Diet For Stage 4 CKD
As you navigate life with stage 4 chronic kidney disease (CKD), a kidney-friendly diet becomes a crucial part of your treatment plan. Your kidneys aren't working as they should, with an eGFR between 15-29 showing their significantly impaired function. What you eat can help manage your overall health, prepare you for potential dialysis or kidney transplant, and monitor vital albumin levels.
Keeping a close watch on sodium, potassium, and phosphorus intake, and customizing your kidney disease diet are key steps. It's not easy - dining out can be a minefield due to high sodium in restaurant food items - but it's doable with the right guidance.

Rely on advice from medical professionals such as a kidney doctor (nephrologist) and a dietitian to tailor-make a pre-dialysis healthy eating plan that suits you best and could even slow the progression of CKD. Remember, every bite counts when it comes to preserving your kidney health.
Jump to:
- Key Takeaways
- The Role of eGFR in Determining Kidney Function
- Managing Your Health and Diet in Stage 4 Kidney Disease
- The Importance of Albumin Levels in Kidney Health
- Managing Protein Intake at Stage 4 CKD
- Incorporating Vegetable and Starch Proteins or Plant-Based Proteins into Your Diet
- The Impact of Stress and Sleep on Kidney Health
- Customizing Your Diet Plan for Kidney Disease
- The Importance of Measuring Your Food Intake
- Limiting Protein and Sodium in Your Diet
- Sample CKD Stage 4 Meal Plan
- FAQs for Diet For Stage 4 CKD
- Planning Is Key To Stay On Top Of Stage 4 CKD
Key Takeaways
- Stage 4 CKD requires a proper kidney diet to manage the disease and prepare for dialysis if recommended by a nephrologist.
- Customizing a diet plan is important, with a focus on controlling protein intake, limiting sodium, and preparing meals at home.
- When eating out, it's important to be cautious and choose low-sodium options, avoid processed foods with high amounts of sodium, and ask for sauces and dressings on the side.
- Low-carb and low-potassium foods should be included in the diet, with a focus on low-protein options and limiting high-potassium fruits and vegetables.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
The Role of eGFR in Determining Kidney Function
Let's take a closer look at how eGFR plays a vital role in understanding your kidney function. The term eGFR (egfr blood test) stands for estimated Glomerular Filtration Rate, and it's crucial when determining the stage of chronic kidney disease (CKD). It measures the amount of blood filtered by your kidneys per minute.
Your kidney diet prescription is closely related to your eGFR and your percentage kidney function in people with kidney disease. Your eGFR is the amount of creatinine that your kidneys are filtering through. The lower it is, the higher the kidney disease stage you have.
Stage 1 = 90+ eGFR with other conditions like diabetes and heart disease
Stage 2 = 60 - 89 eGFR
Stage 3 = 30 - 59 eGFR (30-44 is close to Stage 4)
Stage 4 = 15 - 29 eGFR
Stage 5 = Below 15 eGFR (aka End Stage of Kidney Disease or End-Stage Renal Disease). On dialysis due to inability to function. Less than 10 % of kidneys are functional.
As you can see from above, your eGFR is fairly close to how well your kidneys are functioning. If you have about 20% kidney function left, you are likely in stage 4 kidney disease, and needing to really stick to a low protein diet.
You are probably feeling fatigued, having trouble with sleeping, and stress. Man, are you feeling a lot of stress.

Managing Your Health and Diet in Stage 4 Kidney Disease
Navigating your way through a diagnosis of Stage 4 kidney disease can feel overwhelming, but by focusing on maintaining your overall health and making healthier food choices, you're taking critical steps to manage the progression of kidney dysfunction.
One vital aspect is understanding dietary restrictions that come with this condition. The goal is to put less stress on your kidneys while ensuring you get enough nutrients.
This table gives a snapshot of some key points in managing your diet for kidney disease:
| Focus Area | Recommendation | Example |
| Meal Planning | Limit protein intake. Opt for low-sodium options and restrict high-potassium foods. Prepare meals at home. | Use quinoa, noodles or rice for added proteins. Choose low-sodium sauces and dressings. |
| Delicious Recipes that are Kidney-Friendly | Incorporate vegetable and starch proteins into meals. Experiment with nut flours like almond flour or coconut flour. | Try kidney-friendly smoothies using spinach, cucumber, apple and mint leaves. Bake using almond flour instead of regular wheat flour. |
| Nutritional Supplements and Lifestyle Modifications | Stick to prescribed medications and supplements as advised by healthcare providers. Incorporate lifestyle modifications such as regular exercise. | Take vitamin D supplements if suggested by doctors; engage in light activities like walking or yoga regularly |
Following these guidelines will not only help you deal with kidney disease but also improve your overall well-being over time.
The Importance of Albumin Levels in Kidney Health
Keeping an eye on your albumin levels is crucial when it comes to managing your kidney health. Albumin, a protein produced by the liver, serves multiple functions in the body.
Within the context of renal health, its primary role is to maintain fluid balance and transport substances throughout the bloodstream.
In relation to kidney function, albumin levels act as a significant marker for kidney well-being. When kidneys are functioning well, they keep the right amount of albumin in the blood while filtering out wastes.
However, with kidney disease progression, especially in advanced kidney disease, these filters can be damaged leading to albumin leakage into urine - a condition known as 'albuminuria'.
Albuminuria not only indicates deteriorating kidney function but also accelerates CKD progression. Hence monitoring and maintaining optimal albumin levels becomes imperative in your fight against CKD. Consuming adequate protein from sources like vegetable proteins or starches can help preserve healthy albumin levels without overworking your kidneys.
Your journey towards better renal health should prioritize keeping track of this key biomarker – because understanding and acting upon your albumin levels could make a world of difference in managing CKD effectively (managing your kidney disease).
Managing Protein Intake at Stage 4 CKD
At stage 4 Chronic Kidney Disease (CKD), the kidneys' function is significantly impaired, and managing protein intake becomes crucial to support kidney health while maintaining overall nutrition. The Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines recommend restricting protein intake to slow down the progression of kidney damage and reduce the accumulation of waste products.
In this stage, individuals are often referred to a registered dietitian who specializes in kidney disease management to develop a personalized nutrition plan. The dietitian will consider the person's age, weight, muscle mass, and other medical conditions while setting the protein allowance.
Typically, high-quality protein sources with essential amino acids, such as lean meats, poultry, fish, and eggs, are preferred as they produce fewer waste products during metabolism. However, the total protein intake is often limited to around 0.6 to 0.8 grams of protein per kilogram of body weight per day.
In some cases, a low-protein diet may be necessary, but this should be carefully balanced to prevent malnutrition and muscle loss. Nutritional supplements may be recommended to ensure adequate vitamin and mineral intake.
Regular monitoring of kidney function, nutritional status, and fluid balance is essential for adjusting the protein intake as the disease progresses. Managing other aspects of the diet for kidney disease, such as sodium, phosphorus, and potassium, is equally vital in supporting kidney health and overall well-being.
Adherence to the recommended diet and regular follow-ups with healthcare team and knowing the best treatment options can help slow the progression of CKD and improve the quality of life for those in stage 4.
Incorporating Vegetable and Starch Proteins or Plant-Based Proteins into Your Diet
Incorporating more vegetable and starch proteins (plant-based proteins) into your meals can be a game-changer for your kidney health. Rather than relying solely on animal-based proteins, consider vegetarian options such as beans, lentils or tofu. These protein alternatives are not only beneficial for the kidneys but also provide additional nutrients like fiber.
Here's a handy table to help you get started:
| Vegetable Proteins | Starch Proteins |
| Tofu | Quinoa |
| Lentils | Brown rice |
| Chickpeas | Whole grain bread |
| Spinach | Oats |
| Broccoli | Sweet potatoes |
Incorporating starch proteins is equally essential. Food items like quinoa (is quinoa good for kidney disease) and brown rice are excellent sources of plant-based proteins while also being rich in fiber and low in sodium, perfect for a kidney-friendly diet.
Remember, the goal here isn't to eliminate animal protein entirely but to balance it with plant-based ones. Consult with your healthcare professional or a dietitian before making significant changes to your diet.
By incorporating vegetable and starch proteins into your meals, you're taking an empowering step towards managing stage 4 CKD while nourishing yourself holistically.
The Impact of Stress and Sleep on Kidney Health
Balancing the demands of daily life, you might overlook how stress and inadequate sleep can significantly impact your kidney health. The effects on kidneys of extra stress can exacerbate stage 4 Chronic Kidney Disease (CKD) by increasing blood pressure levels. This heightened blood pressure can put additional strain on your kidneys, compromising their function even further.
The quality of sleep you get is equally important. Sleep disorders like obstructive sleep apnea are common in individuals with CKD and can lead to high blood pressure (high blood pressure and kidney disease) and heart disease, both of which negatively impact kidney function.
Investing time in self-care through effective stress management techniques is crucial for maintaining optimal kidney health. Deep breathing exercises, yoga, or even a simple walk outdoors can help reduce stress levels substantially.
To improve your sleep quality, establish a regular bedtime routine, limit caffeine intake especially towards the evening, and maintain a quiet and comfortable sleeping environment.
Always remember that managing your diet isn't the only aspect vital to your renal health; addressing emotional wellbeing and ensuring adequate restorative sleep play significant roles in kidney health and heart health too. Incorporating these lifestyle modifications alongside dietary changes will provide comprehensive care for your kidneys during this critical period.
Customizing Your Diet Plan for Kidney Disease
Customizing a proper kidney diet plan for individuals with stage 4 Chronic Kidney Disease (CKD) is an essential part of the treatment plan to manage their condition effectively and improve overall health.
Through the kidney disease stages, there could be some changes in the proper kidney diet over time.
Hence, a personalized diet plan takes into account the dietary restrictions and the person's unique medical history, personal health factors, kidney function, nutritional needs, and lifestyle. Here are some key considerations:
- Low Protein Diet: As kidney function declines, protein intake must be adjusted to avoid excessive waste product accumulation. A registered dietitian will determine the appropriate amount of high-quality protein sources to maintain muscle mass and prevent malnutrition.
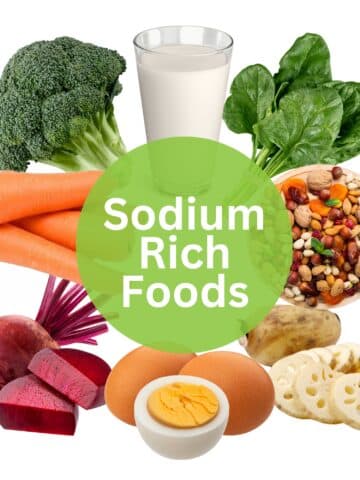
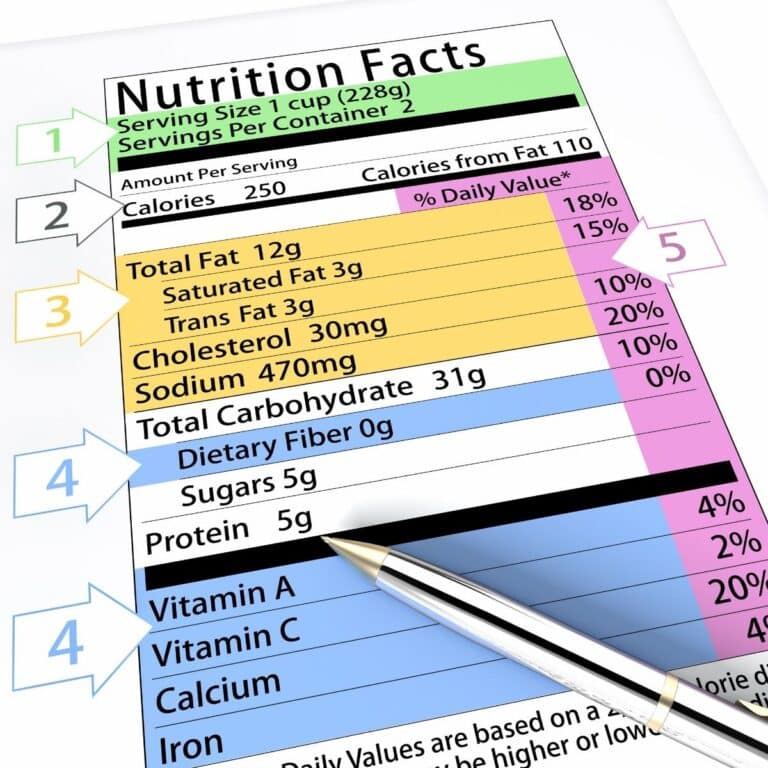
- Sodium Control: Limiting sodium intake helps manage blood pressure and fluid retention. Processed and packaged foods, which are often high in sodium, should be avoided, and instead, fresh foods and homemade meals are recommended. Make sure to read nutrition labels to see the amounts of sodium in each food item you buy.
- Phosphorus and Potassium Management: Foods rich in phosphorus and potassium should be controlled, as these minerals can accumulate in the blood with reduced kidney function. Dairy foods, nuts, seeds, and some fruits and vegetables may be restricted. Look out for anything with "phos" in the nutrition facts labels which you should avoid in keeping with your phosphorus restrictions.
- Fluid Balance: Fluid intake needs to be carefully monitored to prevent fluid overload. A dietitian will advise on the appropriate amount of fluid intake based on individual needs and urine output.
- Individual Tolerance: A diet plan must consider any food intolerances or allergies the person may have, ensuring they can follow the diet safely and comfortably.
- Nutritional Supplementation: In some cases, nutritional supplements may be recommended to fill in nutrient gaps and prevent deficiencies.
- Regular Monitoring: Periodic assessment of kidney function, nutritional status, and compliance with the diet plan is crucial. The dietitian will make adjustments as necessary based on the person's progress and changing needs.
Collaboration between the individual, healthcare professionals, and the dietitian is vital to ensure that the dietary approaches are well-tailored to the person's specific needs, and it helps slow down the progression of kidney disease, manage symptoms, and improve their quality of life.
The Importance of Measuring Your Food Intake
Don't underestimate the power of portion control, as it's a crucial part of managing your kidney health in stage 4 CKD. Measuring portions accurately can help you keep track of your protein, sodium, and potassium intake – all vital for maintaining optimal kidney function.
One effective food measurement technique is using kitchen scales to weigh your meals. This gives you an accurate understanding of how much food you're consuming daily. It's especially important when tracking food intake for high-protein foods like meat or fish.
For example, a portion size guideline might suggest that only around 3-4 ounces (about the size of a deck of cards) should be consumed per meal.
Another approach is employing portion control tips such as using smaller plates and bowls to naturally limit portion sizes. Visual cues can also be helpful - consider a tennis ball-sized serving for fruits and vegetables, or a small fist for rice or pasta servings.
Remember, every bite counts when you're focusing on renal health management. By regularly measuring portions and tracking your food intake meticulously, you're taking proactive steps towards slowing down disease progression while supporting overall wellbeing – demonstrating true commitment to self care and better health outcomes.
Limiting Protein and Sodium in Your Diet
Limiting sodium intake is a crucial aspect of a kidney friendly diet for individuals with stage 4 Chronic Kidney Disease (CKD) to manage blood pressure and fluid balance effectively. Here's why and how sodium restriction is emphasized:
- Blood Pressure Control: High sodium levels can cause the body to retain more water, leading to increased blood volume and higher blood pressure. Elevated blood pressure can further damage the kidneys and worsen CKD as well as affect heart health. By limiting sodium intake, blood pressure can be better controlled, reducing the strain on the kidneys.
- Fluid Balance: Sodium plays a significant role in regulating the body's fluid balance. When sodium intake is high, it can lead to fluid retention, causing swelling (edema) in the legs, ankles, and around the eyes. In CKD, impaired kidney function makes it harder for the body to remove excess fluid, making sodium restriction even more crucial to manage fluid levels (fluids to hydrate with kidney disorder).
- Kidney Function Preservation: By reducing sodium intake, the kidneys' workload is lessened, which can help preserve their function and slow down the progression of CKD.
To limit intake of sodium in a kidney friendly diet for stage 4 CKD:
- Avoid processed such as frozen dinners and canned soups and other types of foods with excess levels of sodium. Opt for fresh foods and delicious meals made from scratch instead (Low Sodium Canned Foods For CKD).
- Pay attention to sodium levels in foods you buy. Read food labels and choose those with lower amounts of salt.
- Minimize the use of salt during cooking and at the table. Instead, use herbs, spices, lemon juice, or vinegar to add flavor in making delicious meals.
- Be cautious of high-sodium condiments, sauces, and seasoning mixes.
- Limit consumption of salty snacks, such as chips, pretzels, and salted nuts.
Working closely with a registered dietitian or healthcare provider is essential to develop a personalized kidney-friendly eating plan that addresses dietary restrictions when it comes to salt intake while ensuring proper nutrition and overall well-being.
Careful monitoring of blood pressure and fluid balance can help assess the effectiveness of the sodium restriction and guide any necessary adjustments to the food plan. Periodic blood tests as recommended by your kidney doctor can also help determine any abnormalities that warrant prompt medical attention.
Sample CKD Stage 4 Meal Plan
Please note that creating a sample meal plan for patients with stage 4 CKD requires careful consideration of their specific medical condition, nutritional needs, and any other medical issues they may have.
It's crucial to consult a registered dietitian or healthcare provider to develop a personalized food plan. However, here's a general sample kidney-friendly eating plan that emphasizes protein and sodium restrictions:
Breakfast:
- Egg white omelet with spinach and tomatoes (low in phosphorus)
- 1 slice of whole-grain toast (low-sodium)
- 1 small serving of fresh fruit (e.g., berries or apple slices)
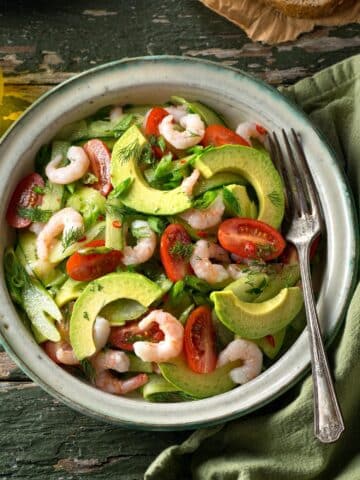
Lunch:
- Grilled chicken or turkey breast (portioned to fit protein needs)
- Mixed green salad with cucumber, bell peppers, and a low-sodium vinaigrette
- Quinoa or brown rice (limited portion for phosphorus control)
Snack:
- Low-fat Greek yogurt (portioned for protein needs)
- Carrot sticks or celery (low in sodium)
Dinner:
- Baked or broiled fish (e.g., salmon or cod) seasoned with herbs and lemon (low-sodium)
- Steamed asparagus (limited portion for phosphorus control)
- Mashed sweet potatoes (limited portion for potassium control)
Dessert (if allowed):
- A small serving of low-sodium, low-phosphorus dessert (e.g., a fruit sorbet)
Remember that individual dietary needs may vary, and this sample food plan is not a substitute for personalized medical advice. A registered dietitian can adjust your healthy eating plan based on an individual's specific lab results, medical history, and lifestyle to optimize kidney health and overall well-being.
FAQs for Diet For Stage 4 CKD
In Stage 4 CKD, the consumption of animal protein can have a significant impact on kidney function. Animal protein intake increases the workload on the kidneys, as it produces more waste products that need to be filtered out. This can further stress the already compromised kidneys, potentially accelerating the progression of kidney damage.
Animal protein can also raise the levels of certain substances like phosphorus and uric acid, which can be harmful to the kidneys. Reducing the consumption of animal protein and opting for high-quality, low-phosphorus sources can help alleviate the strain on the kidneys and support kidney health in Stage 4 CKD.
In late stage kidney disease, certain foods and supplements may not improve kidney function, as the damage to the kidneys is generally irreversible. However, a well-balanced healthy diet that is low in sodium, phosphorus, and potassium can help manage symptoms and slow down disease progression.
Some supplements like vitamin D or iron may be prescribed to address specific deficiencies. It's crucial to consult with a health care provider or registered dietitian before making any dietary changes or starting supplements to ensure they are safe and appropriate for individual health conditions.
In late stage CKD, impaired kidney function can lead to an accumulation of potassium and phosphorus in the blood, known as hyperkalemia and hyperphosphatemia, respectively. High potassium levels can cause irregular heart rhythms and be life-threatening. Elevated levels of phosphorus can cause bone disease through bone mineral loss, damage blood vessels, and worsen kidney function.
Restricting dietary intake of potassium and phosphorus is essential to prevent these complications. Food items high in potassium and phosphorus, such as certain fruits, vegetables, dairy products, and processed foods, should be limited. Working with a dietitian to develop a healthy diet plan is crucial to normal blood levels and support kidney health (why do you need a pre-dialysis diet plan?).
Some easy-to-make, kidney-friendly lunch options for someone with Stage 4 CKD include:
1. Grilled chicken or turkey breast salad with mixed greens and low-phosphorus vegetables.
2. Quinoa or brown rice bowl with cooked vegetables, lean protein (e.g., fish or tofu), and a low-sodium sauce.
3. Egg white omelet with spinach and low-potassium vegetables.
4. Low-sodium tuna or chicken salad with lettuce wraps or whole-grain bread. 5. Vegetable and bean soup with limited sodium and potassium.
5. Pasta or noodle salad with kidney-friendly vegetables and a low-phosphorus dressing.
6. Baked sweet potato with a small portion of low-sodium protein (e.g., chicken or turkey).
Remember to consult with a dietitian for personalized meal planning that meets individual nutritional needs and restrictions.
Managing both diabetes and Stage 4 CKD requires careful dietary planning. An individualized kidney disease diet that balances blood glucose levels and supports kidney health is essential. Focus on key foods with low glycemic index to control blood glucose levels, and limit carbohydrates to manage diabetes.
Opt for kidney-friendly food without salt or excess sodium levels, as well as low phosphorus foods, and low potassium food options to support kidney function.
Work with a registered dietitian to develop a personalized kidney friendly eating plan, monitor blood glucose levels and kidney function regularly, and adjust the kidney disease diet as needed.
Proper medication management, blood sugar level monitoring, food exercise habits depending on your activity level, and close communication with health care providers are also crucial for overall health management and switching to a healthy lifestyle.
Planning Is Key To Stay On Top Of Stage 4 CKD
You will find plenty of options for help with your dialysis kidney friendly diet, because Medicare reimbursement allows you to see a dietitian and get more help. You are pre-dialysis, and you need to know your kidney disease diet and how you fit in.
You are at a point of needing to seriously measure the amount of food that you eat if you want to stop your kidney disease progression. I'm not saying that you can stop it, but to have a chance you should control the amount of food you eat as far as protein is concerned. Stick to a plan of 40-60 grams of protein per day. That is only about 2 ounces of beef, pork or poultry per meal. That is not much. And limit your sodium. At this point you are making your meals at home.
Life with stage 4 CKD or any late stage kidney disease for that matter is not easy but, if you are serious about trying to slow down your kidney disease progression (ckd progression), you will need to get a pre-dialysis kidney friendly eating plan and stick to it. It's one of the best ways to make it through this tough time.











THE DR. JUST INFORMED ME THAT MY KIDNEY FUNCTION DROPPED 7 POINTS I'AM A 3-4 STAGE KIDNEY DISEASE. HE HAD TOLD ME THAT I COULD EAT ANYTHING EXCEPT HAMBURGER. NOW HE TELL'S ME NOT TO EAT PORK, HAM, HOT DOGS LUNCH MEAT. WATCH MY SALT AND DRINK MORE WATER. AS I DRINK TEA COFFEE, COLD ICE TEA SODA ONCE IN A WHILE SO I CAN HAVE SOMETHING DIFFERENT. I REALLY DO NOT KNOW WHAT TO EAT OR DRINK, AS I'VE BEEN EATING A LOT OF PROCESSED FOOD. I'M BESIDE MYSELF. CAN YOU PLEASE HELP.
Why did I not hear about this type of diet other than by my own research? I started out at mid-Stage 3 and I went to Stage Four and now I am starting to enter Stage 5. My doctor (a nephrologist here in VA) talks about weight loss and soidum restriction but has never mentioned the other parts of the diet nor has he referred me to a renal dietician, which my insurance would cover.
He goes on about exercise but I have told him I usually am too tired to exercise. I might be able to swim if I could find a heated pool but I am stuck using public transportation and in my area finding a pool I can access with hours (weekends, after work on weekdays) I can attend seems impossible.
I am 63, work full time (and many times OT!) and in addition have Hepatitis C and am plagued by Fibromyalgia. And I do not want to do dialysis.