End Stage Renal Disease
End-Stage Renal Disease (ESRD) marks the final, critical stage of chronic kidney disease, where the kidneys' ability to perform essential functions is severely compromised. Individuals facing ESRD encounter life-altering challenges, often requiring extensive medical intervention and a new perspective on daily life.
In this article, we delve into the complexities of ESRD, exploring its causes, symptoms, and the various treatment options available, including dialysis and kidney transplantation.
Understanding this stage of kidney disease is essential, as it sheds light on the experiences, choices, and resilience of those who confront ESRD and the critical decisions they must make to ensure continued health and well-being.
Jump to:
- Key Takeaways
- Understanding End Stage Renal Disease
- The Role of Kidneys in the Human Body
- Symptomatology of End Stage Renal Disease
- Importance of Early Detection
- Potential Risk Factors for Kidney Disease
- Common Causes of Kidney Damage
- Life-Saving Role of Dialysis in Renal Disease
- More on the Dialysis Process
- Kidney Transplants: A Gold Standard in ESRD
- Challenges in Kidney Transplantation
- Lifestyle Modifications for Managing Kidney Disease
- Future Perspectives in the Treatment of Kidney Disease
- Frequently Asked Questions
- End Stage Renal Disease Shouldn’t Mean It’s The End
Key Takeaways
- End Stage Renal Disease is a condition where the kidneys are no longer able to function properly, leading to the buildup of waste products and excess fluid in the body.
- Symptoms of the disease may not appear until kidney function is significantly impaired.
- Early detection of renal disease is crucial in managing the condition and minimizing its impact on health.
- The kidneys play a vital role in maintaining homeostasis, regulating electrolytes, and producing hormones that affect other organs in the body.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding End Stage Renal Disease
End-Stage Renal Disease or permanent kidney failure is the most advanced stage of Chronic Kidney Disease (CKD) and represents a critical milestone in the spectrum of kidney health.
CKD is typically categorized into five stages based on the glomerular filtration rate (GFR), a measure of kidney function. ESRD is Stage 5, where the GFR drops to 15 milliliters per minute or less, indicating a profound loss of kidney function.
At this stage, the kidneys are severely damaged and can no longer efficiently filter waste products, excess fluids, and electrolytes from the blood. Consequently, ESRD leads to a host of systemic complications, including fluid retention, high blood pressure, anemia, bone disorders, and metabolic abnormalities.
ESRD profoundly impacts an individual's overall health and quality of life. Symptoms can be debilitating, causing severe fatigue, nausea, and an array of symptoms related to the imbalances in the body.
The management of ESRD typically involves one of two long-term renal replacement therapies:
- Dialysis: Dialysis is a medical procedure that artificially filters the blood to remove waste and excess fluid, compensating for the lost kidney function. Two primary forms exist:
- Hemodialysis: A machine filters the blood outside the body, typically performed at a dialysis center three times a week.
- Peritoneal Dialysis: The patient's abdominal lining (peritoneum) filters the blood by filling and draining a sterile solution, usually performed at home.
- Kidney Transplantation: A kidney transplant is considered the best treatment option for ESRD, offering the prospect of a more normal life. However, it necessitates finding a compatible donor, and lifelong immunosuppressive medications are required to prevent organ rejection.
ESRD represents the most severe manifestation of CKD, necessitating advanced medical intervention. Timely CKD management is vital to delay its progression and maximize the opportunity for effective treatment and an improved quality of life.
Disease Progression and Symptoms
End-Stage Renal Disease represents the advanced and often irreversible culmination of Chronic Kidney Disease. CKD progresses through five stages, with ESRD being the final stage.
Initially, in Stages 1-3, kidney damage is present, but symptoms may be mild or absent. As CKD advances to Stage 4, kidney function significantly declines, leading to complications like high blood pressure and electrolyte imbalances.
By Stage 5, or ESRD, the GFR drops below 15 milliliters per minute, signifying critical kidney dysfunction. This stage results in severe symptoms, such as fluid retention, anemia, adynamic bone disease, and metabolic issues. ESRD necessitates renal replacement therapy, either through dialysis or kidney transplantation, as the kidneys can no longer filter waste products from the blood.
Thus, the progression from CKD to ESRD marks a profound transition, highlighting the urgency of timely CKD management to slow the decline in kidney function and enhance long-term health.
Importance of Early Detection
Early detection of Chronic Kidney Disease and identification of its risk factors are crucial in preventing progression to End-Stage Renal Disease. CKD often develops silently, with mild or no symptoms in its early stages. By the time symptoms manifest, the kidneys may be severely damaged.
Detecting CKD in its early stages through routine health screenings, particularly for individuals with risk factors like hypertension, diabetes, or a family history of kidney disease, allows for timely interventions.
With early detection, your kidney doctor can implement strategies to manage CKD effectively, slow its progression, and prevent the development of ESRD. These strategies include control of hypertension, medication management, dietary changes, and lifestyle modifications. The overarching goal is to preserve kidney function and improve the long-term health and quality of life for individuals at risk of CKD.
The Role of Kidneys in the Human Body
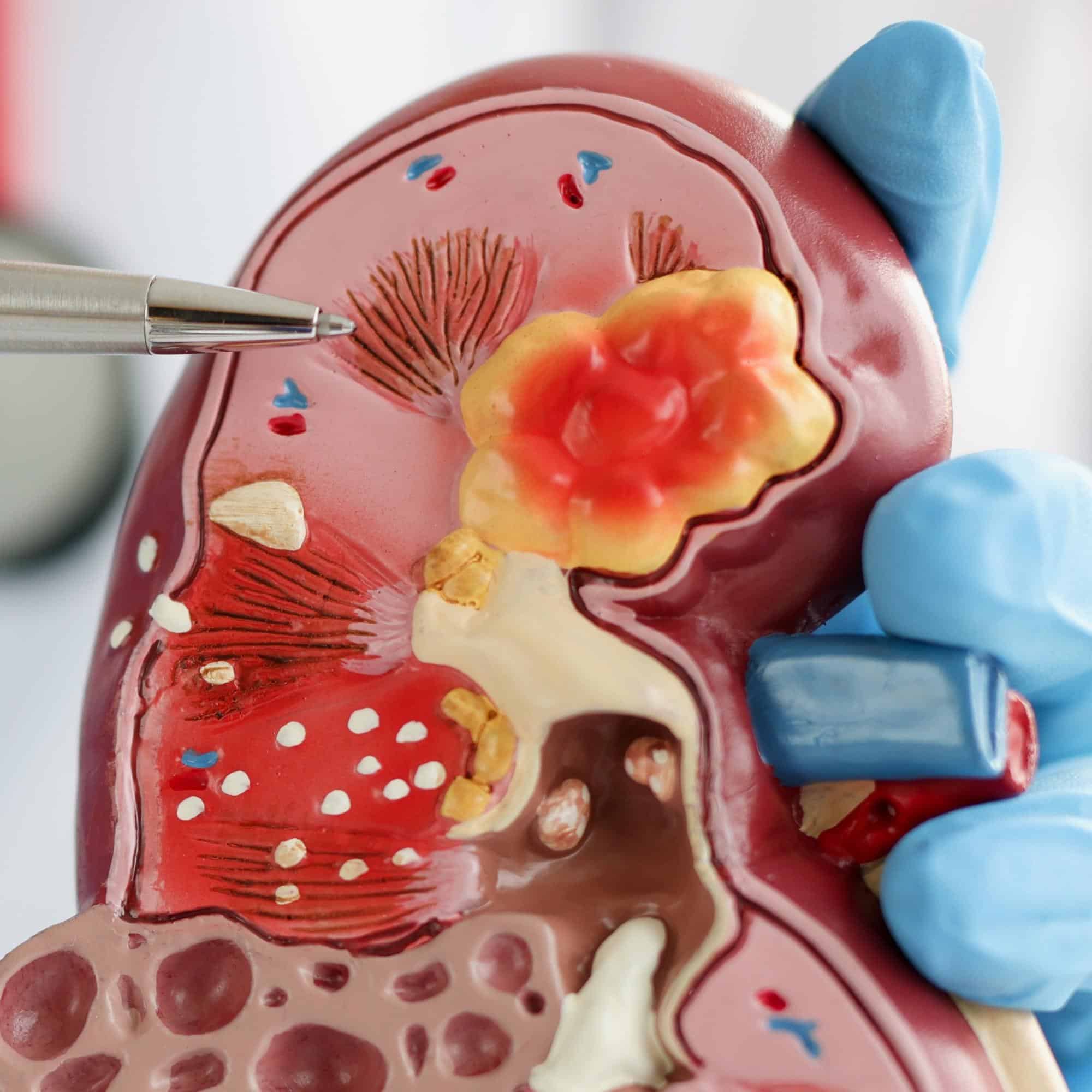
The kidneys are unsung heroes within the human body, performing a range of vital functions that are often overlooked. These bean-shaped organs filter waste products and excess fluids from the blood, maintain electrolyte balance, and regulate blood pressure. They also produce essential hormones that influence red blood cell production and calcium metabolism.
Kidney damage, as seen in conditions like Chronic Kidney Disease, can disrupt these functions, leading to a cascade of health issues. In this section, we explore the pivotal role of kidneys and the far-reaching consequences of kidney damage on the body's overall well-being.
Kidneys' Vital Functions
The kidneys perform several vital functions:
- Filtration and Excretion: The primary role of the kidneys is to filter waste products and excess substances, such as urea and creatinine, from the bloodstream. These waste materials are then excreted as urine.
- Fluid and Electrolyte Balance: The kidneys regulate the body's fluid balance, maintaining the right amount of water to ensure proper bodily functions. They also balance electrolytes like sodium, potassium, and calcium.
- Blood Pressure Regulation: The renin-angiotensin-aldosterone system helps control blood pressure. When blood pressure drops, the kidneys release renin, which initiates a series of reactions to raise blood pressure.
- Erythropoiesis Regulation: The kidneys produce erythropoietin, a hormone that stimulates the bone marrow to produce red blood cells. This is vital for maintaining adequate oxygen transport in the bloodstream.
- Acid-Base Balance: The kidneys help regulate the body's acid-base balance by excreting hydrogen ions and reabsorbing bicarbonate ions.
- Toxin and Drug Metabolism: They play a role in metabolizing and excreting certain medications and toxins.
- Calcium Homeostasis: The kidneys help control calcium levels in the body, which is essential for bone health and muscle function.
Kidney damage or disease, as seen in conditions like Chronic Kidney Disease (CKD), can disrupt these functions, leading to complications such as fluid retention, high blood pressure, anemia, and electrolyte imbalances. Hence, preserving kidney health is vital for overall well-being and homeostasis in the body.
Impact of Kidney Damage
Kidney damage can have a profound impact on the vital functions of these essential organs. When the kidneys are compromised, their ability to filter waste products and excess fluids from the blood is impaired, leading to a buildup of toxins in the body. This can disrupt electrolyte balance, contributing to high blood pressure, muscle weakness, and even cardiac arrhythmias.
Kidney damage also impairs the kidneys' capacity to produce erythropoietin, resulting in anemia due to reduced red blood cell production. Furthermore, it disrupts the delicate balance of calcium, affecting bone health and potentially causing bone disease.
Overall, kidney damage can compromise the intricate and interrelated functions of these organs, leading to a cascade of health issues and emphasizing the critical importance of kidney health for overall well-being.
Symptomatology of End Stage Renal Disease
End-Stage Renal Disease is marked by a myriad of symptoms that significantly impact daily life. From unrelenting fatigue and fluid retention to nausea and bone pain, the symptomatology of ESRD is both diverse and debilitating.
Recognizing these symptoms is crucial for timely intervention. This section delves into the common signs of ESRD, their consequences on daily life, and the importance of seeking medical attention for effective symptom management and treatment.
Identifying Disease Symptoms
End-Stage Renal Disease or Chronic Kidney Failure is characterized by a myriad of debilitating symptoms, profoundly affecting individuals' daily lives:
- Fatigue: Overwhelming and persistent exhaustion is a hallmark symptom, often limiting physical and mental activities.
- Fluid Retention: ESRD causes fluid buildup, leading to swelling, particularly in the legs and ankles (peripheral edema), and shortness of breath (pulmonary edema).
- Nausea and Vomiting: Gastrointestinal distress, often triggered by waste buildup, is common. Loss of appetite is also not uncommon, increasing the risk for malnutrition in dialysis patients.
- Anemia: Reduced red blood cell production causes anemia in CKD leading to weakness, pallor, and sometimes dizziness. This necessitates frequent laboratory test for complete blood count.
- Itching and Muscle Cramps: These are common skin and muscle discomforts associated with ESRD.
- Bone Pain: Mineral imbalances can lead to bone pain and an increased risk of fractures.
- Cognitive Changes: Cognitive decline includes difficulties concentrating and thinking clearly.
- Neurological Symptoms: In advanced stages, waste products can accumulate in the brain, leading to confusion and, in severe cases, coma.
These symptoms of kidney failure collectively impair the quality of life and emphasize the urgency of timely diagnosis and management to alleviate suffering and enhance the overall well-being of those confronting ESRD.
Symptom Impact on Life
The symptoms of End-Stage Renal Disease can profoundly disrupt daily life.
Overwhelming fatigue and weakness make even simple tasks challenging. Fluid retention causes discomfort, difficulty breathing, and limited mobility.
Nausea and vomiting disrupt eating habits and lead to weight loss. Anemia-induced weakness and dizziness make daily activities taxing.
Itching, muscle cramps, and bone pain erode comfort and sleep quality. Cognitive changes, including difficulties concentrating, impede work or study. Moreover, in advanced ESRD, waste accumulation can lead to confusion or coma, affecting decision-making and independence.
These symptoms not only diminish the quality of life but also pose psychological and emotional challenges, leading to anxiety and depression.
Coping with ESRD requires significant adjustments in lifestyle, including dietary restrictions and medical treatments like dialysis or transplantation. Timely intervention and holistic support are critical to mitigate the impact of these symptoms and improve the overall well-being of individuals grappling with kidney failure.
Importance of Early Detection
Early detection is paramount in the management of Chronic Kidney Disease and End-Stage Renal Disease. Recognizing symptoms in their early stages and routine kidney function tests can make all the difference in mitigating the progression of these conditions.
In this section, we delve into the significance of early detection, emphasizing the role of regular check-ups and diagnostic tests in identifying kidney disease when interventions can be most effective, potentially preventing the advanced stages of these debilitating conditions.
Symptom Recognition
Early detection of End-Stage Renal Disease hinges on the prompt recognition of symptoms, as this advanced stage of kidney disease often presents with subtle but significant signs.
Overwhelming and unexplained exhaustion is a common initial symptom, affecting daily energy levels. Swelling, particularly in the legs and ankles, along with unexplained weight gain, can be indicators of fluid buildup.
Gastrointestinal symptoms, especially persistent and unexplained nausea and vomiting, should raise concerns. Weakness, pallor, and dizziness may result from decreased red blood cell production. Unusual skin itching and muscle cramps can be early signs.
Recognizing these symptoms early is essential. They may not be severe but serve as red flags for kidney damage. Prompt evaluation by a healthcare provider and kidney function tests can facilitate timely intervention, potentially slowing the progression of ESRD and improving long-term outcomes.
Early detection and treatment play a pivotal role in managing this advanced stage of kidney disease effectively.
Routine Kidney Function Tests
Routine kidney function tests are essential for early detection of kidney disease, including the advanced stage known as End-Stage Renal Disease. These tests offer insights into how well the kidneys are functioning, enabling timely intervention and management. Here's a table of some key kidney function tests and their significance:
| Test | Significance |
| Glomerular Filtration Rate (GFR) | Measures the rate at which the kidneys filter waste. A lower GFR indicates reduced kidney function. |
| Serum Creatinine | Elevated levels suggest impaired kidney function since it's a waste product the kidneys should eliminate. |
| Blood Urea Nitrogen (BUN) | Elevated BUN levels indicate inefficient removal of urea from the bloodstream, often associated with kidney dysfunction. |
| Urinalysis | Examines the urine for abnormalities, including the presence of protein or blood, which can signal kidney damage. |
| Serum Electrolytes | Measures levels of sodium, potassium, and calcium, which can indicate electrolyte imbalances due to kidney dysfunction. |
| Albumin-to-Creatinine Ratio | High levels suggest kidney damage, as healthy kidneys prevent significant albumin from entering the urine. |
Regular monitoring of these kidney function tests is critical for early detection and effective management of kidney disease. It enables healthcare providers to intervene promptly, potentially slowing the progression of kidney disease and mitigating the risk of ESRD.
Potential Risk Factors for Kidney Disease
The risk factors for Chronic Kidney Disease are a blend of underlying health conditions and lifestyle choices. In this section, we delve into the key contributors that can predispose individuals to CKD.
From chronic diseases like diabetes and hypertension to lifestyle factors such as diet and smoking, understanding the risk landscape is crucial for prevention and early intervention. By exploring these factors, we aim to shed light on the importance of proactive health management in mitigating CKD's onset and progression.
Underlying Conditions Impact
Chronic Kidney Disease can stem from a variety of underlying conditions or clinical risk factors, often serving as a consequence of longstanding health issues:
- Diabetes: Prolonged uncontrolled high blood sugar damages the small blood vessels in the kidneys, impairing their filtration capacity and triggering CKD due to diabetic nephropathy.
- Hypertension: Elevated blood pressure strains the kidney's blood vessels, causing inflammation and eventual scarring, which can disrupt kidney function.
- Glomerulonephritis: Inflammation of the glomeruli, the kidney's filtering units, can lead to kidney damage.
- Polycystic Kidney Disease (PKD): An inherited disorder causing cysts in the kidneys that gradually replace healthy tissue and impair function.
- Kidney Stones: Recurrent kidney stones can damage the kidneys and contribute to CKD.
- Autoimmune Diseases: Conditions like Systemic Lupus Erythematosus (SLE) can impact various organs, including the kidneys, resulting in kidney damage.
Understanding the underlying conditions that can lead to CKD is pivotal for early detection, management, and prevention of kidney disease, underscoring the significance of addressing these health concerns proactively.
Lifestyle and Kidney Health
Lifestyle habits play a significant role in the development and progression of Chronic Kidney Disease and End-Stage Renal Disease. These are considered modifiable risk factors and several factors contribute to kidney damage:
- Unhealthy Diet: High consumption of processed foods, excessive salt, and a diet low in fruits and vegetables can raise the risk of hypertension and diabetes, key drivers of CKD.
- Smoking: Smoking not only raises blood pressure but also impairs blood flow to the kidneys, increasing the risk of kidney disease.
- Excessive Alcohol Consumption: Heavy drinking can disrupt the kidney's filtration process and contribute to hypertension.
- Lack of Physical Activity: A sedentary lifestyle can lead to obesity, diabetes, and hypertension, which are all risk factors for development of CKD.
- Dehydration: Insufficient water intake can lead to the formation of kidney stones and other kidney-related problems.
- Overuse of Over-the-Counter Pain Medications: Non-prescription pain relievers, when used excessively, can harm the kidneys.
Addressing these lifestyle factors through a balanced diet, regular exercise, smoking cessation, and moderation in alcohol consumption is vital in reducing the risk of CKD and ESRD and promoting overall kidney health.
Common Causes of Kidney Damage
The leading causes of Chronic Kidney Disease are often silent, yet their impact is profound. In this section, we delve into the two most prevalent culprits: hypertension and diabetes. Hypertension, or high blood pressure, and diabetes are insidious conditions that can quietly ravage kidney health.
Understanding their mechanisms, effects, and management is crucial for preventing the onset or progression of CKD, highlighting the importance of proactive health management in the face of these pervasive risk factors.
High Blood Pressure Impact
High blood pressure, or hypertension, is a leading cause of End-Stage Renal Disease and a major contributor to the progression of Chronic Kidney Disease. Hypertension exerts damaging effects on the delicate blood vessels in the kidneys. Prolonged high pressure can cause these vessels to narrow and become less efficient in filtering blood, leading to a reduction in the glomerular filtration rate, a key measure of kidney function.
This decline in GFR causes the kidneys to work harder to compensate, which in turn, damages the kidney's filtering units and their surrounding tissues. Over time, the kidneys can become scarred and fibrotic, further impairing their ability to filter waste and excess fluid.
Additionally, hypertension promotes the release of angiotensin II, a hormone that constricts blood vessels and can cause inflammation in the kidneys, accelerating kidney damage.
Managing hypertension through lifestyle changes and blood pressure medicines is crucial in preventing hypertension-induced CKD and ESRD.
Diabetes' Role in Damage
Diabetes mellitus, especially Type 2 diabetes, plays a central role in the development of End-Stage Renal Disease by exerting a multifaceted impact on kidney health.
Prolonged elevated blood sugar levels associated with diabetes place significant stress on the glomeruli, the kidney's filtration units, leading to glomerular damage, thickening, and scarring of the filtration membranes. This, in turn, impairs their ability to filter blood effectively.
Additionally, diabetes can cause the glomerular filters to become more permeable, allowing proteins like albumin to escape into the urine, a condition known as proteinuria, often indicating kidney damage. Hypertension, a common comorbidity of diabetes, further stresses the delicate kidney blood vessels, leading to inflammation and damage.
Moreover, chronic inflammation and fibrosis in the kidney tissue, triggered by persistent poor glycemic control, contribute to the progressive impairment of kidney function over time.
Effective diabetes management, encompassing blood sugar control, blood pressure regulation, lifestyle modifications, and medication, is essential for mitigating the risk of kidney damage and preventing the progression to ESRD. Early detection, proactive monitoring, and timely intervention are paramount in preserving kidney function for individuals living with diabetes.
Life-Saving Role of Dialysis in Renal Disease
Dialysis is a life-saving intervention that plays a vital role in the management of advanced kidney disease. In this section, we explore the critical and transformative role of dialysis in the context of renal disease. By delving into the types, techniques, and considerations for choosing dialysis, we aim to shed light on how this vital procedure helps sustain life and improve the well-being of individuals facing the challenges of kidney failure.
Dialysis Procedure
Dialysis is a life-sustaining medical procedure designed to mimic the kidney's vital functions when they fail. The procedure involves the removal of excess waste, toxins, and fluid from the blood, which the kidneys would typically filter and eliminate. Two primary forms of dialysis exist: hemodialysis and peritoneal dialysis.
Hemodialysis operates by diverting blood from the patient's body into a machine called a dialyzer, which filters the blood and returns it, purified, back to the patient. In contrast, peritoneal dialysis involves introducing a sterile solution into the patient's abdomen to facilitate the exchange of waste and excess fluid through the peritoneal membrane.
Dialysis serves as a lifeline for individuals with kidney failure, offering a bridge to transplantation or a long-term management solution for those not suitable for transplant.
Types and Considerations
There are two primary types of dialysis: hemodialysis and peritoneal dialysis, each with distinct considerations.
- Hemodialysis:
- Location: Typically performed in a specialized dialysis center, requiring regular visits, often thrice weekly.
- Procedure: Blood is removed from the patient's body, filtered through a machine (dialyzer) to eliminate waste and excess fluid, and then returned to the patient.
- Considerations: Requires vascular access, usually in the form of an arteriovenous fistula or graft, to allow blood flow in and out of the body. Regular transportation to a dialysis center is necessary.
- Peritoneal Dialysis:
- Location: Can be performed at home, offering more flexibility and independence.
- Procedure: A sterile dialysis solution is introduced into the patient's abdomen, where it remains for a prescribed period, allowing waste and excess fluid to diffuse through the peritoneal membrane into the solution, which is then drained out.
- Considerations: Requires surgical placement of a catheter in the abdomen. Offers more autonomy, but requires meticulous hygiene practices. Suited for individuals who prefer home-based care or have limited vascular access options.
The choice between these types depends on individual circumstances, including medical suitability, lifestyle preferences, and patient education and support. Both aim to effectively manage kidney failure, albeit with distinct considerations and impacts on daily life.
More on the Dialysis Process
This section delves into the world of hemodialysis, examining its effectiveness as a life-sustaining treatment for kidney failure. We explore not only the clinical aspects but also the often-overlooked human dimension - the patient's perspective. From the science behind hemodialysis to the personal experiences of those who depend on it, this section offers a comprehensive understanding of the impact, challenges, and outcomes of this vital medical intervention.
Dialysis Effectiveness
Dialysis is a highly effective treatment for managing symptoms associated with End-Stage Renal Disease, although its effectiveness is multi-faceted:
- Symptom Management: Dialysis efficiently removes waste products and excess fluid from the blood, reducing symptoms like fatigue, nausea, and swelling.
- Life Expectancy: While dialysis doesn't cure ESRD, it significantly extends life expectancy, enabling individuals to lead longer, more productive lives.
- Quality of Life: Effective symptom control and regular dialysis treatments can improve the quality of life for ESRD patients, allowing them to engage in daily activities and maintain some semblance of normalcy.
- Monitoring and Measurement: The effectiveness of dialysis is continually assessed through various measures, including monitoring blood pressure, blood tests to ensure adequate waste removal, and assessing the patient's overall well-being.
While dialysis is life-sustaining, it does come with challenges and lifestyle adjustments. The effectiveness is not only measured in clinical terms but also in the improvement of a patient's life, the relief from debilitating symptoms, and the prolongation of life, offering hope and a chance for a better future.
Dialysis Patient Experience
The patient experience in dialysis is a complex interplay of positive and negative facets, shaped by the life-sustaining nature of the treatment:
Positive Experiences:
- Symptom Relief: Many patients on dialysis experience significant relief from debilitating symptoms associated with ESRD, such as fatigue and swelling.
- Life Extension: Dialysis prolongs life, providing an opportunity for patients to spend more time with loved ones and achieve personal goals.
- Supportive Community: Dialysis centers often foster a sense of community, allowing patients to connect with others who share their experiences.
- Improved Quality of Life: Effective treatment enhances the quality of life, enabling patients to lead more fulfilling, active lives.
Negative Experiences:
- Inconvenience: Frequent dialysis sessions can be disruptive, requiring adjustments to work and daily routines.
- Physical Discomfort: Some patients may experience discomfort or complications related to vascular access or peritoneal catheters.
- Emotional Strain: The need for lifelong treatment can be emotionally taxing, leading to feelings of anxiety and depression.
- Limited Diet and Fluid Intake: Dietary restrictions and fluid limitations can be frustrating, affecting the enjoyment of meals and beverages.
The patient experience in dialysis is a delicate balance of relief, hope, and challenges. It underscores the resilience and adaptability of individuals facing the complexities of chronic kidney disease.
Kidney Transplants: A Gold Standard in ESRD
Kidney transplantation stands as the gold standard in the management of End-Stage Kidney Disease, offering the promise of renewed life and freedom from dialysis. In this section, we delve into the intricate process of kidney transplantation, exploring the eligibility criteria for potential recipients and the critical aspects of post-transplant care. Understanding who qualifies for this life-changing procedure and what it entails afterward is essential for those navigating the journey from ESRD to renewed health and vitality.
Transplant Eligibility Criteria
Eligibility for kidney transplantation, often considered the best treatment for End-Stage Renal Failure, involves careful assessment based on a range of factors:
- Medical Evaluation: Candidates undergo a thorough medical evaluation to ensure they are healthy enough for surgery. Existing medical conditions such as heart disease or cancer are considered.
- Compatible Donor: A suitable donor, either living or deceased, must be identified. Compatibility is determined through blood type and tissue matching.
- Age and Overall Health: Age and general health are considered. While there is no strict age limit, older candidates may face additional scrutiny.
- Psychological Evaluation: Mental and emotional stability is assessed to ensure candidates can cope with the challenges of transplantation and post-operative care.
- Commitment: Transplant recipients must demonstrate commitment to lifelong post-transplant care, including immunosuppressive medications.
- Financial and Social Support: Having the necessary financial means and social support for pre and post-transplant care is essential.
Transplantation can provide a new lease on life, but the criteria are rigorous. A comprehensive evaluation helps determine if a candidate is a suitable candidate for this life-changing procedure.
Post-Transplant Care
Post-transplant care is a critical phase for individuals who have received a kidney transplant, aiming to ensure the success of the procedure and overall well-being.
It encompasses several key components, starting with the necessity of immunosuppressive medications to prevent kidney rejection. Adherence to the medication regimen is paramount. Regular medical check-ups are essential to monitor kidney function, assess overall health, and make necessary medication adjustments.
Adopting a healthy lifestyle that includes a balanced diet, regular exercise, and quitting smoking is vital for protecting the transplanted kidney and sustaining overall health.
Immunosuppressive drugs can increase the risk of infections, emphasizing the need for precautionary measures. Emotional support through counseling and support groups is indispensable in navigating the emotional challenges that can arise during the post-transplant journey.
Additionally, managing the financial aspects of post-transplant care, including medications and follow-up appointments, is a practical consideration that transplant recipients must address.
Challenges in Kidney Transplantation
The journey through kidney transplantation, while transformative, is not without its share of challenges. In this section, we delve into the complex dynamics of kidney transplantation, exploring two pivotal aspects: the availability of suitable donors and the demanding landscape of post-transplant care which can involve a number of complications.
These challenges, spanning the search for donors to the intricacies of lifelong care, offer insights into the complexities of this life-changing procedure and the resilience required to overcome them.
Donor Kidney Availability
The availability of donor kidneys significantly impacts the prospects of End-Stage Renal Failure patients for transplantation. The demand for kidney transplants far outweighs the supply of available organs, resulting in long waiting lists. Several factors influence donor kidney availability:
- Deceased Donors: Organs from deceased donors contribute a substantial portion of available kidneys. Their availability depends on factors like accidents, medical conditions, and consent for organ donation.
- Living Donors: Kidneys from living donors offer a viable alternative, but the willingness of individuals to donate is limited. Compatibility and health of potential living donors are also factors.
- Transplant Centers: Different regions may have varying transplant center densities, affecting the access to available kidneys. Patients may need to travel to find centers with shorter waiting lists.
- Legal and Ethical Considerations: Legal and ethical concerns surrounding organ procurement can influence donor availability.
- Allocation Systems: Allocation systems prioritize recipients based on various criteria, including medical urgency and waiting time.
The shortage of donor kidneys underscores the need for broader organ donation awareness, improvements in allocation systems, and the importance of living donations. It's a challenging landscape that ESRD patients must navigate in their quest for a new lease on life through transplantation.
Transplant Complications
Kidney transplant, while transformative, can present several complications and challenges for End-Stage Renal Disease patients. These challenges include:
- Rejection: The recipient's immune system may identify the transplanted kidney as a foreign entity and attempt to reject it. Immunosuppressive drugs are needed to prevent rejection.
- Infection: Immunosuppressive medications, vital for preventing rejection, can weaken the immune system, making recipients more susceptible to infections.
- Organ Damage: The transplanted kidney may experience complications, such as clot formation or blockages in blood vessels, which can affect its function.
- Side Effects: Medication side effects can be challenging, including weight gain, infections, high blood pressure, and increased risk of diabetes.
- Post-Transplant Lymphoproliferative Disorder (PTLD): This is a rare condition where the immune system responds excessively to the immunosuppressive drugs, causing lymph gland enlargement.
- Long-Term Monitoring: Lifelong post-transplant care, involving continuous medication and regular check-ups, is necessary to manage these complications.
Navigating these challenges is part of the kidney transplant journey, and patients must maintain close contact with healthcare providers to ensure the success of the procedure and their overall well-being.
Lifestyle Modifications for Managing Kidney Disease
Lifestyle modifications play a pivotal role in managing kidney disease and promoting overall well-being. In this section, we explore the positive impact of specific changes to one's daily habits and choices.
From dietary adjustments to exercise routines, hydration practices, and stress management, these modifications are not only beneficial for kidney health but can enhance the quality of life for those navigating the challenges of kidney disease. Understanding the power of these lifestyle changes empowers individuals to take an active role in their health and well-being.
Dietary Changes Benefits
Dietary changes are of paramount importance for individuals with End-Stage Renal Disease, especially those on dialysis. The dialysis diet is carefully designed to manage the metabolic imbalances and reduce the burden on the kidneys. Key aspects include:
- Sodium Control: Restricting sodium intake helps manage fluid balance and blood pressure, a crucial consideration in ESRD.
- Phosphorus and Potassium Restriction: Dialysis patients need to limit phosphorus and potassium to prevent complications such as bone disease and heart problems.
- Protein Adjustment: Protein intake is tailored to individual needs, ensuring proper nutrition while avoiding excess waste buildup.
- Fluid Management: Controlling fluid intake is essential to prevent fluid overload and hypertension.
The benefits of adhering to the dialysis diet are numerous. It helps maintain electrolyte balance, prevent complications, reduce symptoms, and improve overall well-being.
Compliance with this diet is crucial to maximize the benefits of dialysis and minimize the risk of complications, making dietary changes a cornerstone in managing ESRD effectively.
Exercise and Kidney Health
Exercise plays a vital role in kidney health, particularly for individuals with End-Stage Renal Disease. While ESRD may pose physical limitations, there are several benefits to incorporating exercise into one's routine:
- Improved Cardiovascular Health: Regular exercise helps manage blood pressure and reduces the risk of cardiovascular disease, common in ESRD.
- Weight Management: Maintaining a healthy weight through exercise can reduce the strain on the kidneys and alleviate related complications.
- Enhanced Muscle Strength: Muscle strength is crucial for mobility and overall well-being, especially for individuals undergoing dialysis.
- Improved Mental Health: Exercise can alleviate symptoms of depression and anxiety, common among ESRD patients.
- Increased Energy Levels: Staying active can boost energy, allowing individuals to engage in daily activities and maintain a better quality of life.
While exercise is beneficial, it's essential to consult with healthcare providers to tailor a safe and effective exercise regimen to individual needs and limitations. The right exercise plan can play a significant role in improving kidney health, enhancing overall well-being, and promoting a healthier and more active life for ESRD patients.
Future Perspectives in the Treatment of Kidney Disease
The future of kidney disease treatment holds promise for improved prognoses, extended life expectancy, and innovative solutions in the management of End-Stage Renal Disease (ESRD). This section explores the exciting landscape of emerging treatments and cutting-edge technologies that are reshaping the way we approach kidney disease. From advancements in transplantation to novel therapies and wearable technologies, the future is bright for those seeking improved kidney health and enhanced quality of life.
Emerging Kidney Disease Treatments
Emerging kidney disease treatments and technologies hold the potential to revolutionize the management of kidney conditions. Some notable advancements include:
- Artificial Kidneys: Researchers are developing wearable or implantable artificial kidneys that could offer continuous dialysis, providing more convenience and a better quality of life for ESRD patients.
- Stem Cell Therapies: Stem cell research offers the hope of regenerating damaged kidney tissue, potentially reducing the need for transplants.
- Precision Medicine: Personalized treatment plans, based on a patient's genetic makeup, can enhance the effectiveness of treatments and reduce side effects.
- Remote Monitoring: Telehealth and wearable devices enable real-time remote monitoring, allowing healthcare providers to track kidney function and intervene promptly when necessary.
These innovations signify a brighter future for kidney disease management, offering the potential for more effective treatments, improved patient outcomes, and enhanced quality of life for those affected by kidney conditions.
Dialysis Advancements
The findings from the CONVINCE trial represent a significant breakthrough in the quest to enhance survival rates and quality of life for individuals battling End-Stage Kidney Disease (ESKD). This randomized, multicenter trial, involving 1360 patients over a 30-month period, demonstrated the substantial benefits of high-dose hemodiafiltration (HDF) over conventional high-flux hemodialysis.
HDF, with its enhanced ability to remove waste products and excess fluids, proved to be a game-changer. The improved survival rates observed suggest that this approach can be a more effective treatment option for ESKD patients. These results are not only medically significant but also offer renewed hope to those facing the challenges of ESKD, promising a future with extended life expectancy and a higher quality of life.
The CONVINCE trial underscores the importance of ongoing research and innovation in renal care, as it has the potential to reshape the landscape of ESKD treatment, improving patient outcomes and providing new avenues for managing this complex condition.
Frequently Asked Questions
The financial cost of managing End-Stage Renal Disease is substantial. In the United States, for instance, ESRD treatment, which often includes dialysis, transplant, and ongoing care, can incur high expenses. Medicare typically covers a significant portion of these costs, but individuals may still face out-of-pocket expenses, including premiums, copayments, and additional insurance costs.
The financial burden also extends to lost income due to treatment and potential job loss. Managing ESRD necessitates significant financial resources, making it essential for patients and their families to plan and seek financial assistance and support when available.
Yes, End-Stage Renal Disease can have profound emotional and psychological impacts. The chronic nature of the condition, the need for lifelong treatment, and the physical limitations can lead to feelings of depression, anxiety, and stress.
People with kidney failure often grapple with the emotional toll of managing ESRD, including adjusting to dietary restrictions, medication regimens, and concerns about mortality. Support from mental health professionals, support groups, and loved ones is crucial to address these emotional challenges and enhance the overall well-being of individuals living with ESRD.
End-Stage Renal Disease can significantly impact a patient's work or educational pursuits. The rigorous treatment regimen, including dialysis and frequent medical appointments, can disrupt work schedules and make it challenging to maintain a full-time job. Patients may also experience fatigue, reduced concentration, and physical limitations that affect their ability to perform in their educational or professional roles.
Some may need to reduce working hours or seek disability benefits. Flexible work arrangements and support from employers or educational institutions are vital for ESRD patients to balance their health needs with their work or educational commitments.
Balancing the demands of End-Stage Renal Disease treatment with other life responsibilities and relationships can be challenging. Open communication with loved ones and employers is crucial to establish support systems. Prioritizing self-care, adhering to treatment plans, and managing time effectively can help maintain a balance.
Seeking flexibility in work or educational arrangements, such as part-time or remote work, can accommodate treatment needs. Additionally, joining support groups or seeking professional counseling can provide emotional support and strategies to manage the physical and emotional aspects of ESRD while maintaining relationships and responsibilities.
End Stage Renal Disease Shouldn’t Mean It’s The End
End-Stage Renal Disease marks the most severe stage of Chronic Kidney Disease, profoundly affecting health and quality of life. Early detection, through kidney function tests and symptom recognition, is crucial for effective management. Kidneys play a vital role in maintaining overall well-being, and their damage disrupts essential functions.
Dialysis is a life-saving treatment for ESRD, alleviating symptoms and extending life expectancy, though it presents challenges. The patient experience is a delicate balance of relief and adjustment.
Kidney transplantation is the gold standard, but it involves rigorous eligibility criteria and lifelong post-transplant care. The journey is not without complications, making resilience and understanding key to navigating the complexities of ESRD and its management, ultimately leading to improved health and well-being.












I hadn't realized just how essential kidney dialysis was until I read this article. It states that dialysis is a life-saving procedure since it takes over the function of kidneys and filters toxins and waste from your blood. Is dialysis and outpatient procedure?
It's an outpatient procedure that may be done in the clinic or at home using specialized equipment.