Can Kidney Disease Cause Heart Problems
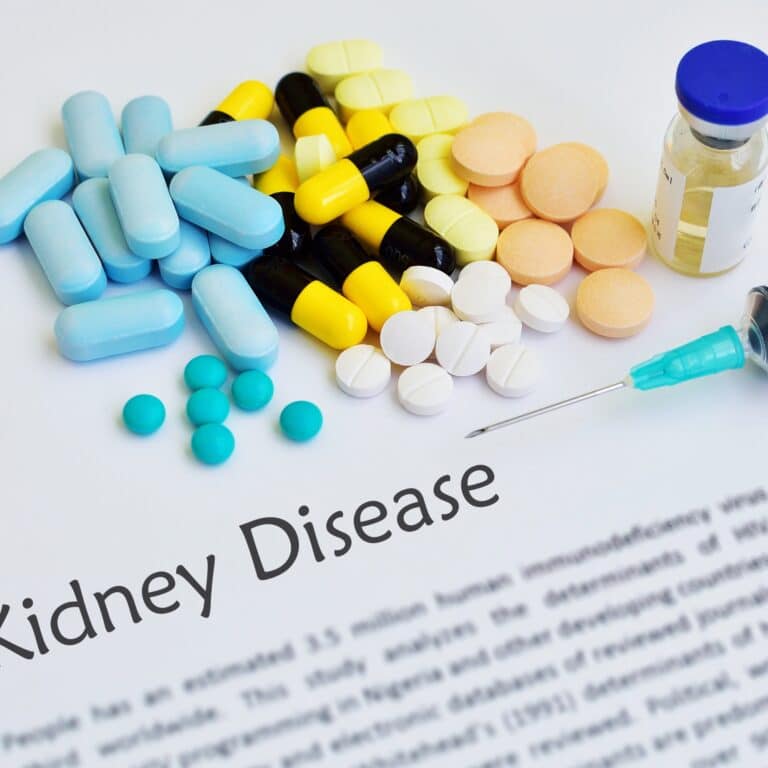
If you're caring for someone with Chronic Kidney Disease (CKD), it's important to understand the link between CKD and heart health. Due to their higher risk of heart disease, this is the top cause of death in patients with CKD.
This connection stems from complications like high blood pressure, diabetes, anemia, fluid retention, and atherosclerosis that are common in CKD patients. These issues can lead to serious cardiac problems such as heart attack or congestive heart failure.

Therefore, managing these conditions through lifestyle changes such as a healthy diet, regular exercise and routine check-ups becomes imperative. It's crucial to monitor blood pressure levels and blood sugar if diabetes is present.
In this article, we'll delve into how kidney disease can cause heart problems and provide tips on prevention strategies. Remember that understanding health risks associated with kidney disease is a key step towards providing effective care.
Jump to:
- Key Takeaways
- Understanding the Connection Between Kidney Disease and Heart Health
- How High Blood Pressure in CKD Increases Heart Disease Risk
- The Role of Diabetes in Kidney Disease and Heart Complications
- Anemia: A Common Complication of CKD Leading to Heart Problems
- Fluid Retention in CKD and Its Impact on Heart Health
- Electrolyte Imbalance in CKD: A Hidden Risk for Heart Disease
- Atherosclerosis: A Heart-Related Complication of CKD
- Lifestyle Changes to Reduce Heart Disease Risk in CKD
- The Importance of Regular Check-ups for CKD and Heart Health
- Frequently Asked Questions
- If You Have CKD, It’s Important To Take Care of Your Heart
Key Takeaways
- Chronic Kidney Disease (CKD) is linked to a higher risk of heart disease, the top cause of death in patients with renal disease.
- Complications common in CKD patients include high blood pressure, diabetes, anemia, fluid retention, and atherosclerosis, all of which can contribute to heart problems.
- Lifestyle changes, such as a healthy diet, regular exercise, and routine check-ups, are crucial for managing these conditions and preventing cardiovascular complications.
- Monitoring and managing blood pressure, blood sugar levels, anemia, fluid retention, and electrolyte imbalances are essential for preventing heart-related issues in CKD patients.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding the Connection Between Kidney Disease and Heart Health
The connection between kidney disease and heart health is intricate and bidirectional. Chronic kidney disease (CKD) and cardiovascular disease share several risk factors and often coexist, leading to a synergistic negative impact on overall health.
Firstly, CKD can contribute to heart problems through various mechanisms. As the kidneys function declines, they become less effective in removing waste and excess fluids from the body. This can lead to fluid retention and an increase in blood pressure, putting strain on the heart. Additionally, CKD can cause an imbalance of electrolytes, such as potassium and phosphorus, which can disrupt heart rhythm and function.
Secondly, heart disease can also contribute to kidney damage. Cardiovascular issues, like atherosclerosis and hypertension, can reduce blood flow to the kidneys, impairing their function over time. Furthermore, some medications used to manage heart conditions can have adverse effects on kidney function.
Both CKD and heart disease share common risk factors, such as diabetes, high blood pressure, obesity, and smoking. Managing these risk factors is vital to prevent or slow the progression of both conditions.
To improve heart health in patients with CKD, health care providers focus on controlling blood pressure, managing blood sugar levels, and promoting a heart-healthy diet. Similarly, in individuals with heart disease, careful management of medications and lifestyle changes can help preserve kidney function.
Regular monitoring and coordination between nephrologists and cardiologists are crucial to ensuring comprehensive care for patients with both kidney disease and heart conditions. An integrated approach to managing these interconnected conditions can significantly improve overall outcomes and enhance the quality of life for affected individuals.
How High Blood Pressure in CKD Increases Heart Disease Risk
In individuals grappling with CKD, elevated blood pressure is a frequent concern, significantly heightening the likelihood of heart-related complications. This health predicament forces your heart to work harder than usual to circulate blood throughout your body. Over time, this overexertion can weaken the heart muscles and induce a heart attack or stroke.
The impact of medication can't be overstated in regulating blood pressure and mitigating potential cardiovascular issues. Antihypertensive drugs are often prescribed to control high blood pressure and protect your heart from damage. However, their effectiveness can be influenced by genetic factors unique to each individual.
Chronic inflammation, commonly seen in CKD patients, plays a critical role in elevating blood pressure levels and indirectly contributes to the progression of heart disease. Lifestyle modifications such as maintaining a balanced diet low in sodium, regular exercise, and stress management techniques can aid in keeping inflammation and hypertension under control.
The impact of stress on cardiovascular health is profound too; it exacerbates high blood pressure conditions making it even more challenging for CKD patients. It's essential that you manage stress effectively through mindfulness practices or other relaxation techniques.
Remember that managing kidney disease isn't just about treating the kidneys - it involves comprehensive care for all interconnected bodily systems.
The Role of Diabetes in Kidney Disease and Heart Complications
Diabetes plays a multifaceted and detrimental role in both chronic kidney disease (CKD) and cardiovascular disease (CVD). As a leading cause of CKD, diabetes poses a significant risk to kidney health.
Prolonged high blood sugar levels damage the delicate blood vessels in the kidneys, impairing their filtration function. Over time, this can lead to kidney damage and the progressive decline of kidney function.
Furthermore, diabetes is closely linked to an increased risk of cardiovascular disease. High blood sugar levels can damage the inner lining of blood vessels, promoting the formation of atherosclerotic plaques.
These plaques can narrow and obstruct blood vessels, leading to conditions like coronary artery disease, heart attacks, and strokes. Diabetes also contributes to other risk factors for CVD, such as high blood pressure and abnormal lipid profiles.
The combination of diabetes, CKD, and cardiovascular disease forms a dangerous triad known as "diabetic kidney disease." The coexistence of these conditions amplifies the risk of adverse health outcomes and further complicates treatment and management.
Diabetes management is crucial in mitigating the impact of diabetes on both CKD and CVD. Early detection, regular monitoring, and lifestyle modifications are essential components of minimizing the progression of kidney and heart complications.
Close collaboration between healthcare providers is necessary to ensure comprehensive care for individuals with diabetes and its associated effects on kidney and cardiovascular health. By addressing the connection between diabetes, CKD, and CVD, healthcare professionals can work towards preventing complications and improving overall health outcomes for affected individuals.
Anemia: A Common Complication of CKD Leading to Heart Problems
Anemia and chronic kidney disease (CKD) are closely interlinked, and their connection can have significant implications for cardiovascular health. Anemia is a common complication of CKD, especially in its later stages when the kidneys' ability to produce erythropoietin, a hormone that stimulates red blood cell production, is compromised.
In CKD, as the kidneys lose their function, they produce less erythropoietin, leading to reduced red blood cell production. This results in anemia, where the blood's oxygen-carrying capacity is diminished, leading to fatigue, weakness, and shortness of breath. Anemia can worsen other CKD-related symptoms and reduce the patient's quality of life.
Moreover, anemia can have adverse effects on cardiovascular health. When the body's tissues and organs receive insufficient oxygen due to reduced red blood cells, the heart compensates by pumping more blood to meet the oxygen demand. This increased workload on the heart can lead to cardiac strain and the development of left ventricular hypertrophy, a condition where the heart's left ventricle thickens and enlarges.
Furthermore, anemia is associated with an increased risk of cardiovascular events, such as heart attacks and heart failure. The combination of CKD, anemia, and cardiovascular disease can create a harmful cycle, where each condition exacerbates the other, leading to a higher risk of complications and mortality.
Effective management of anemia in CKD patients is crucial to improve overall health and prevent cardiovascular complications. Treatment may involve erythropoiesis-stimulating agents or iron supplementation to boost red blood cell production. Regular monitoring of anemia and cardiovascular health is essential to provide timely interventions and optimize patient outcomes.
Fluid Retention in CKD and Its Impact on Heart Health
Fluid retention, also known as edema, is a common and concerning complication of chronic kidney disease. As the kidneys lose their ability to filter waste and excess fluids from the body, fluid can accumulate, leading to swelling in various parts of the body, including the ankles, legs, and hands.
Fluid retention in CKD can have a significant impact on the heart and cardiovascular system. The extra fluid levels in the body increases blood volume, putting added strain on the heart. This can lead to an increase in blood pressure, a condition known as hypertension, which is a common complication of CKD.
Hypertension can further damage the already compromised kidneys, leading to a vicious cycle of worsening kidney function and fluid retention.
Moreover, fluid overload can lead to congestive heart failure, a condition where the heart's ability to pump blood efficiently is impaired. The increased fluid volume puts pressure on the heart, causing it to weaken over time. As the heart becomes less effective in pumping blood, fluid can back up into the lungs, leading to shortness of breath and other respiratory symptoms.
In addition to its impact on the heart, fluid retention in CKD can also lead to electrolyte imbalances, such as high potassium levels (hyperkalemia), which can be life-threatening.
Managing fluid retention is crucial in CKD to alleviate strain on the heart and improve overall cardiovascular health. Dietary modifications, such as limiting salt intake, and the appropriate use of diuretics to promote fluid removal are common strategies to address fluid retention in CKD patients. Regular monitoring of fluid status and cardiovascular health is essential to prevent complications and optimize patient outcomes.
Electrolyte Imbalance in CKD: A Hidden Risk for Heart Disease
Electrolyte imbalances, such as hyperkalemia (high potassium levels), can pose significant cardiac complications for patients with chronic kidney disease (CKD).
The kidneys play a crucial role in maintaining the balance of electrolytes, including potassium, in the body. However, as kidney function declines in CKD, the kidneys may become less effective in excreting potassium, leading to its accumulation in the bloodstream.
Hyperkalemia can have adverse effects on the heart and can lead to life-threatening cardiac arrhythmias. Excess potassium interferes with the normal electrical activity of the heart, causing irregular heartbeats or even sudden cardiac arrest. This risk is particularly heightened in patients with pre-existing heart conditions.
Furthermore, in CKD patients, the combination of electrolyte imbalances and fluid retention can further exacerbate the cardiac strain. The increased blood volume resulting from fluid overload can worsen hypertension, which is already prevalent in CKD. Elevated blood pressure places additional stress on the heart, increasing the risk of heart failure and other cardiovascular complications.
To address hyperkalemia and prevent cardiac complications, CKD patients may be prescribed medications called potassium binders, which help remove excess potassium from the body. Additionally, dietary modifications, such as limiting potassium intake, may be recommended.
Regular monitoring of potassium levels and close communication with healthcare providers are essential to manage electrolyte imbalances effectively and reduce the risk of cardiac complications in patients with CKD.
Atherosclerosis: A Heart-Related Complication of CKD
Chronic kidney disease and atherosclerosis are closely linked, with one condition often exacerbating the other. Atherosclerosis is a progressive condition characterized by the buildup of plaque within the arterial walls, leading to narrowing and hardening of the blood vessels. In CKD, the kidneys' impaired function contributes to an increased risk of atherosclerosis and its related complications.
One of the key factors linking CKD and atherosclerosis is chronic inflammation. In CKD, there is a state of systemic inflammation due to the kidneys' inability to efficiently filter and eliminate waste products from the bloodstream. This chronic inflammation can damage the blood vessel walls and promote the development of atherosclerotic plaques.
Moreover, CKD is associated with various risk factors that contribute to atherosclerosis, such as hypertension, dyslipidemia (abnormal or elevated levels of cholesterol), coronary heart disease, and insulin resistance. Additionally, CKD patients often have increased levels of oxidative stress, which can further promote atherosclerosis.
As atherosclerosis progresses, it can have serious consequences for CKD patients. The narrowed and hardened blood vessels reduce blood supply to vital organs, including the kidneys, exacerbating kidney damage and accelerating CKD progression. Atherosclerosis also increases the risk of adverse cardiovascular outcomes, such as ischemic heart disease, heart attacks, and strokes, which are the leading causes of mortality in CKD patients.
To manage the link between CKD and atherosclerosis, it is essential to control the underlying risk factors and focus on lifestyle modifications. Controlling blood pressure, managing cholesterol levels, adopting a heart-healthy diet, engaging in regular physical activity, and avoiding smoking are critical steps in reducing the impact of atherosclerosis on CKD patients.
Regular monitoring and close collaboration with health care providers can help mitigate the risk of complications and improve the overall health outcomes for individuals with CKD and atherosclerosis.
Lifestyle Changes to Reduce Heart Disease Risk in CKD
Chronic Kidney Disease (CKD) patients are at an increased risk of heart disease, making lifestyle changes essential to reduce this risk. Adopting a heart-healthy lifestyle can positively impact both kidney and cardiovascular health. Key lifestyle modifications include:
- Diet: Follow a balanced diet low in sodium, saturated and trans fats, and cholesterol. Opt for fresh fruits, vegetables, whole grains, lean proteins, and healthy fats like those found in nuts and avocados. Limit processed foods and sugary beverages.
- Physical Activity: Engage in regular physical activity, such as walking, swimming, or cycling, to maintain a healthy weight, improve cardiovascular function, and lower blood pressure.
- Smoking Cessation: Quit smoking and avoid exposure to secondhand smoke. Smoking damages blood vessels and exacerbates kidney and heart conditions.
- Manage Blood Pressure: Monitor blood pressure regularly and take prescribed medications as directed by a healthcare provider to keep it under control.
- Control Blood Sugar: If diabetic, manage blood glucose levels through medication, diet, and exercise, as uncontrolled diabetes can exacerbate kidney and heart problems.
- Weight Management: Maintain a healthy weight to reduce the strain on the kidneys and heart.
- Stress Management: Practice stress-reduction techniques like meditation, yoga, or deep breathing to lower stress levels, which can impact heart health.
- Limit Alcohol Intake: If you consume alcohol, do so in moderation as excessive alcohol can strain the kidneys and adversely affect heart health.
Remember, always consult a health care provider before making significant lifestyle changes to ensure they are appropriate for your specific CKD condition and medical history.
The Importance of Regular Check-ups for CKD and Heart Health
Regular check-ups should be a non-negotiable part of your self-care routine, especially when you're grappling with conditions like CKD. These visits are crucial for monitoring your cardiovascular health and identifying any potential risk factors that might lead to heart problems.
Your healthcare provider will focus on these key prevention strategies:
- Monitoring blood pressure and sugar levels: This helps in managing hypertension and diabetes, two major contributors to heart disease.
- Regular blood tests: They can detect early signs of anemia or electrolyte imbalance that can impact your heart's function.
- Checking for signs of fluid retention or atherosclerosis: Early detection is vital in preventing congestive heart failure or coronary artery disease.
By adhering to regular check-ups, you're not just taking care of your kidneys but also actively investing in your heart's health. It allows for timely intervention if there are concerning changes in your health status.
Remember, the goal is not just about surviving with CKD; it's about thriving despite it. Good cardiovascular health is integral to this aim. So make sure those appointments are marked on your calendar and attended without fail because every step taken towards prevention today ensures a healthier tomorrow.
Frequently Asked Questions
Early signs of heart disease in CKD patients may include high blood pressure, elevated cholesterol levels, and abnormal electrocardiogram (ECG) results. Additionally, symptoms of heart disease may include chest pain (angina), shortness of breath, fatigue, and swelling in the legs and ankles.
As CKD progresses, these signs can worsen, leading to chronic heart failure and other cardiovascular complications. Regular monitoring of blood pressure, cholesterol levels, and renal function is crucial in detecting and managing heart disease in CKD patients. Prompt medical attention and lifestyle modifications can help reduce the risk of cardiovascular events in this vulnerable population.
CKD patients should have their heart health checked regularly to monitor and manage any potential cardiovascular complications. The frequency of these checks may vary based on the individual's specific condition and risk factors. Generally, it is recommended to have annual check-ups that include monitoring blood pressure, cholesterol levels, and kidney function which is measured by the glomerular filtration rate.
Additionally, regular visits to a cardiologist may be advised, especially if there are any concerning symptoms or risk factors. Collaboration between nephrologists and cardiologists is essential to provide comprehensive care and reduce the risk of heart disease in CKD patients.
In CKD patients, certain medications can help prevent heart disease and its complications. Angiotensin-converting enzyme inhibitors (ACE inhibitors) and angiotensin receptor blockers (ARBs) are commonly prescribed as they not only lower blood pressure but also have protective effects on the kidneys and heart. Additionally, statins may be prescribed to control cholesterol levels and reduce the risk of atherosclerosis.
Aspirin might be recommended for some CKD patients with a high risk of cardiovascular events. Others may need beta blockers to control heart rate. However, medication choices should be personalized to the individual's medical history, kidney function, and overall health, and only prescribed by a qualified healthcare professional.
Yes, there is a genetic link between kidney disease and heart disease. Certain genetic factors can predispose individuals to both conditions. For instance, certain genetic mutations can lead to abnormalities in proteins that affect blood vessel function, leading to both kidney and heart problems. Moreover, genetic conditions like polycystic kidney disease (PKD) can affect both the kidneys and the heart.
Additionally, shared risk factors such as high blood pressure, diabetes, and obesity can contribute to the development of both kidney and heart diseases. Early detection, monitoring, and lifestyle modifications are essential for individuals with a genetic predisposition to these conditions.
Lifestyle changes play a crucial role in reducing the risk of heart disease in CKD patients, but in many cases, medication is also necessary. Lifestyle modifications, including a heart-healthy diet, regular exercise, smoking cessation, and stress management, can positively impact cardiovascular health and kidney function.
However, some risk factors, like high blood pressure and elevated cholesterol levels, may require medication to achieve optimal control. A combination of lifestyle changes and appropriate medications prescribed by healthcare professionals is often the most effective approach to reduce the risk of heart disease in CKD patients and improve overall outcomes.
If You Have CKD, It’s Important To Take Care of Your Heart
Chronic Kidney Disease patients have a higher risk of heart disease, making it vital to understand the connection between CKD and heart health. Complications like high blood pressure, diabetes, anemia, fluid retention, and atherosclerosis contribute to serious cardiac problems.
Implementing lifestyle changes such as a healthy diet, regular exercise, and routine check-ups is imperative to manage these conditions and prevent cardiovascular complications. Monitoring and managing blood pressure, blood sugar levels, anemia, fluid retention, and electrolyte imbalances are essential for preventing heart-related issues in CKD patients.
An integrated approach with regular check-ups and collaboration between health care providers is crucial for comprehensive care and improving overall outcomes.