How Does Kidney Failure Affect the Body
You've often heard about kidney failure, but do you know how it impacts your body? It's not just about dialysis. When your kidneys can't filter waste or prevent fluid buildup (fluids to hydrate with kidney disorder), every part of you feels the strain.
From blood pressure issues to skeletal problems and even disruption of sleep patterns - kidney failure affects it all.
Let's dive deeper into understanding these effects; because knowing more could make a difference in someone's life.
Jump to:
- Key Takeaways
- The Role of Kidneys in Waste Removal and Dietary Impact
- The Function of Kidneys in Hormone Production
- Importance of Fluid Regulation by Kidneys
- Impact of Kidney Failure on the Blood and Cardiovascular Systems
- Kidney Failure and Its Effects on the Integumentary System
- Consequences of Kidney Failure on the Skeletal System
- Kidney Failure and Its Disruption of the Circadian System
- Other Noteworthy Effects of Kidney Failure
- Frequently Asked Questions
- Kidney Health Affects Overall Health
Key Takeaways
- Kidneys are vital for waste filtration, electrolyte balance, and blood pressure regulation.
- Kidney failure compromises filtration, leading to complications and dialysis need.
- Adhering to dietary restrictions eases strain on weakened kidneys in kidney failure.
- Impaired renal hormones affect blood, bone, and electrolyte balance.
- ESRD patients (ESRD anemia) face cardiovascular risks, skin issues, and mental health challenges.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
The Role of Kidneys in Waste Removal and Dietary Impact
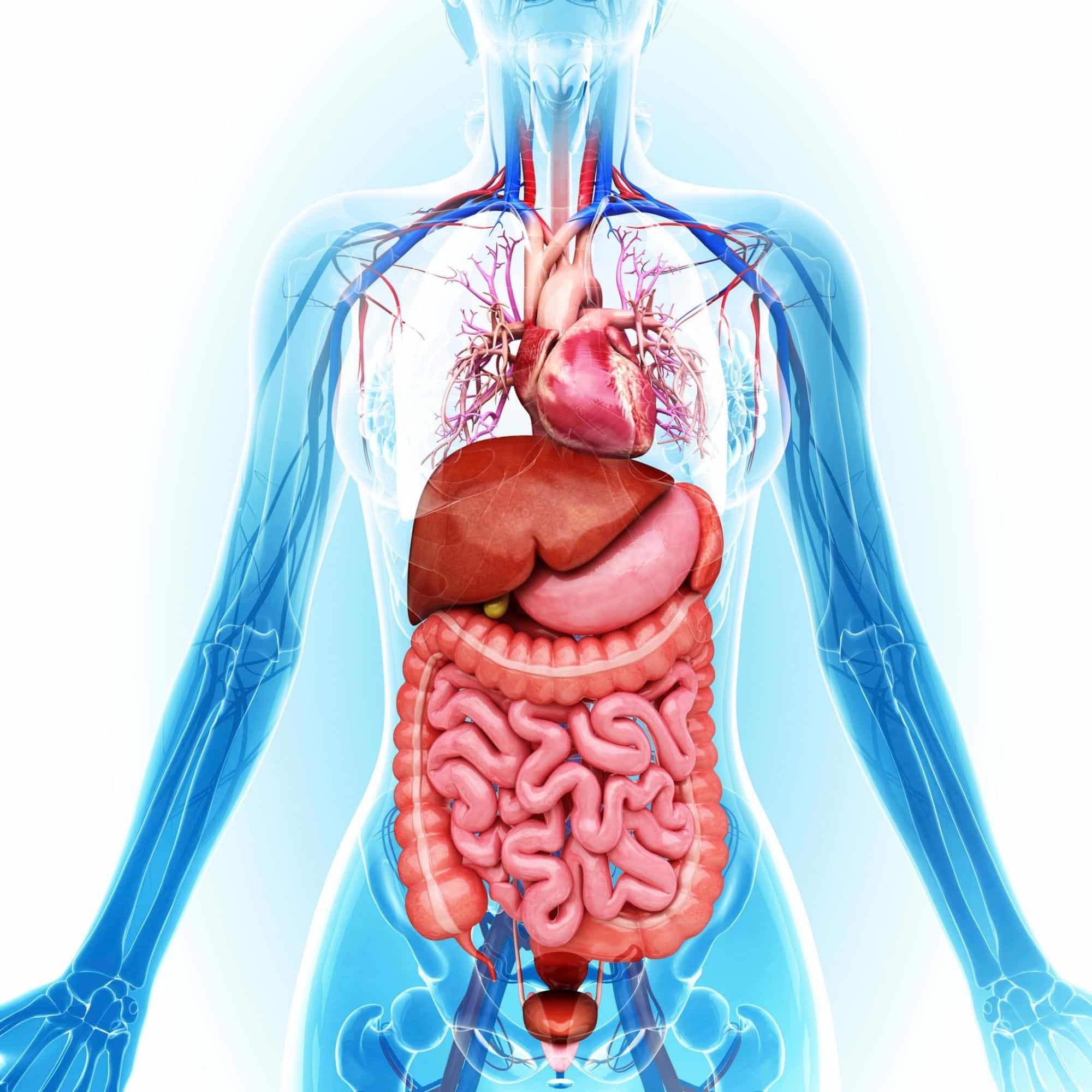
You might not fully appreciate the tremendous job your kidneys perform every day. They're not only responsible for filtering waste products, toxins, and excess substances from your bloodstream, but they also maintain a delicate balance of electrolytes in your body.
However, when there is loss of kidney function, it's crucial to adjust your diet as certain foods can further burden these vital organs or exacerbate health problems (questions about kidney transplant?)
Hence, the importance of understanding dietary restrictions (hyperparathyroidism diet restriction) for optimal kidney health.
Kidney's Role in Filtration
In the context of kidney failure, the role of the kidneys in waste filtration becomes crucially compromised. Healthy kidneys serve as the body's filtration system, removing waste products, extra fluids, and toxins from the bloodstream.
In kidney failure, the kidneys' ability to effectively filter and excrete these substances diminishes, leading to a buildup of waste in the blood. This accumulation of waste products contributes to various complications, such as elevated blood pressure, build up of fluid, electrolyte imbalances, and the deterioration of overall health.
Dialysis, a medical intervention, is often necessary to replicate the kidney's filtration function in individuals with kidney failure. Through hemodialysis or peritoneal dialysis, waste products and excess fluids are mechanically removed from the bloodstream, helping manage waste filtration in the absence of functional kidneys.
The profound impact of kidney failure on waste filtration underscores the critical importance of early detection, timely intervention, and ongoing medical management to alleviate the burden placed on the body by impaired kidney function.
Dietary Restrictions Importance
Kidney failure patients must adhere to dietary restrictions due to the kidneys' compromised ability to filter out wastes effectively. In this condition, the kidneys struggle to eliminate waste products, toxins, and excess fluids from the bloodstream.
Dietary restrictions help mitigate the strain on the body brought about by kidney damage by reducing the accumulation of waste and harmful substances. For instance, a low protein diet lessens the production of waste that the kidneys need to process.
Likewise, restricting sodium helps prevent fluid retention and hypertension. Potassium and phosphorus restrictions are crucial to avoid electrolyte imbalances that can arise from impaired kidney function.
By adhering to this special diet, kidney failure patients can optimize their overall health and minimize the risk of complications like fluid overload, electrolyte imbalances, and heart disease.
Collaborating with your health care team or registered dietitians ensures that dietary restrictions are tailored to individual needs, promoting a better quality of life and potentially slowing the progression of kidney disease.
The Function of Kidneys in Hormone Production
You might already know that your kidneys are crucial for filtering waste from your blood, but did you also know they're key players in hormone production?
That's right, these small yet mighty organs produce a variety of hormones that play vital roles in maintaining body functions.
In our discussion, we'll going to dive into the specifics of these hormones and explore how they impact everything from blood pressure (grilling blood pressure) regulation to target hemoglobin levels.
Hormones Produced by Kidneys
Kidney failure has a big impact on the hormones your body produces, especially those that come directly from the kidneys themselves. This can lead to a hormonal imbalance, which is where renal endocrinology comes into play.
As part of your role in serving others, it's crucial to understand three key kidney hormones:
- Erythropoietin: This hormone prompts erythropoiesis stimulation or red blood cell production. Kidney failure reduces its production, leading to anemia.
- Renin: It regulates blood pressure and electrolyte balance. When kidneys fail, this control falters.
- Calcitriol: The active form of Vitamin D necessary for calcium absorption. Impaired kidneys can't convert vitamin D into calcitriol, resulting in bone disorders.
Can kidney disease cause heart problems? In severe cases, hormone therapy may be required to manage symptoms and restore balance.
Impact on Body Functions
The impaired production of renal hormones, including erythropoietin, renin, and calcitriol, due to kidney dysfunction significantly impacts bodily functions.
Erythropoietin, responsible for red blood cell production, becomes deficient, leading to anemia and fatigue. Renin, regulating blood pressure, becomes imbalanced, contributing to hypertension and fluid retention.
Calcitriol, the active form of vitamin D, plays a role in calcium absorption and bone health; its reduced production can result in bone weakening and disturbances in calcium and phosphorus levels, affecting skeletal integrity and potentially leading to disorders like osteoporosis.
The interconnectedness of these hormones emphasizes how kidney dysfunction not only impairs waste filtration but also disrupts a range of essential physiological processes, necessitating careful medical management to address these multifaceted consequences.
Importance of Fluid Regulation by Kidneys
Your kidneys play a vital role in fluid regulation, significantly impacting your hydration status, blood volume, blood pressure, and ultimately your overall health. If they don't function properly, you could face serious health issues.
So let's dig into understanding how these two critical roles of the kidneys contribute to maintaining our body's delicate balance.
Preventing Water Retention
The kidney plays a crucial role in maintaining fluid balance by excreting excess water from the body and preventing water retention. It achieves this through intricate filtration and reabsorption mechanisms.
Blood enters the kidney, where it undergoes filtration, removing waste products and extra water, forming urine. The reabsorption process then takes place, allowing essential substances like nutrients and electrolytes to be reclaimed and returned to the bloodstream, while excess water is directed to the bladder for eventual elimination.
Hormones like antidiuretic hormone (ADH) regulate this process, adjusting water reabsorption based on hydration levels (kidney friendly drinks). In cases of kidney dysfunction, this balance is disrupted, leading to fluid retention, swelling, and potential complications.
Regulating Blood Pressure
The kidneys play a crucial role in regulating blood pressure through a complex system involving hormones, fluid balance, and blood vessel constriction. The renin-angiotensin-aldosterone system (RAAS) is a key component: when blood pressure drops, the kidneys release renin, which triggers a chain reaction leading to the production of angiotensin II.
Angiotensin II narrows blood vessels and stimulates the release of aldosterone, which promotes sodium retention, leading to water retention and increased blood volume. This mechanism raises blood pressure.
Additionally, the kidneys filter excess sodium, regulating its levels in the blood. Through these processes, the kidneys influence blood volume, sodium balance, and blood vessel constriction, all of which impact blood pressure regulation.
Dysfunction in these mechanisms can contribute to hypertension and other cardiovascular issues seen in renal patients.
Impact of Kidney Failure on the Blood and Cardiovascular Systems
Kidney failure has a profound impact on both your blood and cardiovascular systems.
One key point we'll tackle is how kidney failure can lead to anemia, a condition that arises when your body doesn't produce enough red blood cells.
Moreover, we'll explore the heightened cardiovascular risks associated with End-Stage Renal Disease (ESRD) also known as End Stage Kidney Disease, an advanced stage of kidney disease where dialysis or kidney transplant becomes essential for survival. Use these tips learn about how to avoid end stage renal disease.
Kidney Failure and Anemia
When kidney failure occurs, it often leads to anemia because the kidneys aren't producing enough of the hormone that helps create red blood cells. Anemia management becomes crucial in such situations.
Iron supplements are commonly used to boost erythropoiesis, or red blood cell production. Erythropoiesis Stimulating Agents (ESAs) may also be introduced, acting as a substitute for the hormone your kidneys should produce. In severe cases, you might need blood transfusions to maintain adequate red blood cell levels.
The impact of hemodialysis on anemia is significant too. While it's essential for removing waste from your bloodstream when your kidneys can't perform this task, hemodialysis may exacerbate anemia by causing extra loss of red blood cells during treatment.
Cardiovascular Risks in ESRD
End-stage renal disease (ESRD) patients face heightened cardiovascular risks due to the intricate connections between kidney function and cardiovascular health.
The impaired kidneys in ESRD contribute to fluid retention, elevated blood pressure, and electrolyte imbalances. As a result, the heart works harder, leading to left ventricular hypertrophy, heart failure, heart attack, arrhythmias, and other types of heart disease (ckd and heart disease).
The loss of renal hormones like erythropoietin affects red blood cell production, causing anemia, which strains the heart further. Additionally, ESRD disrupts the balance of calcium and phosphorus, affecting blood vessel health and increasing the risk of vascular calcifications.
Inflammatory processes, oxidative stress, and vascular inflammation further exacerbate cardiovascular risk. Consequently, a comprehensive approach to managing ESRD should encompass both renal and cardiovascular considerations to mitigate the substantial cardiovascular challenges this patient population faces.
Kidney Failure and Its Effects on the Integumentary System
If you're living with kidney failure, you might have experienced an annoying and persistent itch. This itching, medically known as uremic pruritus, is a common symptom indicating your body's struggle to filter waste products due to reduced kidney function.
We'll delve into the causes behind this discomfort and arm you with knowledge on how to manage and treat these skin symptoms effectively.
Itching and Kidney Failure
Patients with Stage 5 kidney disease (stages of chronic kidney disease) commonly experience skin issues, including uremic pruritus and xerosis cutis, due to the intricate interplay between kidney function and skin health.
Uremic pruritus, characterized by intense itching, arises from accumulated toxins that the kidneys fail to filter properly. These toxins irritate nerve endings in the skin, triggering itching. Xerosis cutis, or dry skin, is prevalent due to decreased oil and sweat gland function, coupled with dehydration common in ESRD.
Scratching caused by uremic pruritus can further exacerbate dry skin. Both conditions impact patients' quality of life, causing discomfort and potential sleep disturbances.
Proper hydration, maintaining skin moisture, and addressing underlying causes like effective dialysis and managing kidney function can help alleviate these skin issues.
Collaborative care between nephrologists (kidney doctor) and dermatologists (skin doctor) is crucial for managing ESRD-related skin complications effectively.
Treating Skin Symptoms
Treatment options for xerosis cutis and uremic pruritus in people with end-stage kidney failure involve a multifaceted approach.
For xerosis cutis, regular use of moisturizers helps alleviate dryness and itching. Avoiding hot water during bathing and using mild, non-drying soaps is recommended.
Uremic pruritus can be managed through improved dialysis, reducing phosphorus levels, and addressing underlying causes of itching.
Topical treatments like emollients and creams with menthol or pramoxine can provide relief. Antihistamines and certain medications like gabapentin can also help manage itching.
Collaborating with nephrologists, dermatologists, and other healthcare professionals ensures a tailored treatment plan to alleviate the discomfort and enhance the quality of life for people with kidney disease dealing with these skin issues.
Consequences of Kidney Failure on the Skeletal System
One major issue renal patients may encounter is bone mineral imbalance, a side effect that can lead to serious complications if not properly managed.
We'll explore what this means for you: why it occurs, how it impacts your skeletal system, and strategies to maintain optimal bone health despite these challenges.
Bone Mineral Imbalance
Bone mineral disorders are common in chronic kidney disease patients due to intricate disruptions in mineral metabolism. In normal kidney function, the kidneys regulate calcium and phosphorus levels, maintaining bone health.
In ESRD, the kidneys' diminished ability to excrete phosphorus leads to its accumulation in the blood, triggering a decrease in calcium levels. The body compensates by producing parathyroid hormone (PTH), which pulls calcium from bones to maintain blood levels.
Elevated PTH levels cause bone resorption, weakening bones and leading to medical conditions like renal osteodystrophy. The imbalances disrupt the delicate equilibrium between bone formation and resorption, resulting in bone demineralization, fragility, and an increased risk of fractures in a person with stage 5 CKD.
The intricate interplay of mineral metabolism, PTH, and bone health underscores the complexity of bone mineral disorders in this population.
Maintaining Bone Health
ESRD patients can take preventive measures to maintain good bone health and reduce the risk of bone mineral disorders.
Adequate management of calcium and phosphorus levels is crucial, often through dietary adjustments and medications to control hyperphosphatemia. Monitoring and managing parathyroid hormone (PTH) levels helps prevent excessive bone resorption.
Regular exercise, including weight-bearing activities, supports bone density and strength. Managing vitamin D deficiency aids in calcium absorption and bone health. Adherence to prescribed dialysis and proper management of ESRD overall play vital roles.
Collaborating with healthcare professionals for tailored guidance on nutrition, medications, and lifestyle adjustments such as regular physical activity is essential to optimize bone health and prevent bone mineral disorders, ultimately enhancing the quality of life for people with kidney failure.
Kidney Failure and Its Disruption of the Circadian System
You're likely aware that kidney failure can disrupt more than just the body's filtering system—it can also wreak havoc on your sleep patterns.
The interplay between chronic kidney disease and sleep disturbances is a complex issue, resulting in a variety of problems including insomnia, restless leg syndrome, and sleep apnea.
Understanding these issues not only helps to improve the quality of life for people with kidney disease but also guides healthcare professionals in developing effective treatment strategies for such sleep-related complications. Some people even
Sleep Disturbances in Patients
It's common for patients with kidney failure to experience sleep disturbances due to a variety of factors. You might notice insomnia prevalence, restless legs, or dream disturbances making it hard for your patient to maintain good sleep hygiene.
Consider these reasons:
- Dysregulation of Circadian Rhythm: Kidney failure disrupts the body's internal clock.
- Restless Legs Syndrome (RLS): This uncomfortable sensation results in an irresistible urge to move the legs during rest.
- Dream Disturbances: Conditions like nightmare disorder or REM sleep behavior disorder may develop.
- Medication Side Effects: Sleep medications could inadvertently cause disruptions.
Understanding these factors allows you to better serve those in need and provide them with appropriate interventions aimed at improving their quality of life.
Treatment for Sleep Issues
There're several treatments available for sleep issues, ranging from lifestyle changes to medication adjustments. You might consider improving your sleep hygiene habits or exploring cognitive therapy options. For more severe cases, melatonin supplementation or specific sleep medications could be beneficial.
If you're dealing with restless legs syndrome, there are various strategies that can provide relief. Here's a helpful table outlining these treatment methods:
| Treatment Method | Description |
| Sleep Hygiene | Establishing a regular bedtime routine and creating an environment conducive to good quality sleep |
| Cognitive Therapy | Using psychological techniques to change the patterns of thinking or behavior that contribute to sleep problems |
| Melatonin Supplementation | Taking synthetic hormones to adjust the body's internal clock and improve sleep quality |
| Sleep Medication | Using prescribed drugs to treat insomnia or other serious sleep disorders |
Remember, all treatments given for each kidney patient are individualized. Hence, if you suffer from any sleep disturbance associated with your chronic kidney disease, it is crucial to seek consult with your healthcare provider.
Other Noteworthy Effects of Kidney Failure
Aside from the various systemic effects of kidney failure that we discussed, this condition has further notable effects in terms of mental health and digestive health.
How does kidney failure affect the body? With a detailed understanding of these aspects, you'll gain a comprehensive view of the far-reaching consequences that renal failure could have on your overall health.
Mental Health Impact
Kidney failure's impact on mental health can't be underestimated, often leading to depression and anxiety. You'll find that the emotional stress faced by patients is monumental. Let's look at three main effects: Depression Prevalence, Anxiety Disorders, and Cognitive Decline.
| Impact | Symptoms | Management |
| Depression | Persistent sadness, loss of interest in activities, difficulty concentrating. | Psychotherapy, medication. |
| Anxiety Disorders | Rapid heart rate, rapid breathing, restlessness. | Therapy sessions with a psychologist or psychiatrist. |
| Cognitive Decline | Mental confusion, memory problems. | Brain exercises like puzzles or games. |
In addition to these issues is the problem of social isolation due to physical limitations and dependency on others for survival needs.
Remember, it's crucial to address these struggles immediately as they significantly affect a patient's quality of life and overall health outcomes. Check out this 7 day meal plan for kidney disease.
Digestive System Effects
ESRD patients often experience digestive issues, with uremic gastropathy being a significant concern. Uremic gastropathy, resulting from the accumulation of urea and other waste products, affects the stomach's function.
It leads to delayed gastric emptying, reduced acid production, and impaired motility, causing symptoms like nausea, vomiting, and early satiety. Additionally, constipation (constipation and kidney disease) is common due to factors such as fluid restrictions, dietary changes, and medications.
These digestive issues contribute to poor appetite, malnutrition, and a reduced quality of life for ESRD patients. Adequate fluid management, dietary adjustments, and medications to control symptoms play pivotal roles in alleviating these concerns.
Collaborative care involving nephrologists, dietitians, and other specialists ensures a comprehensive approach to managing digestive problems and improving overall well-being in ESRD patients (ESRD Prognosis).
Frequently Asked Questions
Primary symptoms of kidney failure include fatigue, weakness, swelling in the legs and ankles (edema), decreased urine output, changes in urination patterns, persistent nausea, loss of appetite, difficulty concentrating, itchy skin, and shortness of breath.
As kidney function declines, waste products and fluids build up in the body, causing these symptoms of kidney disease.
High blood pressure, anemia, and electrolyte imbalances can also accompany kidney failure. Early detection and medical evaluation are crucial if these symptoms arise, as prompt intervention can help manage the condition and prevent further complications.
Kidney failure can significantly impact mental health and cognitive function. Accumulation of waste products in the blood, electrolyte imbalances, and hormonal disruptions can lead to symptoms like difficulty concentrating, memory problems, confusion, and even cognitive impairment.
Patients may also experience mood changes, including depression and anxiety, due to the physical and emotional challenges of managing a chronic condition.
Dialysis and medication side effects can further affect mental well-being. Addressing these aspects is vital for holistic patient care, as improved kidney function and comprehensive support contribute to better cognitive function and enhanced mental health outcomes in individuals dealing with kidney failure.
Yes, kidney failure can affect sexual health and reproductive capabilities. Hormonal imbalances, including decreased testosterone and disrupted menstrual periods, can lead to reduced libido, erectile dysfunction, and infertility.
Accumulation of toxins and fluid imbalances can contribute to fatigue, impacting sexual desire.
Additionally, psychological factors like anxiety, depression, and body image concerns stemming from kidney disease can affect sexual well-being. Management strategies, including proper treatment, medication adjustments, and open communication with healthcare providers, can help mitigate these challenges.
Collaborative care addressing physical and emotional aspects is crucial in maintaining sexual health and reproductive capabilities for individuals with kidney failure.
Have questions about kidney transplant? Kidney failure treatment include dialysis and kidney transplantation. Dialysis treatment involves using machines to filter waste and excess fluid from the blood, helping to manage kidney functions.
There are two main types: hemodialysis, where blood is filtered through an external machine, and peritoneal dialysis, where the abdominal lining filters the blood.
Kidney transplantation involves replacing the failed kidney with a healthy one from a living or deceased donor. Each option has its benefits and considerations, and the choice depends on factors like overall health, lifestyle, and medical recommendations.
Collaborative care with healthcare professionals including a kidney specialist is essential in determining the best treatment approach for each individual.
Yes, lifestyle changes and dietary modifications can help prevent or slow down the progression of kidney failure. Managing blood pressure and blood sugar levels, weight loss (if needed), and staying physically active are crucial.
Reducing salt and processed foods intake, limiting phosphorus and potassium-rich foods, and monitoring protein intake can ease the strain on the kidneys.
Staying hydrated and avoiding excessive alcohol consumption also play a role. Collaborating with healthcare professionals, particularly dietitians and nephrologists, is essential in tailoring lifestyle and dietary adjustments to individual needs, thus supporting kidney health and potentially delaying the progression of kidney failure.
Kidney Health Affects Overall Health
You see, your kidneys are crucial for keeping your body in balance - from waste removal to hormone production. Kidney failure disrupts this balance, affecting everything from your blood to your skin and bones. It even throws off your circadian rhythm! Make sure you take the right steps to improving kidney health.
So remember, looking after your kidney health is essential for overall wellness. Don't underestimate the far-reaching effects of kidney failure (dialysis effects) on the body.