid management is a key aspect of the kidney disease treatment diet.
Understanding Chronic Kidney Disease and Treatment Options
You need to understand that chronic kidney disease is a long-term condition that can be managed but not cured.
There are several treatment options available, ranging from medication to dialysis and even kidney transplant. In addition to these medical interventions, a kidney-friendly diet can play a crucial role in managing your symptoms and slowing the progression of the disease.
Kidney Disease Treatment Methods
Chronic Kidney Disease management involves various approaches. Medications aim to address underlying causes and manage complications. ACE inhibitors or ARBs control blood pressure and protect the kidneys. Phosphate binders, erythropoietin-stimulating agents, and iron supplements manage mineral and anemia imbalances. Diet adjustments, particularly limiting sodium and protein, are crucial.
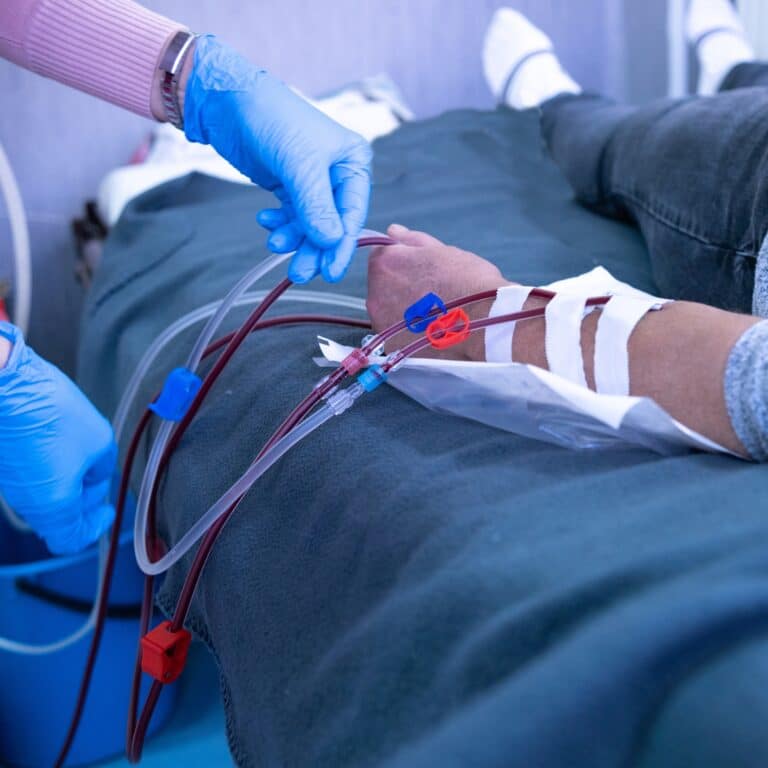
Renal replacement therapies become necessary in advanced CKD stages. Dialysis, including hemodialysis and peritoneal dialysis, filters waste and excess fluids from the blood, substituting some kidney functions.
Kidney transplantation is considered the most effective treatment, offering a better quality of life and improved longevity compared to dialysis. A donor kidney replaces the failing kidney, restoring most kidney functions. However, transplantation requires lifelong immunosuppressive medications to prevent rejection.
Each treatment has its considerations, benefits, and limitations. The choice depends on individual health, preferences, and stage of CKD. Ongoing monitoring, medication adherence, and lifestyle adjustments are vital components in managing CKD effectively.
Kidney Diet as a Treatment Option
A plan with renal diet restrictions is a cornerstone in managing Chronic Kidney Disease, focusing on nutrient control to alleviate strain on the kidneys. It aims to minimize waste buildup while maintaining essential nutrients. Key aspects include limiting sodium, potassium, phosphorus, and protein intake to ease kidney workload and manage complications.
Sodium restriction helps control blood pressure and fluid retention. Potassium moderation prevents heart rhythm abnormalities. Phosphorus management prevents bone and heart complications. Controlling protein intake reduces waste buildup, lessening the kidneys' burden.
This special diet prioritizes high-quality, low-impact foods like fruits, vegetables, grains, and limited portions of lean protein sources. Balancing nutritional needs with dietary restrictions requires meticulous planning. Regular monitoring by healthcare professionals ensures nutritional adequacy while managing CKD progression. Personalized adjustments cater to individual health status and kidney function, emphasizing the diet's crucial role in CKD management.

Exploring Natural Treatment Alternatives for Kidney Disease
Several natural treatments can complement traditional CKD management:
- Herbal Remedies: Some herbs like dandelion root and nettle leaf may have diuretic properties, aiding in fluid balance. However, caution is crucial due to potential interactions with medications and varying effects on individuals.
- Omega-3 Fatty Acids: Found in fish oil supplements or certain seeds (flaxseeds, chia seeds), omega-3s may reduce inflammation and cardiovascular risk factors associated with CKD.
- Probiotics: These beneficial bacteria promote gut health, potentially reducing uremic toxins in people with kidney disease. Yogurt and fermented foods are natural sources.
- Acupuncture and Massage: Complementary therapies like acupuncture or massage therapy may alleviate symptoms like pain, stress, or fatigue associated with CKD.
- Dietary Modifications: Incorporating anti-inflammatory foods (turmeric, ginger), antioxidant-rich fruits and vegetables, and maintaining hydration can support kidney health.
While these adjunct therapies may offer some benefits, they should be approached cautiously and in consultation with healthcare providers. Their efficacy varies, and they should complement, not replace, standard medical treatments for CKD.
The Significance of a Comprehensive Treatment Plan in Managing Kidney Disease
Why is it crucial for you to embrace a comprehensive treatment plan when managing kidney disease? Because it's not just about popping pills. It's about treatment compliance, medication management, the importance of exercise, stress reduction, and the pivotal role of family support.
Here's a table illustrating the significance of each component:
| Component | Why it's Important | How it Helps |
| Treatment Compliance | Adherence to prescribed treatment | Improves kidney function, slows disease progression |
| Medication Management | Ensures correct medicine intake | Prevents complications, maximizes therapeutic benefits |
| Exercise Importance | Maintains physical health | Aids in blood pressure control, helps manage body weight |
| Stress Reduction | Promotes mental wellbeing | Decreases blood pressure, reduces risk of heart disease |
| Family Support | Encourages adherence to treatment | Provides emotional support, assists in treatment management |
You see, it's a holistic approach. You can't just focus on one aspect and ignore the others. It's about balancing all these elements. It's about understanding that your mental health is just as important as your physical health. It's about being disciplined with your medication and respectful of the diet restrictions. It's about integrating exercise into your daily routine.
And it's about accepting help, from healthcare professionals and loved ones alike because managing kidney disease isn't a journey you should walk alone.
Key Facts About Kidney Disease and Its Management
Undeniably, you're dealing with a complex disease when managing kidney disease, but remember, it's also manageable with the right approach and commitment. Disease progression prevention is crucial, and lifestyle modification impacts are significant. You play a pivotal role in this battle, and your choices can make a difference.
Key aspects to consider:
- Disease progression prevention: It's not just about treating the symptoms, but slowing down the disease progression. Regular check-ups, medication adherence, and early detection of complications are essential.
- Lifestyle modification impacts: Your decisions matter. A balanced, kidney-friendly diet, coupled with regular, kidney-friendly exercise routines, can have a profound impact on your health. This isn't about drastic changes, but consistent, small steps towards a healthier you.
- Exercise and Stress Management: Regular physical activity helps maintain kidney function and manage stress levels. Remember, it's not about extreme workouts but staying active and incorporating stress management techniques like meditation and deep breathing.
- Hydration's role: Keeping yourself adequately hydrated is important. However, in kidney disease, balance is key as excessive fluids can also be harmful.
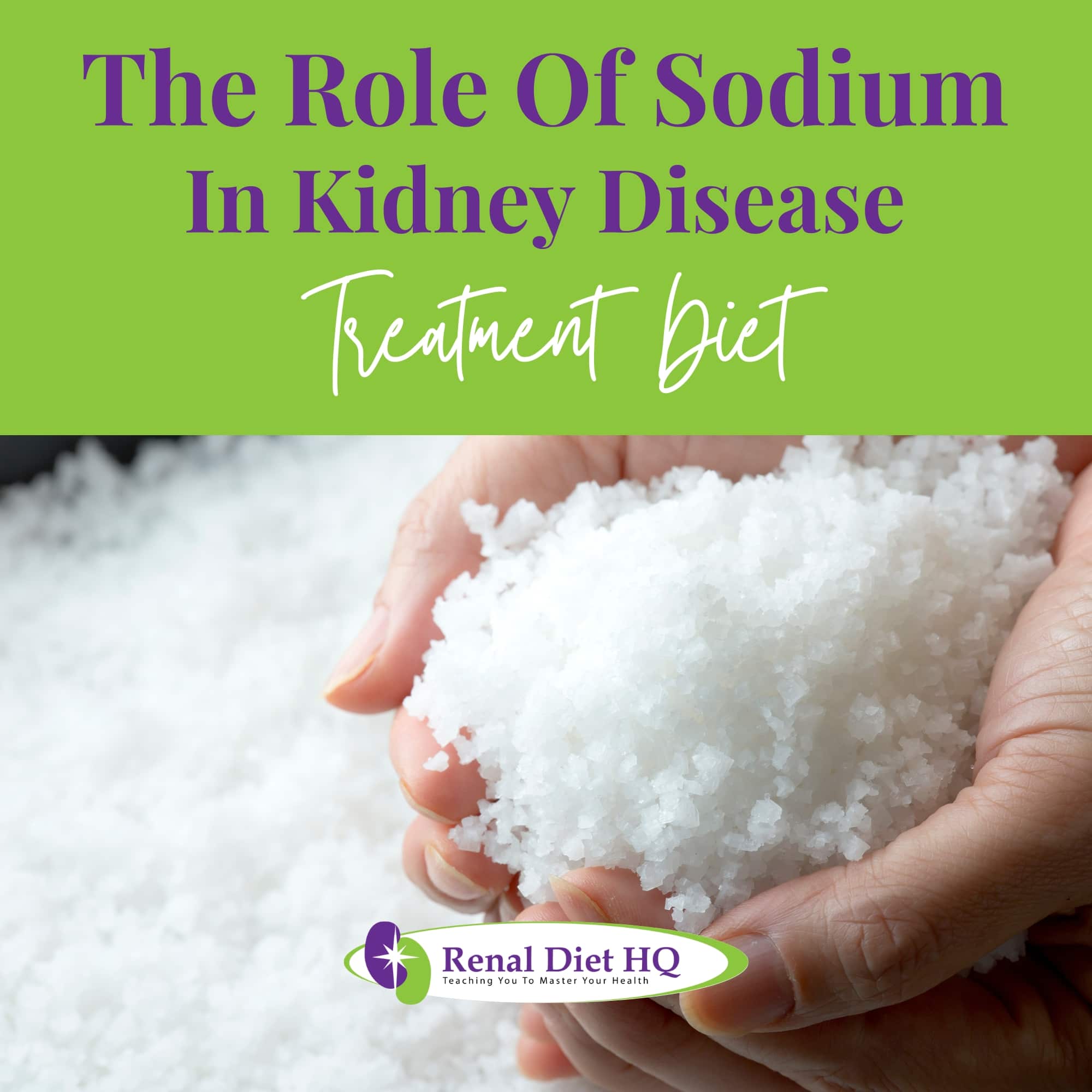
The Role of Sodium in Kidney Disease Treatment Diet
You mightn't realize how much your sodium intake impacts your kidney health.
When you have kidney disease, high sodium levels can exacerbate your condition by causing increased blood pressure and swelling.
Therefore, it's crucial to understand how reducing your sodium consumption can significantly aid in your kidney disease treatment.
Sodium's Impact on Kidneys
Sodium plays a crucial role in kidney health, but excessive intake can strain these organs. High sodium levels lead to increased fluid retention, elevating blood pressure and burdening the kidneys.
The kidneys work harder to filter excess sodium, impacting their ability to regulate fluid balance and electrolytes. This strain may accelerate kidney damage and exacerbate conditions like hypertension and CKD. Additionally, sodium can contribute to edema, causing swelling in extremities and further stressing the kidneys.
Managing sodium intake is pivotal in kidney care, as reducing salt consumption can alleviate kidney workload, regulate blood pressure, and mitigate complications associated with kidney diseases.
Reducing Sodium Intake
Renal patients can effectively reduce sodium intake through several strategies:
- Read Labels: Check food labels for sodium content and choose low-sodium or sodium-free alternatives.
- Limit Processed Foods: Avoid processed, canned, or pre-packaged foods known for high sodium content.
- Cook at Home: Prepare meals from scratch using fresh ingredients, controlling the amount of added salt.
- Use Herbs and Spices: Flavor foods with herbs, spices, citrus, or vinegar instead of salt for taste.
- Rinse Canned Foods: Rinse canned beans, vegetables, or fish to remove excess sodium.
- Moderate Salty Condiments: Minimize or avoid high-sodium condiments like soy sauce, ketchup, and dressings.
- Be Mindful Eating Out: Request dishes with less added salt when dining out or ask for sauces/dressings on the side to control intake.
These practices help renal patients manage sodium levels, supporting kidney health and reducing complications related to excessive sodium consumption.
Choosing the Right Protein Sources in a Kidney Disease Treatment Diet
When managing a kidney disease treatment diet, it's crucial for you to choose the right protein sources. You'll need to balance both animal and plant proteins, as each offers unique benefits for kidney health.
Additionally, portion control for proteins plays a vital role in preventing further kidney damage.
Balancing Animal and Plant Proteins
Balancing animal and plant protein intake is crucial in CKD. While animal proteins contain essential nutrients, they also contain higher phosphorus levels, potentially taxing compromised kidneys. Plant-based proteins offer a lower phosphorus load, easing the kidneys' burden. However, they may lack certain essential amino acids, requiring a combination of varied plant sources to ensure a complete protein profile.
Managing overall protein intake is vital. Excessive protein strains the kidneys, leading to waste buildup. Yet, inadequate protein can result in malnutrition and muscle wasting. Thus, moderation is key.
Dietitians tailor protein intake based on individual kidney function, recommending sufficient but controlled protein levels. Balancing animal and plant proteins allows essential nutrient intake while reducing phosphorus load, supporting kidney health in CKD patients. Monitoring and personalized dietary planning help optimize protein intake, supporting overall health and kidney function.
Portion Control for Proteins
Proper portion control for proteins in a renal diet is essential for managing chronic kidney disease (CKD). The kidneys, when impaired, struggle to process the byproducts of protein metabolism, making portion control vital to reduce strain. Typically, a renal diet limits protein to about 0.8 grams per kilogram of body weight per day, but this can vary based on the stage of CKD and individual health needs.
A practical approach is using visual cues: a portion of meat, fish, or poultry should be about the size of a deck of cards or the palm of the hand, equating to approximately 3 ounces. For plant-based proteins like beans or lentils, a half-cup serving is appropriate. Consulting with a kidney dietitian for personalized advice ensures that protein intake aligns with kidney health requirements while fulfilling nutritional needs.
Heart-Healthy Cooking Techniques and Food Selections for Kidney Disease Patients
Your heart health is just as important when managing kidney disease. Opting for heart-healthy food choices can help control your blood pressure and reduce fluid buildup. Additionally, using healthy cooking techniques can significantly lower your intake of unhealthy fats, sodium, and cholesterol. These factors are beneficial for both your heart and kidneys.
Selecting the right foods and cooking methods matters when managing kidney disease. Opting for heart-healthy diet choices can help control your blood pressure and reduce fluid buildup. Additionally, using healthy cooking techniques can significantly lower your intake of unhealthy fats, sodium, and cholesterol. These factors are beneficial for both your heart and kidneys.
Choosing Heart-Healthy Foods
Selecting heart-healthy foods is paramount in a renal diet to manage both kidney health and cardiovascular risk factors often associated with CKD. Optimal choices include:
- Fruits and Vegetables: Rich in antioxidants, fiber, and vitamins, they support heart health while being low in sodium and potassium.
- Whole Grains: High-fiber options like brown rice, quinoa, and whole wheat provide nutrients and promote heart health without excessive phosphorus or potassium.
- Lean Proteins: Selecting lean cuts of poultry, fish, and limited portions of red meat reduces saturated fats and cholesterol, supporting heart function.
- Healthy Fats: Incorporating sources like olive oil, avocados, and nuts in moderation provides essential fatty acids without burdening the heart.
- Limiting Sodium and Processed Foods: Reducing sodium intake and avoiding processed foods high in trans fats and unhealthy additives further supports heart and kidney health in a renal diet.
Consulting a renal dietitian ensures a balanced, heart-healthy approach tailored to individual needs.
Healthy Cooking Methods
In a CKD renal diet, heart-healthy cooking methods are crucial to support both kidney and cardiovascular health. Here are key strategies:
- Steaming and Boiling: These methods preserve the natural flavors of foods without adding unhealthy fats or excess sodium. Ideal for vegetables and lean proteins.
- Grilling and Baking: Cooking meats, fish, and vegetables by grilling or baking reduces the need for added fats while imparting a rich flavor. Using herbs and spices instead of salt enhances taste.
- Sautéing with Healthy Oils: Using olive or canola oil in small amounts for sautéing is a heart-healthy choice, as these oils are high in monounsaturated fats.
- Stir-Frying: Quick and requiring minimal oil, stir-frying vegetables and lean proteins keeps nutrients intact and limits unhealthy fat intake.
- Herbs and Spices for Flavor: Opt for fresh or dried herbs and spices over salt to flavor dishes, reducing sodium intake crucial for both heart and kidney health.
Adopting these cooking methods helps manage CKD effectively while promoting overall cardiovascular wellness.
The Importance of Monitoring Phosphorus Intake in Kidney Disease Treatment Diet
When it comes to a kidney disease treatment diet, it's crucial to keep an eye on your phosphorus intake. Packaged foods often contain high amounts of phosphorus, which can be harmful to your kidneys.
Phosphorus in Packaged Foods
You've got to keep an eye on the phosphorus content in packaged foods as part of your kidney disease treatment diet. Hidden phosphorus, often in the form of phosphorus additives, can sneak into your diet, aggravating your condition. Unfortunately, phosphorus labeling isn't always clear, making dietary phosphorus difficult to monitor.
- Phosphorus additives: You'll find these in many processed foods. Despite being necessary for normal body functions, excess levels can harm your kidneys.
- Phosphorus absorption: Your body doesn't always differentiate between dietary and additive phosphorus, leading to harmful absorption.
- Hidden phosphorus: It's not always labeled. You may consume more than you realize, straining your kidneys.
- Phosphorus labeling: Companies aren't required to list phosphorus content, making it harder to control your intake.
Regulating Phosphorus With Diet
Regulating phosphorus in a renal diet is vital due to the complications associated with high phosphorus levels in chronic kidney disease. Healthy kidneys regulate phosphorus, but in CKD, impaired kidney function can lead to phosphorus buildup in the blood. High phosphorus levels can cause serious issues, including:
- Bone and Mineral Disorders: Excess phosphorus pulls calcium from bones, weakening them and increasing the risk of fractures. It can also lead to abnormal calcium deposits in blood vessels, lungs, eyes, and heart.
- Cardiovascular Disease: High phosphorus levels contribute to the hardening and narrowing of blood vessels, increasing the risk of heart disease and stroke.
- Itchy Skin: Elevated phosphorus can cause severe itching, a common and uncomfortable symptom in CKD patients.
- Hormonal Imbalance: High phosphorus disrupts the balance of hormones like parathyroid hormone (PTH), leading to secondary hyperparathyroidism, which further exacerbates bone disease.
Therefore, regulating phosphorus intake through diet is crucial in CKD management. This includes limiting foods high in phosphorus, like dairy products, certain meats, and processed foods, and possibly using phosphate binders as prescribed by healthcare providers. This management helps slow the progression of kidney disease, reduces the risk of cardiovascular complications, and improves the overall quality of life for CKD patients.
Managing Potassium Levels in a Kidney Disease Treatment Diet
Managing your potassium levels is a crucial aspect of your kidney disease treatment diet. You'll need to familiarize yourself with potassium regulation techniques to keep levels in check.
Additionally, making low-potassium food choices can further aid in maintaining a balanced diet that supports your kidney health.
Potassium Regulation Importance
Regulating potassium in a renal diet is crucial due to potential complications associated with elevated levels in chronic kidney disease (CKD). Impaired kidney function can lead to difficulty excreting excess potassium, resulting in hyperkalemia. Complications include:
- Cardiac Arrhythmias: Elevated potassium levels can disrupt normal heart rhythm, leading to serious and potentially life-threatening arrhythmias.
- Muscle Weakness: Excess potassium affects muscle function, causing weakness or paralysis.
- Nausea and Fatigue: Elevated potassium levels can lead to symptoms such as nausea, fatigue, and numbness or tingling.
To manage potassium intake, individuals with CKD may need to limit high-potassium foods like bananas, oranges, tomatoes, and potatoes. This dietary regulation, along with medical guidance, is essential to prevent complications and maintain overall health in CKD patients.
Low-Potassium Food Choices
You'll find plenty of low-potassium food choices that are both tasty and nutritious, and they'll also help keep your potassium levels in check. Ditch potassium-rich fruits like bananas for apples, berries, and grapes. Avoid high potassium in dairy by opting for almond or rice milk.
Low potassium desserts such as blueberry muffins or apple pie can be a delight to your taste buds while managing your potassium. Hydration is crucial, but remember that even water contains potassium. Instead, try lemonade or cranberry juice.
Explore alternatives to high potassium foods. For instance, switch out high potassium foods like potatoes for sweet potatoes or squash.
With careful planning and some creativity, you can enjoy a diverse diet while managing your kidney disease.
Frequently Asked Questions
Early warning signs of kidney disease include persistent fatigue, swelling in the ankles, feet, or hands (edema), changes in urine frequency or color, difficulty concentrating, decreased appetite, and persistent itching. High blood pressure and blood in the urine can also signal kidney problems. Regular monitoring and awareness of these symptoms are crucial, prompting early medical attention to mitigate the progression of kidney disease.
Obesity or being overweight significantly increases the risk and accelerates the progression of kidney disease. Excessive weight strains the kidneys due to increased metabolic demands, leading to conditions like hypertension and diabetes, common causes of kidney damage. Fat accumulation disrupts hormonal balance, promoting inflammation and insulin resistance, further harming kidney function. Additionally, obesity heightens the risk of proteinuria and glomerular hyperfiltration, accelerating kidney decline. Weight management is crucial in mitigating kidney disease progression.
Regular exercise plays a vital role in enhancing kidney function. It helps manage weight, reducing the risk factors associated with kidney disease such as high blood pressure and diabetes. Exercise promotes cardiovascular health, improving blood flow to the kidneys and aiding in their function. It also reduces inflammation and oxidative stress, factors contributing to kidney damage. However, individuals should consult healthcare providers for exercise recommendations tailored to their specific condition and kidney health status.
Kidney disease often takes a toll on mental health, leading to anxiety, depression, and emotional distress. Coping with a chronic illness, treatment demands like dialysis or transplant, and lifestyle adjustments can cause feelings of isolation and stress. Fatigue and cognitive changes due to kidney-related complications can further affect mental well-being. Support networks, counseling, and holistic care are essential in addressing these psychological challenges and improving the overall quality of life for individuals navigating kidney disease.
Yes, a kidney disease treatment diet can aid in managing diabetes. By focusing on nutrient control, such as monitoring sodium, phosphorus, and potassium intake, the diet can align with diabetes management goals. It often emphasizes healthy eating patterns that benefit both conditions, like consuming whole grains, limiting processed foods, and moderating sugar intake. This dual-focused diet helps control blood sugar levels and reduces stress on the kidneys, benefiting individuals managing both kidney disease and diabetes.
Diet is Central in CKD Treatment
It's essential that you learn about how chronic kidney disease is treated in order to stay as healthy as you can after your diagnosis. Find out all you can about the different treatment options available to you and develop a plan for treatment with your doctor right away. Take your medication as directed to slow the disease's progression.
Treating chronic kidney disease naturally is important too, since your lifestyle can lead to further complications with the condition or related ones. Follow the renal diet you will be given and stay active to keep your body healthy.