Why Do I Need A Pre Dialysis Diet
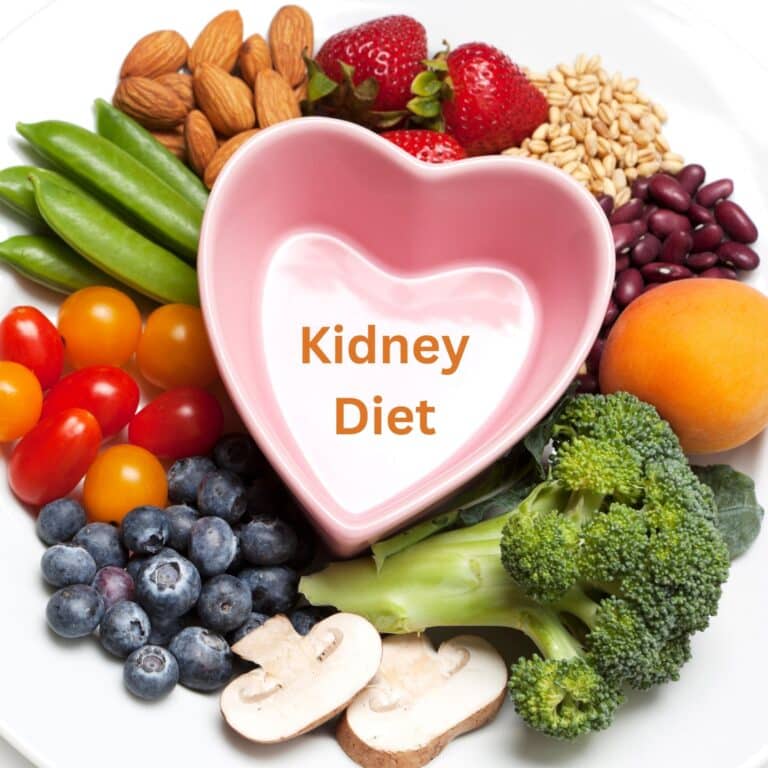
A pre-dialysis kidney diet plays a crucial role in the well-being of individuals diagnosed with chronic kidney disease (CKD). As kidneys gradually lose their ability to filter waste and excess fluids from the blood, adopting a specialized diet becomes essential to manage the progression of the disease (ckd progression) and maintain overall health.
This dietary approach aims to control the intake of certain nutrients, such as sodium, potassium, phosphorus, and protein, which can accumulate in the bloodstream when kidney function declines.
By adhering to a pre-dialysis diet, patients can help alleviate the strain on their kidneys, manage blood pressure, and prevent complications like fluid retention and electrolyte imbalances.

Understanding the significance of a pre-dialysis diet empowers individuals to actively engage in their healthcare journey, enhancing their quality of life and potentially delaying the need for dialysis treatment or transplantation.
Jump to:
- Key Takeaways
- Understanding the Need for a Renal Pre-Dialysis Diet
- The Role of Blood Urea Nitrogen (BUN) in Kidney Health
- Other Indicators of Kidney Function
- The Impact of Protein Intake on BUN Levels
- Adjusting to Dietary Needs in Pre-Dialysis Stage
- The Importance of Fluid Intake in Pre-Dialysis Diet
- Limiting Salt Intake in a Renal Pre-Dialysis Diet
- The Role of Whole Grains in a Renal Pre-Dialysis Diet
- How Much Protein Should You Eat on a Renal Pre-Dialysis Diet?
- The Importance of Planning Ahead Through the Progression of Kidney Disease and Dietary Adjustments
- FAQs for Renal Pre-Dialysis Diet
- A Pre-Dialysis Diet Can Significantly Impact Your CKD Progression
Key Takeaways
- A renal pre-dialysis diet is crucial for managing declining kidney function, alleviating stress on compromised kidneys, and preventing complications associated with chronic kidney disease (CKD).
- Monitoring Blood Urea Nitrogen (BUN) levels is essential for assessing kidney health in patients with kidney disease, as elevated levels can indicate impaired kidney function and the accumulation of waste products.
- Multiple indicators beyond BUN, such as creatinine, Glomerular Filtration Rate (GFR), electrolyte levels, albumin in urine, and hemoglobin, provide a comprehensive picture of kidney health, guiding treatment decisions and dietary adjustments.
- Protein intake significantly influences BUN levels and kidney strain. Pre-dialysis kidney patients should manage protein intake to balance nutritional needs and kidney health, with individualized dietary plans tailored to their specific requirements.
- Planning ahead through disease progression and dietary adjustments empowers pre-dialysis renal patients to make informed food choices, manage complications, and potentially delay the need for dialysis treatment or transplantation, enhancing overall quality of life.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding the Need for a Renal Pre-Dialysis Diet
Why do you need a pre-dialysis diet plan? A renal pre-dialysis diet is imperative for individuals grappling with declining kidney function due to its pivotal role in mitigating complications and optimizing overall health. Kidnxeys, essential organs responsible for filtering waste and maintaining fluid-electrolyte balance, gradually lose efficiency in cases of chronic kidney disease.
A specialized pre-dialysis diet becomes necessary to alleviate stress on compromised kidneys. By controlling intake of specific nutrients like sodium, potassium, phosphorus, and protein, renal patients can prevent their accumulation in the bloodstream and subsequent harm to the body.
High sodium intake can exacerbate hypertension, a common complication of CKD, leading to cardiovascular strain. Excess potassium can disrupt heart rhythm and cause muscle weakness, while heightened phosphorus levels contribute to bone issues.
Meanwhile, excess protein can further strain weakened kidneys. A pre-dialysis diet tailored to individual needs curbs these risks, helping maintain blood pressure, electrolyte balance, and bone health.
Moreover, adopting a pre-dialysis diet fosters patient empowerment by enabling active participation in managing their condition. As CKD progresses, adhering to dietary guidelines can delay the need for dialysis or transplantation, enhancing quality of life.
In essence, a renal pre-dialysis diet is pivotal in promoting well-being, preserving kidney function, and averting complications, thereby underscoring its indispensable role in the holistic management of chronic kidney disease.
The Role of Blood Urea Nitrogen (BUN) in Kidney Health
Blood Urea Nitrogen (BUN) serves as a crucial indicator of kidney health, particularly for people with kidney disease, offering valuable insights into renal function and overall well-being.
BUN is a waste product resulting from protein metabolism, and its levels in the bloodstream are primarily regulated and eliminated by the kidneys. In pre-dialysis patients, whose kidney function is compromised due to conditions like chronic kidney disease, monitoring BUN levels becomes pivotal.
Elevated BUN levels often signify reduced glomerular filtration rate, indicating impaired kidney function. For people with kidney disease, high BUN levels might suggest a decline in the kidney's ability to effectively remove waste products from the body.
This can lead to the accumulation of toxins in the bloodstream, potentially causing various complications like nausea, fatigue, and cognitive impairment. Moreover, elevated BUN levels can also indicate dehydration or excessive protein intake, further straining compromised kidneys.
Regular monitoring of BUN levels assists health professionals in assessing the progression of kidney disease and tailoring interventions accordingly. This might involve adjusting dietary protein intake, managing fluid balance, and considering potential medical treatments to prevent further deterioration.
By understanding the role of BUN in kidney health, pre-dialysis patients can actively engage in their care, making informed choices to optimize kidney function and overall quality of life.
Other Indicators of Kidney Function
Beyond Blood Urea Nitrogen, several other indicators play a pivotal role in evaluating kidney function, providing comprehensive insights into renal health for people with kidney problems.
Creatinine, another waste product generated by muscle metabolism, serves as a key marker. Elevated creatinine levels suggest reduced glomerular filtration rate, highlighting compromised kidney function.
Glomerular Filtration Rate (GFR) itself is a vital measure, indicating the kidneys' ability to filter waste from the blood. A decreasing GFR signifies declining kidney function.
Electrolyte levels, particularly potassium and sodium, are crucial indicators. Potassium imbalances can impact heart rhythm, while sodium levels relate to fluid balance and blood pressure control. Abnormal levels can signal kidney dysfunction. Phosphorus, often elevated in kidney disease, can impact bone health and require monitoring.
Albumin in urine is a marker for protein leakage, suggesting impaired kidney filtration. High albumin levels indicate potential damage to the kidney's filtering units.
Hemoglobin levels, indicating red blood cell health, are monitored as kidney dysfunction can lead to anemia due to reduced production of erythropoietin, a hormone necessary for red blood cell production.
Collectively, these indicators provide a comprehensive picture of kidney health, guiding treatment decisions, dietary adjustments, and lifestyle modifications for pre-dialysis patients. Regular monitoring and interpretation of these markers are essential in managing chronic kidney disease and maintaining overall well-being.
The Impact of Protein Intake on BUN Levels
Check out the protein for CKD Patients by stage. Protein intake plays a significant role in influencing Blood Urea Nitrogen levels, particularly in individuals with compromised kidney function such as pre-dialysis patients. BUN is a byproduct of protein metabolism, and its levels in the blood can be affected by the amount of protein consumed.
In people with kidney problems, the kidneys' ability to filter waste products like urea becomes compromised. When protein is consumed, it is broken down into amino acids, which are eventually metabolized into urea.
Higher protein intake can lead to increased urea production, raising BUN levels in the bloodstream. This can place additional stress on already weakened kidneys, potentially exacerbating the progression of kidney disease.
Health professionals often recommend carefully managing protein intake for pre-dialysis patients to strike a balance between meeting nutritional needs and minimizing kidney strain.
Adequate protein intake is essential for maintaining muscle mass and overall health, but excessive protein consumption can lead to higher BUN levels, contributing to symptoms like nausea, fatigue, and complications related to kidney dysfunction.
Protein is in a lot of foods. Protein is (obviously) meat, pork, chicken, veal, and turkey. Protein is also a part of pastas as well. It’s in bread, vegetables, milk, cheese and a lot of other things.
Now that you have some kidney problems you need to limit the amount of protein. Not necessarily a lot, but it will affect you as you work on your renal pre-dialysis diet. As you progress from one stage of kidney disease to the next, you will have different amounts of protein that you need.
Kidneys are sensitive to protein, and as your body progresses through kidney disease, you may need to eat more or less. As you progress from earlier stages to later stages of kidney disease, you decrease the amount of protein that you need. Then, when you become a kidney dialysis patient (if you do), you get to go back to a higher amount of protein.
Individualized dietary plans that consider the patient's protein needs, kidney function, and overall health status are crucial. Monitoring BUN levels alongside protein intake helps healthcare providers tailor dietary recommendations to optimize both nutritional intake and kidney function, ultimately enhancing the well-being of pre-dialysis patients.
Adjusting to Dietary Needs in Pre-Dialysis Stage
Navigating the changes in your eating habits during this phase of kidney disease can indeed be a challenge, but remember, each carefully considered food choice contributes to preserving your overall health and slowing disease progression. It's all about balance, and learning to cope with dietary restrictions is a crucial part of managing kidney disease pre-dialysis.
One way to make these changes more manageable is by incorporating stress management techniques into your daily routine. This could involve meditation, deep-breathing exercises, or yoga. Exercise also plays an important role - not only does it help you maintain a healthy weight, but regular physical activity can also improve energy levels and mood.
Remember the importance of hydration, while you may need to monitor fluid intake based on the doctor's advice, staying adequately hydrated is key for overall health. When it comes to food choices, think color, incorporating fruits and vegetables into your diet enhances nutrition without adding undue strain on your kidneys.
Making these lifestyle adjustments won't always be easy, but know that every step you take brings you closer to maintaining kidney function as long as possible.
The Importance of Fluid Intake in Pre-Dialysis Diet
Fluid intake management holds immense importance in the pre-dialysis diet for individuals with compromised kidney function. Kidneys play a central role in maintaining fluid and electrolyte balance within the body, but in pre-dialysis patients, this balance can become disrupted. Thus, monitoring and controlling fluid intake becomes crucial to prevent complications.
Kidneys struggling with reduced function may struggle to regulate fluid levels effectively, leading to fluid retention and potential edema. Excessive fluid intake can strain the heart and exacerbate hypertension, both common complications of kidney disease. Moreover, retained fluids can contribute to shortness of breath and swelling, diminishing the patient's quality of life.
Conversely, inadequate fluid intake (fluid restriction diet) can lead to dehydration, causing electrolyte imbalances and even further kidney stress. For instance, concentrated levels of waste products like BUN and creatinine can build up in the bloodstream due to insufficient fluid to flush them out.
A well-managed fluid intake, tailored to the individual's needs and guided by medical professionals, helps maintain a delicate balance, mitigating complications and supporting kidney health.
By adhering to recommended fluid restrictions, pre-dialysis patients can improve blood pressure control, prevent edema, and enhance overall well-being, contributing to a more favorable trajectory in managing their kidney condition.
Limiting Salt Intake in a Renal Pre-Dialysis Diet
Limiting salt (sodium) intake is a fundamental aspect of a renal pre-dialysis diet due to its significant impact on kidney health. Excess sodium can lead to fluid retention and elevated blood pressure, exacerbating the strain on already compromised kidneys. Pre-dialysis patients should aim to reduce salt intake to manage these risks.
Foods high in sodium should be avoided or minimized. Processed and packaged foods, such as canned soups, deli meats, and fast food, often contain excessive salt. Pickled foods, salty snacks, and condiments like soy sauce and ketchup also contribute to sodium intake. Ready-to-eat meals and restaurant dishes may hide high sodium content as well.
Instead, pre-dialysis patients should opt for fresh, whole foods and cook at home to have better control over salt levels. Using herbs, spices, lemon juice, and vinegar can enhance flavor without relying on excess salt. Reading food labels is essential to identify hidden sources of sodium in food products. It's vital to read labels carefully as a kidney patient.
By limiting salt intake, pre-dialysis patients can manage blood pressure, reduce fluid retention, and support overall kidney health. Incorporating a variety of low-sodium, nutrient-rich foods can improve their well-being and potentially delay the need for dialysis or transplantation, offering a proactive approach to managing their kidney condition.
The Role of Whole Grains in a Renal Pre-Dialysis Diet
Whole grains play a significant role in a renal pre-dialysis diet due to their numerous health benefits and their potential to support kidney function.
Unlike refined grains, whole grains are rich in fiber, vitamins, minerals, and antioxidants, which are vital for overall health and can be particularly advantageous for individuals with compromised kidney function.
Whole grains contribute to stable blood sugar levels, which is essential for managing conditions like diabetes often associated with kidney disease. Their high fiber content aids digestion, promotes regular bowel movements, and may help lower cholesterol levels.
Additionally, the nutrients in whole grains can support heart health, crucial for pre-dialysis patients who are at a higher risk of cardiovascular complications.
When choosing whole grains for a renal pre-dialysis diet, it's important to consider phosphorus content, as elevated levels can strain the kidneys. Opt for lower phosphorus whole grains like brown rice, quinoa (quinoa renal diet), bulgur, and whole wheat pasta. By incorporating these grains into meals, pre-dialysis patients can receive essential nutrients while minimizing the burden on their kidneys.
Incorporating whole grains as part of a balanced diet can enhance the overall well-being of pre-dialysis patients, providing a source of energy, fiber, and nutrients that contribute to better blood sugar control, heart health, and digestive function, ultimately supporting the management of their kidney condition.
How Much Protein Should You Eat on a Renal Pre-Dialysis Diet?
On a renal pre-dialysis diet, the amount of protein you should consume is a crucial consideration to support kidney health while meeting your nutritional needs. A common recommendation for individuals with chronic kidney disease (CKD) is to follow a low-protein diet, typically ranging from 0.6 to 0.8 grams of protein per kilogram of body weight per day.
How much protein should you eat – probably in the range of 60-80 grams per day. You might want to know that one ounce of protein contains 7 grams of protein. So, that’s 5-8 ounces per day of meat. Well, if only it were that simple.
In any case, this controlled protein intake helps reduce the buildup of waste products like urea, which can strain compromised kidneys (how to reduce stress naturally). As discussed, consuming excessive protein can lead to higher levels of Blood Urea Nitrogen and other waste products, potentially worsening kidney function.
It's essential to consult with a healthcare professional or registered dietitian to determine the appropriate protein intake based on your specific health status, kidney function, and other individual factors. They can help you calculate your protein needs and develop a dietary plan that provides adequate protein while minimizing stress on your kidneys.
In addition to protein quantity, the quality of protein matters. Choosing high-quality protein sources like lean meats, poultry, fish, eggs, and plant-based options such as beans and lentils can provide essential amino acids without overburdening the kidneys.
Balancing protein intake is a vital component of a renal pre-dialysis diet, promoting kidney health while maintaining overall nutritional well-being.
The Importance of Planning Ahead Through the Progression of Kidney Disease and Dietary Adjustments
Planning ahead for the anticipated progression of kidney disease and dietary adjustments can offer significant benefits for pre-dialysis chronic kidney disease patients.
As CKD advances, the kidneys' ability to filter waste and regulate fluid and electrolytes diminishes, necessitating proactive dietary management to preserve kidney function and overall health.
By engaging in early discussions with healthcare professionals and registered dietitians, patients can tailor their dietary choices to their specific stage of CKD (renal diet restrictions by stage of CKD).
This proactive approach enables gradual adjustments to the intake of nutrients like protein, sodium, potassium, and phosphorus, avoiding sudden and drastic changes that could strain the kidneys.
Planning ahead also empowers patients to make informed food choices that align with their individual needs, preferences, and cultural considerations. Monitoring key indicators like blood pressure, BUN levels, and estimated glomerular filtration rate (eGFR) helps track disease progression and inform timely dietary modifications.
Anticipating the progression of kidney disease allows pre-dialysis CKD patients to better manage complications, such as fluid retention and electrolyte imbalances, leading to improved quality of life. This approach may even delay the need for dialysis or transplantation.
In essence, by being proactive and informed, patients can take charge of their health journey, making strategic dietary adjustments to support kidney function and overall well-being.
FAQs for Renal Pre-Dialysis Diet
Managing potential discomfort or side effects of a renal pre-dialysis diet involves several strategies. Stay hydrated within your recommended limits, as dehydration can exacerbate complications.
Gradually adapt to dietary changes to avoid sudden discomfort. Consult a registered dietitian to create a balanced meal plan that meets your nutritional needs while adhering to restrictions.
Monitor your body's response to foods and adjust portions accordingly. Engage in stress-relief techniques like meditation and gentle exercise to support your overall well-being. Regularly communicate with healthcare professionals to address any concerns promptly.
Remember that the journey requires patience; seek support from peers or support groups to share experiences and coping strategies.
For a renal pre-dialysis diet, focus on low-sodium, low-potassium, and controlled protein meals. Start your day with oatmeal topped with berries and a sprinkle of cinnamon. Lunch could feature a spinach and quinoa salad with grilled chicken breast, cucumbers, and a lemon vinaigrette.
For dinner, try baked salmon with steamed asparagus and a side of brown rice. Snack options include apple slices with almond butter or a small handful of unsalted nuts. Remember to consult a dietitian for personalized recipes and portion recommendations to suit your specific dietary needs and kidney health goals.
Are you learning how to improve bun level? Understanding the importance of your BUN levels is crucial when managing kidney health on a pre-dialysis diet. Regular monitoring has several benefits. It helps you track the impact of your diet on BUN levels, detect any fluctuations early, and make necessary adjustments to your diet.
It's recommended to check your BUN levels every few months or as advised by your health care provider. Interpreting BUN results can be complex, so always discuss them with your doctor to understand what they mean for you.
Why low protein diet in kidney disease? Yes, there is a difference between animal and plant proteins in a renal pre-dialysis diet. Your protein sources matter in this type of diet. Animal proteins have been found to increase BUN levels more than plant proteins.
Therefore, dietary adjustments are necessary to prioritize plant proteins for their beneficial properties such as fiber and lower phosphorus values.
In contrast, animal proteins have higher phosphorus content, which can be a drawback for kidney health. It is important to remember that in a kidney diet for pre-dialysis patients, it is not only about limiting protein intake but also about selecting the appropriate types of protein to promote better kidney health.
A pre-dialysis kidney friendly diet can have a significant impact on health conditions like diabetes and hypertension. By managing sodium, potassium, and phosphorus intake, the diet helps control blood pressure and fluid balance, crucial for hypertension management. Additionally, monitoring carbohydrates and including whole grains supports blood sugar control for diabetes.
The controlled protein intake in the diet aligns with diabetic guidelines and contributes to kidney health. Collaborating with healthcare professionals and dietitians is essential to create a comprehensive plan that addresses all conditions, promoting better overall health and potentially delaying the progression of kidney disease.
A Pre-Dialysis Diet Can Significantly Impact Your CKD Progression
Understanding the importance of a renal pre-dialysis diet is essential for individuals facing declining kidney function. This special diet plan plays a critical role in managing complications, optimizing overall health, and preserving kidney function.
By controlling nutrients such as sodium, potassium, phosphorus, and protein, patients can prevent their buildup and subsequent harm to the body. Regular monitoring of indicators like Blood Urea Nitrogen offers insights into kidney health and guides interventions.
Protein intake's impact on BUN levels underscores the need for careful management in pre-dialysis patients. Adapting to dietary needs during the pre-dialysis stage requires patience and a balanced approach, aided by stress management and exercise.
Fluid intake management is crucial, avoiding both excess and inadequacy. Limiting salt intake and incorporating whole grains contribute to kidney health. Calculating protein intake, in consultation with professionals, is vital to strike a balance between nutrition and kidney strain.
Lastly, planning ahead and adjusting the diet according to disease progression empower pre-dialysis patients to manage complications and enhance their well-being.








Mathea, as a CKD stage 4 patient, I would like to thank you very much
for the most informative suggestions on Renal diet.
I have purchased your Menu plan book , enjoying most recipes.
Each time I read your articles, gives me a little more hope. My hope of not
to have Dialysis.
Thanks again.
Joyce.