Fluid Restrictions for Dialysis
Hydration is an important part of a healthy lifestyle, so it can be very confusing when all of a sudden things take a turn and your doctors are telling you the opposite.
Fluid restrictions (fluid restricted diet menu) can be very difficult not only to process but to follow through with. If you have been given the advice to restrict fluids, you may need more information to help you understand and follow through with this advice.
Fluid restrictions are typically only assigned to people who are entering the later stages of chronic kidney disease, meaning that these restrictions are necessary to help slow the progression to end-stage renal disease and eventual dialysis or transplant.

This article will provide you with the knowledge and tools to expertly navigate fluid restrictions for renal dialysis diet patients.
Jump to:
- Key Takeaways
- Kidneys, Dialysis, and Fluids
- Fluid Overload: Understanding and Management
- Blood Pressure and Heart Health
- Sodium Intake and Fluid Balance
- Prevention of Fluid Overload
- Individualized Fluid Management
- Fluid Maintenance Tips
- Fluid Restrictions: Effects and Challenges
- Consistency in Control
- FAQs for Fluid Restriction Guidelines
- Fluid Restriction Is Challenging, But It Is Necessary
Key Takeaways
- Fluid restrictions are vital for dialysis patients to prevent complications of fluid overload and maintain overall health.
- Understanding the role of kidneys in fluid balance and the importance of dialysis fluid removal is crucial for effective management.
- Maintaining a balance in fluid intake is important for blood pressure and heart health.
- Adherence to fluid restrictions requires ongoing patient education, lifestyle adjustments, and support systems to overcome challenges.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Kidneys, Dialysis, and Fluids
To gain a better understanding of the importance of fluid restriction, let’s look at the critical role your kidneys play in maintaining your body's delicate fluid balance. When functioning normally, they work tirelessly to filter out waste and excess fluids from your bloodstream.
However, when kidney function is compromised, dialysis steps in as a lifesaver. It does the heavy lifting by removing these wastes and surplus fluid.
Role of the Kidney
The kidneys are remarkable organs with multifaceted roles in maintaining the body's overall health. Their intricate renal anatomy and efficient functions are crucial to human physiology:
- Waste Removal: The kidneys act as natural filtration units, removing metabolic waste products like urea and creatinine from the bloodstream. This cleansing process ensures that the blood remains free of harmful toxins and waste materials.
- Fluid Regulation: These bean-shaped organs finely regulate the volume and composition of bodily fluids. By adjusting urine production, the kidneys help maintain the balance of body water, salts, and other solutes in the body. This fluid equilibrium is essential for various physiological processes.
- Hormone Production: Kidneys are not just filters; they are also endocrine glands. They produce hormones such as erythropoietin, which stimulates red blood cell production in response to low oxygen levels. Additionally, they secrete renin, a hormone that helps regulate blood pressure by controlling blood vessel constriction and fluid volume.
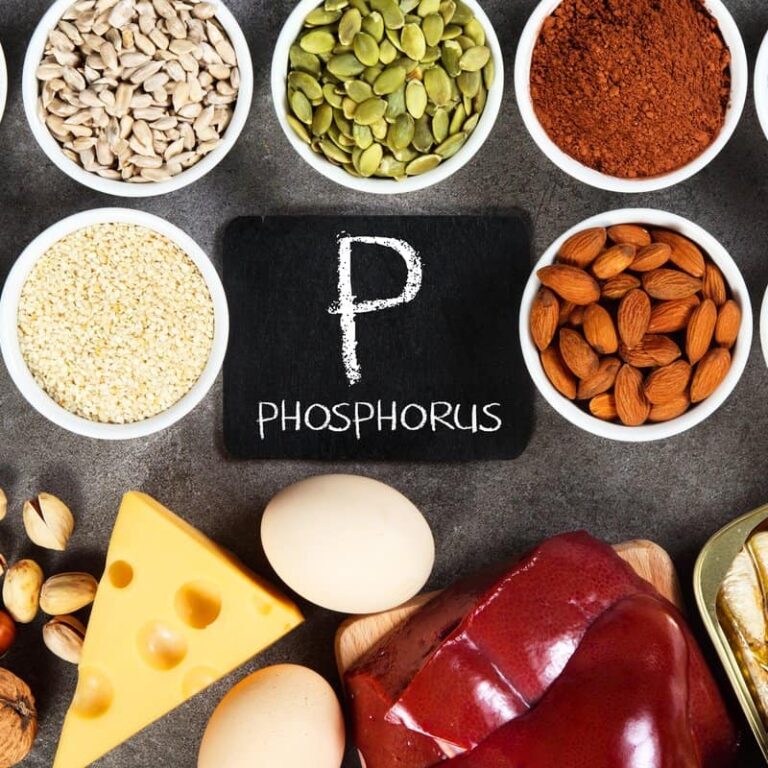
- Electrolyte Management: The kidneys play a vital role in regulating electrolyte levels, including sodium, potassium, calcium, and phosphate. These electrolytes are critical for maintaining nerve function, muscle contraction, and overall cellular health.
The kidneys' intricate functions are essential for life, making their impairment or failure a significant health concern. Understanding the roles of these organs is not only important for those undergoing dialysis but also for everyone seeking to maintain optimal health.
Knowledge of kidney function empowers individuals to make informed decisions about their diet, fluid intake, and overall lifestyle to support kidney health and prevent complications related to kidney dysfunction.
Dialysis Fluid Removal
Chronic Kidney Disease (CKD) is a progressive condition characterized by the gradual loss of kidney function over time.
As CKD advances, the kidneys' ability to filter waste products, excess fluids, and electrolytes from the blood diminishes. In its most severe form, known as End-Stage Renal Disease (ESRD), kidney function is critically compromised, often below 10-15% of normal capacity.
One of the most pressing issues in late-stage CKD and ESRD is fluid management. The kidneys play a crucial role in regulating the body's fluid balance. When their function is impaired, as in ESRD, excess fluid accumulates in the body, leading to a condition known as fluid overload.
Fluid overload has significant health implications. It can cause edema (swelling) in various body tissues, including the legs, lungs, and heart. The accumulation of fluid in the lungs, known as pulmonary edema, can be life-threatening, causing severe breathing difficulties and hypoxia.
Dialysis is the primary therapeutic intervention for ESRD patients to address fluid overload and its associated risks. Hemodialysis and peritoneal dialysis are two main modalities that effectively remove excess fluid and waste products from the body, restoring fluid balance and mitigating the risk of complications such as hypertension, congestive heart failure, and electrolyte imbalances.
Without dialysis, the consequences of fluid overload in ESRD (ESRD Prognosis) can be severe, impacting both the patient's quality of life and overall survival.
Fluid Overload: Understanding and Management
Complications arising from fluid overload are a pressing concern for individuals with late-stage Chronic Kidney Disease or End-Stage Renal Disease.
This section delves into the critical issue of fluid imbalance in CKD and ESRD patients, exploring the potentially severe complications it poses.
We will also outline key steps and strategies to prevent these complications, offering valuable insights for both patients and healthcare professionals seeking to manage fluid overload effectively in this vulnerable population. You can also check out these ckd diet guidelines.
Complications
Fluid overload in dialysis patients presents a range of complications, affecting multiple systems in the body. It can strain the cardiovascular system, leading to high blood pressure and increased cardiovascular risk.
Excessive fluid accumulation can cause congestive heart failure, impairing heart function and reducing overall cardiac efficiency. Pulmonary edema, a condition where fluid accumulates in the lungs, results in severe respiratory distress and can be life-threatening.
Peripheral edema, particularly in the legs, can cause discomfort and limit mobility. Additionally, fluid overload can disrupt the body's electrolyte balance, leading to muscle weakness, cramps, and cardiac arrhythmias.
Dialysis efficiency may also be compromised when excess fluid dilutes the concentration of waste products in the bloodstream.
Managing fluid levels through a combination of strict fluid intake control, appropriate dialysis treatment, and close monitoring by healthcare professionals is essential to prevent these complications and ensure the well-being of dialysis patients.
Intake Management
Effective fluid intake management is crucial for preventing fluid overload in individuals with Chronic Kidney Disease and those undergoing dialysis. Four key steps to manage fluid intake include:
- Monitor Daily Fluid Intake: Patients should keep a daily record of their fluid consumption, including beverages and foods with extra water content. Tracking helps maintain awareness and adherence to prescribed fluid restrictions.
- Set Individualized Limits: Healthcare providers should establish personalized fluid intake goals based on the patient's specific needs, considering factors like kidney function, urine output, and overall health.
- Choose Low-Fluid Foods: Patients can opt for foods with lower water content, like cooked vegetables or fruits, and avoid high-water-content foods like soups, ice cream, water-rich fruits, or water rich foods.
- Stay Hydrated Without Overloading: Patients should focus on staying hydrated while respecting fluid limits. This can be achieved by sipping fluids slowly, using smaller cups, and opting for ice chips or sugar-free gum to alleviate dry mouth.
These steps, when practiced diligently, can help CKD and dialysis patients manage their fluid intake effectively, reducing the risk of fluid overload and its associated complications.
Blood Pressure and Heart Health
This section delves into the significant consequences of fluid overload in patients with kidney failure, with a focus on its impact on hypertension, cardiac strain, and pulmonary congestion. We examine how the accumulation of extra fluid in these individuals can lead to severe health challenges.
Additionally, we explore essential steps and strategies for managing blood pressure, offering valuable insights into safeguarding the cardiovascular well-being of those grappling with kidney failure and its associated fluid-related complications.
Hypertension Link to Kidney Failure
Fluid overload in kidney failure can elevate blood pressure through several mechanisms.
When the kidneys lose their ability to effectively regulate fluid balance, excess fluid accumulates in the bloodstream. This surplus of fluid increases blood volume, causing higher cardiac output and subsequently raising blood pressure.
Moreover, the retained sodium, often accompanying fluid overload, exacerbates the problem as sodium attracts and holds onto water. As a result, the heart must work harder to pump blood against increased resistance, further contributing to hypertension.
Elevated blood pressure not only places added strain on the cardiovascular system but also accelerates kidney damage, creating a vicious cycle. Effectively managing fluid overload through strategies like dialysis and strict fluid intake control is essential for controlling hypertension in kidney failure patients. Here are the top 5 signs of kidney failure.
Heart Strain
Fluid overload in kidney failure, particularly in End-Stage Renal Disease, can lead to heart failure and cardiac strain due to the intricate interplay between the cardiovascular and renal systems. When the kidneys lose their ability to efficiently regulate fluid balance, excess fluid accumulates in the bloodstream.
This surplus fluid increases blood volume, elevating blood pressure and requiring the heart to pump harder to circulate the excess. Over time, this sustained increase in cardiac workload can lead to cardiac remodeling, characterized by ventricular dilation and hypertrophy, as the heart tries to adapt. This remodeling, while initially compensatory, eventually weakens the heart's pumping capacity.
Additionally, the presence of excess fluid can extend into the lungs, causing pulmonary edema. This combination of increased cardiac workload, cardiac remodeling, and pulmonary congestion ultimately elevates the risk of heart failure, making fluid balance management vital in mitigating these cardiovascular complications in individuals with kidney failure.
Breathlessness Risk
Fluid overload in kidney failure, particularly in End-Stage Renal Disease, can result in difficulty breathing through a multifaceted process.
When the kidneys fail to effectively remove excess fluid from the body, the surplus accumulates in the bloodstream. This excess fluid can infiltrate the lungs, a condition known as pulmonary edema.
Pulmonary edema occurs as the fluid migrates from the bloodstream into the lung tissues and air sacs (alveoli). This leads to an impaired exchange of oxygen and carbon dioxide during respiration.
Consequently, oxygen levels in the bloodstream decrease, and carbon dioxide levels rise. The body responds by increasing the rate and depth of breathing in an attempt to improve oxygen uptake.
This heightened respiratory effort can result in shortness of breath, a sensation of breathlessness, and difficulty in getting enough air. As pulmonary edema worsens, these symptoms become more pronounced, often leading to severe respiratory distress.
Managing fluid balance through measures like dialysis and fluid restriction is essential for preventing and alleviating pulmonary edema and its associated respiratory complications in kidney failure patients.
Sodium Intake and Fluid Balance
Now, let’s explore a critical aspect of fluid overload management in kidney failure patients: the profound impact of sodium intake. Sodium, a key component of many foods, plays a pivotal role in fluid balance regulation.
Understanding how dietary sodium intake can contribute to fluid overload is vital for individuals grappling with kidney failure.
We delve into the intricate relationship between amounts of sodium intake and fluid retention, shedding light on essential dietary considerations and strategies for effective control of sodium intake and mitigate fluid overload risks.
Sodium and Blood Pressure Impact
Sodium intake has a profound impact on fluid balance and blood pressure regulation in dialysis patients. Sodium, a major component of table salt and many processed foods, plays a pivotal role in these processes.
Excessive sodium consumption contributes to fluid retention because sodium attracts water. When dialysis patients consume too much sodium, their bodies retain more fluid, leading to fluid overload. This not only exacerbates hypertension but also increases the risk of pulmonary edema and heart strain.
Elevated sodium levels can also interfere with blood pressure regulation. It can cause the blood vessels to constrict, increasing blood pressure. This is especially concerning for dialysis patients, as hypertension is a common complication and a significant cardiovascular risk factor in this population.
To manage fluid balance and blood pressure effectively, dialysis patients must closely monitor and restrict their sodium intake. Reducing the consumption of high-sodium foods like processed snacks, canned goods, and restaurant meals is crucial.
Healthcare providers often recommend a kidney-friendly diet that limits sodium intake, assisting in maintaining a healthier fluid balance and controlling blood pressure.
Low Sodium Diet and Fluid Balance
A low sodium diet plays a vital role in maintaining optimal fluid balance for dialysis patients, as it helps prevent fluid overload and related complications.
Sodium, a component of table salt, has a direct impact on fluid retention in the body. By limiting sodium intake, dialysis patients can better manage their fluid levels and blood pressure.
Foods to avoid on a low sodium diet include processed and packaged foods, as they are often high in salt content. Canned soups, deli meats, fast food, and salty snacks like chips should be minimized or eliminated. Additionally, restaurant meals can be a hidden source of excess sodium.
On the other hand, foods that can be included in a low sodium diet include fresh fruits and vegetables, lean meats, poultry, and fish. Cooking at home with fresh ingredients allows for better control over sodium content. Using herbs and spices for flavor instead of salt can also enhance the taste of dishes without compromising on dietary restrictions.
Overall, a low sodium diet is essential for dialysis patients to maintain proper fluid balance, control blood pressure, and reduce the risk of complications associated with excessive sodium intake.

Prevention of Fluid Overload
In order to prevent fluid overload, it's crucial that you are well-versed in various tracking methods and understand the necessary dialysis adjustments.
You'll need to know how to accurately monitor your fluid intake and interdialytic weight gain, as these can directly influence your dialysis treatment.
Tracking Methods
Tracking daily fluid intake is crucial for hemodialysis patients to prevent fluid overload and maintain their health. Here's how to effectively monitor fluid intake:
- Keep a Fluid Journal: Maintain a daily diary of all fluids consumed. Include details such as the type of beverage or food with high water content, quantity, and the time of consumption.
- Set Personalized Goals: Work closely with your healthcare team to establish personalized fluid intake goals tailored to your specific needs, kidney function, and any existing restrictions.
- Use Measuring Tools: Employ measuring cups or containers to accurately gauge liquid portions. This helps ensure that you're following your prescribed fluid limits.
- Be Sodium Savvy: Learn to recognize high-sodium foods and beverages, as sodium can increase thirst and fluid consumption. Read labels and choose low-sodium options whenever possible.
- Hydrate Mindfully: Consume fluids in small sips throughout the day rather than drinking large amounts at once. This can help manage thirst while staying within your fluid limits.
- Weigh Yourself Regularly: Consistently monitor your body weight, ideally at the same time each day and under similar conditions. Sudden weight gain may indicate fluid retention.
By meticulously tracking fluid intake, dialysis patients can effectively manage their fluid balance, reducing the risk of fluid overload and associated complications like hypertension, heart strain, and pulmonary congestion.
Open communication with healthcare providers is essential for maintaining and adjusting fluid intake goals as needed for optimal health management.
Dialysis Adjustments
During dialysis, adjustments are made for chronic kidney disease patients who have fluid overload to safely remove excess fluid without causing further complications. Here are the key adjustments:
- Ultrafiltration Rate: Dialysis machines control the rate at which excess fluid is removed, known as the ultrafiltration rate. For patients with fluid overload, this rate may be adjusted to remove more fluid during the session.
- Treatment Time: In some cases, dialysis sessions may be extended to allow for a slower and more gradual removal of excess fluid. Longer treatment times can help prevent abrupt changes in blood volume, reducing the risk of low blood pressure or cramping.
- Prescribed Dry Weight: Dialysis patients have a prescribed dry weight, which represents their optimal post-dialysis weight without excess fluid. Adjustments may be made to this dry weight based on the patient's clinical condition and fluid status.
- Monitoring: Dialysis staff closely monitor patients during treatment, assessing vital signs and symptoms of fluid imbalance. If needed, adjustments can be made in real-time to ensure patient safety.
- Regular Assessments: Healthcare providers regularly assess the patient's overall fluid status and adjust the dialysis prescription as necessary to maintain fluid balance.
These adjustments are made to prevent complications like hypotension (low blood pressure) during treatment while effectively addressing fluid overload in chronic hemodialysis patients. They are tailored to each patient's unique needs and clinical condition, ensuring the safest and most effective fluid removal process.
Individualized Fluid Management
Individualized or personalized fluid management is a critical aspect of dialysis care, recognizing that every individual patient's fluid needs and tolerances are unique. In the realm of dialysis, one size does not fit all. This approach tailors fluid removal during dialysis to the specific requirements and medical conditions of each patient.
By recognizing the importance of personalized fluid management, we can optimize the effectiveness of dialysis treatments while minimizing the risk of complications related to fluid balance, such as hypotension and cardiac strain.
Personalized Adjustments
Personalized adjustments in fluid intake and dialysis parameters are vital for achieving fluid balance in kidney failure patients, particularly those undergoing dialysis. Here's how these adjustments play a crucial role:
- Assessing Individual Dry Weight: Determining an individual's dry weight, which is their target post-dialysis weight without excess fluid, is fundamental. This personalized dry weight accounts for factors like residual kidney function, comorbidities, and dietary habits.
- Customized Fluid Restrictions: Dialysis patients receive tailored fluid restriction recommendations based on their specific dry weight and urine output. These restrictions help manage fluid intake and prevent fluid overload.
- Dialysis Prescription: Dialysis treatment parameters, including the duration, frequency, and ultrafiltration rate, are individualized to match each patient's needs. This customization prevents rapid fluid removal that can lead to hypotension and other complications.
- Regular Monitoring: Continuous monitoring of vital signs, fluid weight gain, and symptoms during dialysis sessions allows for real-time adjustments. Dialysis staff can adapt the treatment plan as needed to maintain fluid balance.
- Educational Support: Patients receive education and guidance on recognizing signs of fluid overload and adhering to fluid restrictions. This empowers them to play an active role in managing their fluid intake.
- Fluid Journaling: Encouraging patients to maintain fluid intake journals helps track daily consumption accurately and enables healthcare providers to fine-tune recommendations.
Personalized fluid management for kidney failure patients optimizes the effectiveness of dialysis while minimizing complications associated with fluid imbalance.
It recognizes the unique physiological and lifestyle factors that influence each patient's fluid status, ultimately improving their quality of life and overall health.
Specific Restrictions
Specific fluid restrictions for individual kidney failure patients are crucial because the fluid needs and tolerances can vary widely due to a range of factors, necessitating more or less stringent restrictions. Here are some key considerations:
- Residual Kidney Function: Patients with some remaining kidney function may require less stringent fluid restrictions because their kidneys can still help remove some excess fluid. Conversely, those with little to no residual function may need stricter restrictions.
- Comorbidities: Patients with conditions like congestive heart failure or hypertension may need stricter fluid restrictions because excess fluid can exacerbate these conditions. Those without such conditions may have more lenient restrictions.
- Dietary Habits: Patients who consume high-sodium diets may need more stringent fluid restrictions to compensate for increased thirst and sodium-induced fluid retention.
- Individual Tolerance: Some patients may be more sensitive to fluid removal during dialysis, experiencing symptoms like hypotension or muscle cramps. Their fluid restrictions may need to be adjusted to minimize these side effects.
- Urine Output: Patients who still produce urine may be able to tolerate higher fluid intake, while those with minimal urine output will likely require stricter restrictions.
- Body Size and Composition: Larger individuals may require more lenient restrictions due to their higher volume of distribution, while smaller individuals may need stricter limits.
- Personal Preferences: Patient adherence is crucial. A tailored fluid restriction plan that aligns with a patient's lifestyle and preferences is more likely to be followed.
Specific fluid restrictions are essential in kidney failure patients because various factors influence their fluid needs and tolerance levels.
Customizing these restrictions based on individual characteristics and conditions ensures optimal fluid management, minimizing the risk of fluid overload and its associated complications.
Fluid Maintenance Tips
Effective fluid management is crucial for individuals with kidney issues, particularly those undergoing dialysis.
This section explores valuable tips for managing fluid intake, preventing fluid overload (fluids to hydrate with kidney disorder) and striking the right balance between hydration and restriction.
We'll delve into strategies for handling thirst and cravings, helping patients maintain their dietary and fluid restrictions while optimizing their overall well-being.
On Hydration Choices
For individuals with End-Stage Renal Disease who are on fluid restriction, making the right choices about fluid intake is crucial. The best types of fluids to consume include:
- Water: Plain water is the healthiest choice and is generally allowed in moderation.
- Ice Chips: Sucking on ice chips can help alleviate thirst without increasing fluid intake significantly.
- Fruit Juices: Limit intake of fruit juices due to their natural sugar content. Dilute with water to reduce sugar and potassium content.
- Herbal Teas: Non-caffeinated herbal teas, like chamomile or peppermint, are a good option for variety.
- Homemade Broths: Preparing low-sodium homemade broths or stocks can provide flavor without excessive sodium. Give this chicken broth kidney disease a try!
Conversely, fluids to avoid or limit include:
- Soda and Carbonated Drinks: Soft drinks and other carbonated drinks are typically high in sodium and phosphorus and should be avoided.
- Energy Drinks: High caffeine and sugar content make them unsuitable for ESRD patients.
- Alcohol: Limit alcoholic drinks, as it can lead to dehydration.
- Caffeinated Beverages: Coffee, tea, and caffeinated sodas can increase thirst and should be consumed sparingly.
- High-Sodium Liquids: Avoid soups, broths, and sauces with high sodium content.
Consulting a nephrologist or renal dietitian is essential to create an individualized fluid management plan that aligns with specific dietary restrictions and overall health goals for ESRD patients.
Managing Cravings
Managing thirst and cravings for dialysis patients on fluid restriction can be challenging but essential for maintaining health. Here are some strategies to help:
- Ice Chips: Sucking on ice chips can help quench thirst without significantly increasing fluid intake.
- Rinse Mouth: Swishing and rinsing the mouth with cold water can provide a refreshing feeling without swallowing excess fluids.
- Chew Gum or Sugar-Free Candy: Opt for sugar-free options to stimulate the mouth and reduce the sensation of thirst.
- Flavorful Ice Cubes: Freeze small amounts of flavored, low-calorie liquids (like fruit juice) into ice cube trays for a refreshing treat.
- Limited Salt Intake: Reducing sodium intake can help control thirst, as salt can make you feel thirstier. You can learn how to season food without salt.
- Sip Slowly: When drinking allowed fluids, sip slowly and savor each mouthful to make it last longer.
- Mindful Eating: Chewing food thoroughly and eating slowly can help reduce the desire for fluids during meals.
- Distraction: Engage in activities that divert your attention away from thirst, like reading, hobbies, or watching TV.
- Consult Dietitian: Work closely with a renal dietitian who can provide personalized advice and meal planning to manage thirst and cravings while adhering to fluid restrictions.
It's crucial for dialysis patients to follow their prescribed fluid restrictions while exploring these strategies to maintain comfort and adhere to their dietary and fluid limitations effectively.
Fluid Restrictions: Effects and Challenges
You're about to delve into an insightful discussion on the topic of fluid restrictions, particularly their effects and challenges. This also works for fluid restrictions for dialysis.
The benefits you'll uncover are numerous, from improved kidney function to better overall health. However, it's not without its hurdles; adhering to a strict fluid intake can be difficult, but we'll explore these challenges in detail to give you a comprehensive understanding.
Benefits
Proper fluid management is paramount for dialysis patients, offering a multitude of benefits:
- Blood Pressure Control: Maintaining fluid balance helps control blood pressure, reducing the risk of hypertension-related complications, such as heart disease and stroke.
- Reduced Risk of Fluid Overload: Effective fluid control prevents fluid overload, which can lead to edema, shortness of breath, and heart strain.
- Enhanced Dialysis Efficacy: Adequate fluid management ensures that the dialysis process is more efficient, effectively removing waste products and toxins from the bloodstream.
- Minimized Dialysis Complications: Well-regulated fluid levels reduce the risk of hypotension (low blood pressure) during dialysis, decreasing the likelihood of cramps, nausea, and other treatment-related complications.
- Improved Quality of Life: By preventing fluid-related symptoms and complications, proper fluid management enhances the overall quality of life for dialysis patients (recipes for dialysis patients), allowing them to feel more comfortable and in control of their health.
In summary, optimal fluid management is integral to the well-being of dialysis patients, mitigating the risk of complications, enhancing treatment effectiveness, and improving their overall quality of life.
Challenges
Dialysis patients often face significant challenges when adhering to fluid restrictions, which can be frustrating and impact their overall well-being. Here's a table summarizing these challenges and possible corresponding solutions:
| Challenges | Possible Solutions |
| Persistent Thirst | Chew sugar-free gum or ice chips. Rinse the mouth. |
| Cravings | Use flavored ice cubes or consume sugar-free candy. |
| Dehydration Fear | Educate patients about proper hydration methods. |
| Sodium Intake | Limit high-sodium foods. Opt for low-sodium options. |
| Social Pressure | Communicate dietary needs to friends and family. |
| Mental Stress | Encourage mindfulness techniques to manage stress. |
| Monitoring Difficulty | Keep a fluid intake journal for accurate tracking. |
| Dining Out | Choose restaurants with kidney-friendly options. |
These challenges are common but can be mitigated through a combination of education, support, and strategies to help dialysis patients effectively manage fluid restrictions and maintain their health. Find out more about kidney safe candy and what to eat.
Consistency in Control
Want to how to manage chronic kidney disease? Consistency in fluid intake control is a paramount aspect of managing kidney issues, especially for dialysis patients. It involves unwavering commitment to adhering to prescribed fluid limits consistently, day in and day out.
This discipline plays a crucial role in preventing complications associated with fluid imbalance, such as hypertension and fluid overload. In this section, we delve into the importance of maintaining this steadfast approach to fluid intake management and provide tips on how individuals can achieve this vital consistency.
General Guidelines
Fluid limits for dialysis patients are highly individualized and may vary based on factors such as residual kidney function, body size, and medical history.
However, a general guideline is to restrict daily intake to around 32 ounces of fluid or less. Here are some additional general guidelines:
- Consult a Healthcare Provider: Always follow the fluid restrictions prescribed by your healthcare team, as they will tailor these limits to your specific needs.
- Include All Fluids: Fluid restrictions encompass all beverages and foods with high water content, not just water itself.
- Monitor Symptoms: Pay attention to signs of fluid overload, such as swelling, shortness of breath, or sudden weight gain between treatments as these may indicate the need for stricter fluid limits.
- Maintain a Fluid Journal: Keeping a record of daily fluid intake helps track adherence to limits and facilitates communication with healthcare providers for necessary adjustments.
- Limit High-Sodium Foods: Sodium can increase thirst. Reducing sodium intake by avoiding processed and salty foods can help manage thirst and fluid intake.
Always consult with your healthcare provider or renal dietitian for personalized fluid restriction guidelines that align with your specific health needs and goals.
A Daily Habit
Here's a sample daily fluid intake summary that includes food items and stays under 32 ounces:
| Fluid Type | Amount (in ounces) |
| Water | 8 |
| Herbal Tea | 12 |
| Breakfast Juice | 4 |
| Ice Chips | 2 |
| Soup (Lunch) | 4 |
| Snack: Fruit with high water content | 2 |
| Total Fluid Intake | 32 ounces |
In this example, the individual has consumed a total of 32 ounces of fluids throughout the day, staying within the general guideline of 32 ounces or 1 liter for dialysis patients.
The summary accounts for various fluid sources, including beverages, foods like soup, and fruits with high water content. Monitoring fluid intake in this way helps ensure adherence to prescribed limits and proper fluid balance.
FAQs for Fluid Restriction Guidelines
Excessive fluid intake during dialysis can lead to fluid overload. Some signs and symptoms include sudden weight gain, swelling in the ankles or legs, shortness of breath, high blood pressure, and fatigue.
These indicators suggest that the body is retaining too much fluid, which can strain the heart and lead to serious complications. It's crucial to adhere to prescribed fluid restrictions and monitor these symptoms to maintain proper fluid balance during dialysis.
Yes, some beverages and foods can increase fluid retention in dialysis patients. High-sodium foods like processed snacks and CKD, canned soups, and salty snacks can lead to fluid retention due to sodium's water-attracting properties.
Additionally, caffeinated beverages like coffee and tea can contribute to increased thirst and potentially lead to higher fluid intake. Patients should be cautious with these items and adhere to their prescribed fluid restrictions to maintain proper fluid balance during dialysis.
To measure daily fluid intake accurately, you can:
1. Use measuring cups or containers for beverages.
2. Maintain a fluid intake journal, recording types, amounts, and times.1.
3. Include foods with high water content (like fruits and soups) in your tracking.
4. Be mindful of serving sizes when eating out.
5. Limit high-sodium foods, as sodium can increase thirst. Low Sodium Canned Foods For CKD.
6. Weigh yourself daily at the same time, as sudden weight gain may indicate fluid retention.
These practices help ensure precise monitoring of fluid intake, aiding in adherence to prescribed restrictions.
Lifestyle habits and exercises can complement fluid management for dialysis patients. Regular light physical activity (exercise for healthy heart) can promote circulation and reduce fluid buildup in the extremities. Mindfulness techniques, such as meditation or deep breathing, can help manage thirst and cravings.
Moreover, maintaining a balanced diet with limited sodium and high-potassium foods supports overall fluid restriction goals. Consulting with a healthcare team and following their guidance is essential for creating a holistic approach to effective fluid management.
Yes, the type of dialysis you're on does impact your fluid intake. With hemodialysis, there are stricter fluid limitations because it's typically performed three times a week. Peritoneal dialysis, done daily at home, allows more hydration.
Choosing a dialysis method depends on your lifestyle and health condition. Patient experiences vary greatly between the two types. It's crucial to discuss with your healthcare team for an informed decision about which is best for you.
Fluid Restriction Is Challenging, But It Is Necessary
Fluid restrictions can be difficult at first, but the more you pay attention and keep up with it, the easier it will become. It is important for you to follow through. Remember that this is all to help you live more comfortably even with end-stage renal disease, so keep up the good work. Do you have questions about end stage renal disease?
Fluid restrictions have the potential to be a bit more difficult than you may think. There are fluids in most foods you eat, not to mention that thirst could seriously hinder your ability to follow through properly.
In the end, however, following your doctor’s orders will not only keep you healthier longer but follow through will also help you to live a more comfortable life. Talk with your healthcare providers if you have more questions about fluid restrictions for chronic kidney disease.