Renal Dietitians
Patients living with chronic health conditions such as renal disease should count themselves lucky that they live in such an era of advanced medicine. Just in recent years, advancements have been made that increase the comfort and longevity of people living with these chronic conditions.
Not only that, but people and doctors alike have learned the importance of a healthy and appropriate diet to not only treat renal disease, but effectively slow or halt the kidney disease progression (questions about end stage renal disease).
Renal dietitians are highly trained professional experts in diet who specialize in helping people with chronic kidney disease (CKD) manage their dietary needs. With their help, kidney patients can make lifestyle changes and develop personalized meal plans that will improve their health and quality of life.

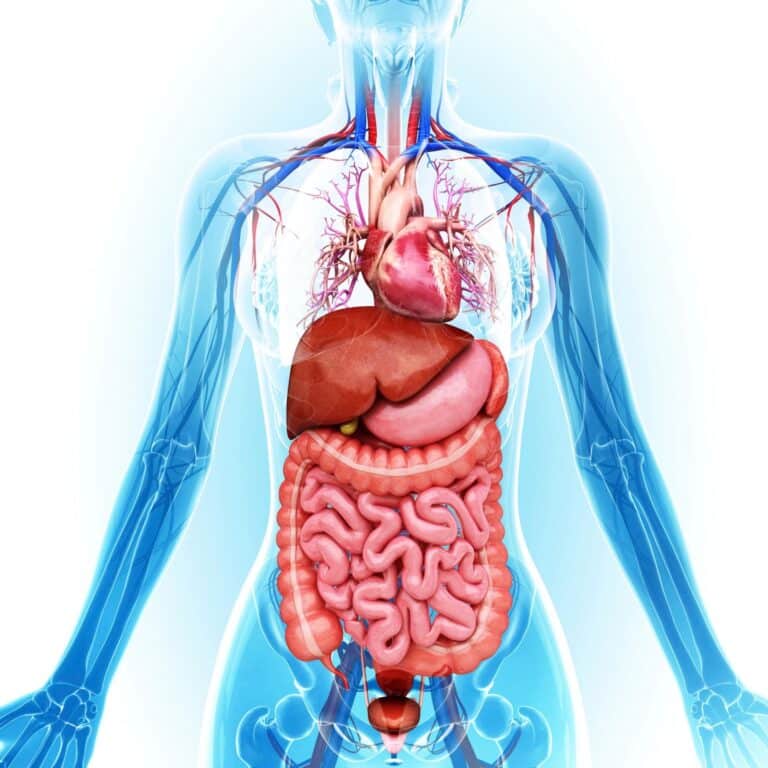
A renal dietitian (or renal nutritionist, or renal dietitian nutritionist is a medical expert that specializes in the diet and nutrition of people with chronic kidney disease. Renal dietitians are highly specialized medical professionals who know all about how diet affects your whole body if you have renal disease, including how your diet will affect not only your kidneys, but your other organs like your heart as well.
The dietary needs of a chronic kidney disease patient are extremely important, as diet often affects the body just as much if not more than medications and regular checkups.
Jump to:
- Key Takeaways
- Understanding Chronic Kidney Disease (CKD)
- The Role of Renal Dietitians in CKD Management
- How Renal Dietitians Help in Personalized Diet Planning
- The Importance of Protein Management in CKD
- Balancing Sodium and Potassium Levels in CKD
- Phosphorus Control in CKD: A Dietitian's Guide
- The Impact of Fluid Intake on Kidney Health
- Dietary Adjustments for CKD Stages
- Lifestyle Changes Recommended by Renal Dietitians
- Additional Resources For Renal Dietitian Advice
- Frequently Asked Questions
- A Renal Dietitian’s Guidance Can Make A World Of Difference In Your CKD Management
Key Takeaways
- Renal dietitians specialize in creating personalized meal plans for CKD patients to improve their health and quality of life.
- People with kidney disease have unique dietary needs, and renal dietitians provide invaluable support in areas such as mineral supplementation, weight management, fluid monitoring, carbohydrate counting, and vitamin intake.
- Balancing sodium and potassium levels, controlling phosphorus intake, and monitoring fluid intake are crucial for kidney health in CKD patients, and renal dietitians can provide individualized advice on these dietary considerations.
- Making lifestyle changes and following a well-rounded plan of care, including effective dialysis treatments and regular monitoring of health status and medication needs, can help manage advanced CKD symptoms, and consulting a renal dietitian for tailored advice and guidance is important.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding Chronic Kidney Disease (CKD)
Chronic kidney disease is a long-term condition characterized by the gradual loss of kidney function over time. It is a significant global health issue that affects millions of people worldwide. CKD can develop due to various underlying causes, such as high blood pressure, diabetes, glomerulonephritis, polycystic kidney disease, and overuse of certain medications.
The kidneys play a vital role in filtering waste products, excess fluids, and toxins from the blood, maintaining electrolyte balance, and regulating blood pressure. As CKD progresses, the kidneys become less efficient in performing these functions, leading to a buildup of waste and fluid in the body.
Common symptoms of CKD include fatigue, swollen ankles, increased urination at night, blood in urine, and high blood pressure.
CKD is classified into five stages based on the estimated glomerular filtration rate (eGFR), which measures the kidney's ability to filter blood.
In the early stages (1 and 2), there may be mild kidney damage, often without noticeable symptoms. However, as the disease progresses to stages 3, 4, and 5, the kidney function continues to decline, and symptoms become more prominent.
If left untreated or unmanaged, CKD can lead to end-stage renal disease (ESRD), where the kidneys lose almost all their function, requiring renal replacement therapy such as dialysis or kidney transplant.
However, with early detection and appropriate management, the progression of CKD can be slowed, and complications can be minimized.
The management of CKD involves a multidisciplinary approach, including lifestyle modifications, medication, and regular monitoring.
Blood pressure control, blood sugar management (for individuals with diabetes), dietary changes (such as reducing sodium and protein intake), and smoking cessation are essential components of CKD management.
Medications may be prescribed to control blood pressure, manage blood sugar levels, reduce cholesterol, and treat complications associated with CKD.
Regular monitoring through blood testing and urine tests is crucial to assess kidney function, identify any complications, and adjust the plan of care accordingly. Patient education and support are also integral to CKD management, empowering individuals to make informed decisions about their health and adhere to the recommended lifestyle changes.
In conclusion, chronic kidney disease is a progressive condition that affects the kidneys' ability to function properly. Early detection, proper management, and lifestyle modifications can slow the progression of the disease, improve quality of life, and reduce the risk of complications.
The Role of Renal Dietitians in CKD Management
A kidney disease diagnosis can be overwhelming, but having an experienced dietitian on your side can help you manage it and even thrive. Renal dietitians are skilled professionals who specialize in helping patients with chronic kidney disease (CKD). They understand how to adjust kidney diets so that CKD patients can maintain optimal nutrition while managing their symptoms.
It's important for those affected by CKD to understand the dietary guidelines set forth by renal dietitians in order to maintain good kidney health. Renal nutritionists are experts at meal planning and helping individuals make better food choices that will help manage CKD symptoms, such as fatigue, anemia, and fluid retention.
They provide individualized advice based on each person's unique needs to ensure that they receive an optimal nutrition plan for their condition. Renal dietitians work with patients and healthcare providers alike in order to create eating plans tailored specifically to the individual's lifestyle, medical history, and health goals.
They take into consideration all aspects of a person's life when creating meal plans, including their weight loss or gain goals, physical activity levels, personal preferences/tastes, cultural background/food traditions, financial resources available for food purchases, etc.
Healthy eating plans created by renal nutritionists should include nutrient-dense foods such as fruits & vegetables; lean proteins; whole grains; low-fat dairy products; healthy fats; and limited amounts of sodium & sugar. Additionally, they may suggest supplements specific to one's condition in order to meet their daily nutritional needs if necessary.
CKD patients have unique dietary needs because what works well for one person may not be beneficial for another. This is why it's important for those affected by CKD to consult with a renal dietician when making changes in their diets or starting a new treatment plan.
This table outlines the key areas where renal dietitians provide invaluable support for CKD patients:
| Area | Role of a Renal Dietitian |
| Mineral supplementation | Assessing mineral levels and providing guidance on supplementing as needed |
| Weight management | Developing dietary plans to promote weight loss or gain as needed |
| Fluid monitoring | Monitoring fluid intake and helping patients avoid dehydration or overhydration |
| Carbohydrate counting | Helping patients monitor carbohydrate consumption to prevent spikes in blood glucose levels |
| Vitamin intake | Assisting with vitamin requirements for proper nutrition and health maintenance |
Renal nutritionists create individualized eating plans for each patient based on their specific needs, accounting for factors like appetite, lifestyle, food preferences, existing medical conditions, medications taken, etc. The goals of these plans are to ensure adequate calories and nutrition while keeping blood sugar levels within normal ranges.
In addition to providing one-on-one counseling sessions about healthy eating habits, renal dietitians also conduct educational workshops that teach CKD patients how to plan meals that meet their dietary restrictions.
Having access to a specialized renal dietitian is an important part of managing CKD effectively. With the right guidance from a professional in this field, people living with CKD can make informed decisions about what they eat.
How Renal Dietitians Help in Personalized Diet Planning
You need personalized guidance to ensure you're getting the nutrition you need to manage your condition and stay healthy, renal nutritionists can help you achieve that. They understand the complexities of chronic kidney disease and other renal conditions, and are equipped with the knowledge necessary to create a tailored menu plan for each individual patient.
With their expertise, they can recommend food choices, portion sizes, fluid restriction, sodium limits, phosphorus sources, potassium foods, and protein sources that meet your specific needs.
Renal dietitians provide a special type of support by helping CKD patients learn more about their condition so they can make informed dietary decisions. They also teach strategies for meal planning and provide practical advice on how to follow a renal-friendly meal plan within budgetary constraints. This helps patients optimize their nutrient intake while still enjoying meals they like.
Renal nutritionists collaborate with nephrologists and other healthcare providers in order to develop the most effective treatment plans for CKD patients. By providing personalized nutrition counseling they enable patients to take an active role in managing their own health, this is important for improving quality of life as well as long-term prognosis outcomes.
| Fluid Restriction | Phosphorus Sources | Sodium Limits |
| Decrease intake of liquids per day (e.g., tea/coffee without sugar or milk) Avoid sugary drinks & alcohol | Bake goods made from white flour Dairy substitutes such as soy milk Non-dairy creamer & butter | Limit processed and canned foods Don't add salt when cooking or seasoning Avoid salty snacks such as chips/crisps |
| High Potassium Foods | Protein Sources | |
| Leafy greens (spinach & kale) Fruits (bananas & apples) Beans & lentils | Fish & seafood Lean poultry & meat Eggs |
The Importance of Protein Management in CKD
Managing protein intake is crucial for individuals with chronic kidney disease (CKD) due to the kidneys' diminished ability to effectively filter waste products. Protein is an essential nutrient that helps build and repair tissues, maintain muscle mass, and support various bodily functions.
However, in CKD, excessive protein intake can increase the workload on the kidneys and contribute to the buildup of waste products in the body.
Reducing protein intake is important for several reasons. Firstly, it helps decrease the production of waste products, such as urea and creatinine, which are normally filtered out by the kidneys. By limiting protein intake, the kidneys have less waste to process, reducing the strain on their compromised function.
Secondly, excessive protein intake can lead to the accumulation of non-essential amino acids, which can be harmful to individuals with CKD. These amino acids can produce toxins and increase the risk of complications such as uremia, which is characterized by symptoms like nausea, fatigue, and poor appetite.
Furthermore, a high-protein diet can contribute to the progression of CKD. Research suggests that excess protein intake can accelerate the decline in kidney function in individuals with pre-existing kidney disease. By moderating protein consumption, the progression of CKD can be slowed, potentially delaying the need for dialysis or kidney transplantation (questions about kidney transplant?).
However, it is important to note that protein restriction should be carefully managed, as some protein intake is still necessary to meet nutritional needs. Working with a registered dietitian or healthcare professional specializing in CKD is crucial to determine an appropriate protein intake based on individual factors such as the stage of CKD, nutritional status, and presence of other health conditions.
Hence, managing protein intake is vital for individuals with chronic kidney disease. It helps reduce the workload on the kidneys, minimizes the accumulation of waste products, and can slow the progression of the disease.
A personalized approach to protein intake, guided by healthcare professionals, ensures that individuals with CKD receive adequate nutrition while protecting their kidney function (improving kidney function with diet).
Balancing Sodium and Potassium Levels in CKD
Balancing sodium and potassium levels is crucial for patients with chronic kidney disease (CKD) due to the kidneys' impaired ability to regulate electrolytes. Sodium and potassium are essential electrolytes that play vital roles in maintaining fluid balance, nerve function, and muscle contraction. However, imbalances in these electrolytes can have detrimental effects on individuals with CKD.
Sodium intake should be carefully managed in CKD patients because excessive sodium can lead to fluid retention and high blood pressure. High blood pressure is a common complication of CKD and can further damage the kidneys.
Restricting sodium intake helps control fluid buildup and reduces the risk of hypertension. A low-sodium meal plan, combined with appropriate medication management, can help maintain blood pressure within a target range and preserve kidney function (high blood pressure and kidney disease).
On the other hand, potassium balance is crucial because impaired kidney function can lead to hyperkalemia, which is characterized by elevated levels of potassium in the blood. Hyperkalemia can cause dangerous cardiac arrhythmias and, in severe cases, cardiac arrest.
Therefore, monitoring and regulating potassium intake is vital for individuals with CKD. A diet that limits high-potassium foods such as bananas, oranges, tomatoes, potatoes, and certain legumes can help prevent potassium buildup in the bloodstream. Medications known as potassium binders may also be prescribed to assist in managing potassium levels.
It is important for individuals with CKD to work closely with a registered dietitian or healthcare professional specializing in kidney disease to develop an individualized, kidney friendly nutrition plan that balances sodium and potassium intake. Regular monitoring of electrolyte levels is necessary to ensure appropriate adjustments to the diet and medications.
In conclusion, maintaining a proper balance of sodium and potassium is essential for individuals with CKD. By managing sodium intake, fluid retention and high blood pressure can be controlled.
Similarly, regulating potassium levels helps prevent the risk of hyperkalemia and associated cardiac complications. A tailored diet plan, in collaboration with healthcare professionals, can effectively manage these electrolyte imbalances and contribute to the overall well-being of CKD patients.
Phosphorus Control in CKD: A Dietitian's Guide
Phosphorus control is a critical aspect of managing chronic kidney disease because impaired kidney function leads to difficulties in regulating phosphorus levels in the body. Phosphorus is a mineral that plays a vital role in bone health, energy production, and numerous cellular processes.
However, elevated levels of phosphorus in the blood, known as hyperphosphatemia, can occur in CKD and contribute to various complications.
In CKD, the kidneys are unable to effectively excrete excess phosphorus, resulting in its accumulation in the blood. This can lead to adverse effects such as bone and mineral disorders, cardiovascular disease, and an increased risk of mortality. Therefore, controlling phosphorus intake is crucial to prevent these complications.
A renal nutritionist plays a pivotal role in guiding individuals with CKD to manage their phosphorus intake effectively. They possess specialized knowledge and expertise in renal nutrition and can provide tailored dietary recommendations based on the stage of CKD, lab results, medications, and individual preferences.
A renal dietitian can help CKD patients identify high-phosphorus foods and make appropriate dietary adjustments. They educate patients on selecting lower-phosphorus alternatives and advise on portion sizes to maintain phosphorus balance. Additionally, they assist in understanding food labels to identify hidden sources of phosphorus, such as additives and preservatives.
Furthermore, a renal dietitian can help patients navigate complex dietary restrictions associated with phosphorus control, especially considering that many high-phosphorus foods are also sources of protein, which needs to be moderated in CKD. They work closely with patients to develop meal plans that strike a balance between phosphorus restriction and meeting other nutritional needs.
Regular monitoring of phosphorus levels is essential, and a renal dietitian can help patients interpret lab results and make necessary adjustments to their custom plan for meals. They can also collaborate with other members of the health care team, such as nephrologists and pharmacists, to ensure comprehensive management of phosphorus control.
Therefore, phosphorus control is crucial in CKD to prevent complications associated with hyperphosphatemia. Guidance from a renal dietitian is invaluable as they provide specialized knowledge, personalized dietary recommendations, and ongoing support.
Working with a renal nutritionist empowers individuals with CKD to effectively manage their phosphorus intake, optimize nutritional balance, and enhance overall health outcomes.
The Impact of Fluid Intake on Kidney Health
Fluid management is an important aspect of care for patients with chronic kidney disease. Impaired kidney function in CKD can lead to difficulties in regulating fluid balance, resulting in fluid retention, swelling (edema), and increased blood pressure. Effective fluid management plays a crucial role in preventing complications and promoting overall well-being in CKD patients.
Renal dietitians play a vital role in guiding individuals with CKD in fluid management. They possess specialized knowledge and expertise in renal nutrition and can provide personalized recommendations based on the stage of CKD, individual needs, and specific medical considerations.
One of the primary goals of fluid management is to maintain a balance between fluid intake and output. Renal nutritionists can help patients determine their fluid allowance, which is based on factors such as urine output, residual kidney function, and presence of other health conditions.
They provide education on monitoring fluid intake, including guidance on the appropriate volume of fluids from various sources such as beverages, foods, and medications.
Renal nutritionists also help patients identify fluid sources that should be limited or avoided. This includes beverages that are high in sodium or potassium, such as carbonated drinks, sports drinks, and certain fruit juices (low potassium side dishes).
They work closely with patients to develop strategies for reducing fluid intake while still meeting nutritional needs. This may involve educating patients on portion control, incorporating foods with higher water content, and finding alternative ways to enhance food flavor without excessive fluid intake.
In addition to fluid restriction, renal dietitian nutritionists assist patients in understanding the signs and symptoms of fluid overload and when to seek medical attention. They play a critical role in educating patients about self-monitoring, including the importance of regular weight checks and how weight changes can indicate fluid retention.
Collaboration between renal nutritionists and other healthcare professionals is essential for comprehensive fluid management in CKD. Renal dietitians work closely with nephrologists, nurses, and other members of the healthcare team to ensure a cohesive approach to fluid management. They provide ongoing support, monitor fluid-related parameters, and adjust recommendations as the patient's condition changes.
In all, fluid management is a crucial aspect of care for patients with CKD. Renal dietitians play an instrumental role in guiding individuals to achieve optimal fluid balance.
Through personalized recommendations, education, and ongoing support, renal nutritionists empower CKD patients to make informed choices about fluid intake, prevent complications associated with fluid overload, and promote overall health and well-being.
Dietary Adjustments for CKD Stages
Dietary adjustments play a critical role in managing chronic kidney disease (CKD) and its progression. Renal dietitians are instrumental in guiding patients through these adjustments, providing personalized recommendations and ongoing support. Here is a summary of dietary adjustments throughout the different stages of CKD and the role of renal dietitians:
Stages 1 and 2 CKD: Renal dietitians work with patients to adopt a healthy eating pattern, such as the DASH diet. They provide guidance on balanced nutrition, portion control, and the importance of maintaining a healthy weight. Renal nutritionists educate patients about sodium and sugar intake and help them make informed choices about food selection.
Stage 3 CKD: Renal dietitians focus on protein moderation to reduce the workload on the kidneys. They provide individualized protein recommendations based on the patient's stage of CKD, nutritional status, and other health factors.
Renal dietitians also assist patients in monitoring and managing sodium, potassium, and phosphorus intake to maintain fluid balance, control blood pressure, and prevent complications associated with electrolyte imbalances.
Stage 4 and 5 CKD (pre-dialysis): Dietary adjustments become more restrictive at these stages of advanced kidney disease, and renal dietitians play a crucial role in guiding patients through the complexities. They provide detailed recommendations on protein restriction, sodium and potassium control, and phosphorus management.
Renal nutritionists help patients navigate food choices, portion sizes, and label reading to identify hidden sources of sodium, potassium, and phosphorus. They educate patients on the importance of adhering to dietary restrictions and assist in developing practical strategies to maintain a well-balanced diet while meeting individual nutritional needs.
Stage 5 CKD (on dialysis): Renal dietitians work closely with patients undergoing dialysis to adjust their diet according to the dialysis regimen. They provide guidance on increased protein needs, sodium and fluid restriction, phosphorus and potassium control, and monitoring of fluid gains between dialysis sessions.
Renal dietitians help patients optimize their nutrition during dialysis treatment and address any challenges they may face, such as dietary restrictions and food preferences.
Throughout all stages of CKD, renal dietitians empower patients by providing education, personalized recommendations, and ongoing support. They monitor patients' progress, assess lab results, and make necessary adjustments to the dietary plan.
Renal dietitians play a crucial role in guiding patients through the dietary adjustments required at each stage of CKD. Their expertise in renal nutrition, personalized recommendations, and ongoing support contribute significantly to the management of CKD, helping patients optimize their nutrition, slow disease progression, and improve overall health outcomes.
Lifestyle Changes Recommended by Renal Dietitians
Making lifestyle changes can help you manage your advanced Chronic Kidney Disease, so it is important to consult a renal nutritionist for tailored advice and guidance. The table below outlines tips and techniques for making beneficial lifestyle plans that will support your dialysis treatments:
| Food Choices | Lifestyle Modifications | Stress Management |
| Reduce sodium intake. | Exercise regularly. | Practice mindfulness. |
| Increase potassium intake. | Get adequate sleep every night. | Take breaks and relax throughout the day. |
| Avoid processed foods & sugary drinks. | Manage fluid intake according to doctor's instructions. | Talk to family or friends about how you feel when needed . |
| Monitor protein & phosphorus levels in meals & snacks everyday. | Attend regular appointments with healthcare professionals for monitoring health status, medication needs, etc. |
Additionally, renal dietitians may recommend vitamin supplementation and tracking food choices on a daily basis as part of a well-rounded treatment plan for managing advanced CKD symptoms. Taking the time to make these changes can help ensure that dialysis treatments are as effective as possible while helping to maintain overall health and wellbeing during this difficult time period in life!
Additional Resources For Renal Dietitian Advice
There is more than one way to seek the advice of a renal dietitian. The first and probably best way is to seek a referral from your own physician. Often they will work closely with a renal nutritionist to ensure you are getting the best treatment.
This is always the best option because every patient is different. What works for someone else may not be the best option for you because your case may differ from someone else.
There is always an abundance of information, meal plans, articles and more at your disposal through a variety of websites. Some of these websites even offer a community option, where you can talk to other patients as well as physicians and renal dietitians.
However you seek the advice of a renal dietitian, make sure that you run everything you do through your physician. Especially if you are making changes to your eating or lifestyle changes, your doctor needs to not only approve the changes according to your particular health but also to document what works best for you.
All in all, you can learn a lot from a renal dietitian regarding your health and how your diet affects it. For more information on a renal diet from a renal dietitian, click here.
Frequently Asked Questions
Chronic kidney disease poses several potential risks to individuals. These include a decline in kidney function over time, leading to end-stage renal disease (ESRD) requiring dialysis or kidney transplantation. CKD also increases the risk of cardiovascular disease, including heart attacks and strokes.
Other complications may include high blood pressure, anemia, bone disorders, electrolyte imbalances, fluid overload, and compromised immune function. CKD can impact overall health and quality of life, necessitating close monitoring, medical management, and lifestyle modifications to mitigate these risks.
The frequency of visits to a renal dietitian may vary depending on individual circumstances and the stage of chronic kidney disease. In general, it is recommended to have regular visits with a renal dietitian, especially during the early stages of CKD.
Initially, more frequent nutritionist engagements may be necessary for comprehensive education, nutritional counseling, and dietary planning. As the individual becomes more knowledgeable and comfortable with their dietary adjustments, the visits may become less frequent.
However, ongoing periodic visits are essential for monitoring progress, adjusting the diet with kidney disease as needed, addressing concerns, and ensuring continued support and guidance in managing the nutritional aspects of CKD.
Dietary supplements for chronic kidney disease management should be approached with caution and only under the guidance of a healthcare professional.
While some supplements may be recommended in specific cases to address nutrient deficiencies, it is essential to assess individual needs and consider potential interactions with medications and the risk of harm.
Commonly recommended supplements include vitamin D, iron, and certain B vitamins. However, each patient's situation is unique, and consulting with a renal dietitian or healthcare provider is crucial to determine if and which supplements may be appropriate for their specific CKD condition.
Self-supplementation without professional guidance may lead to unintended consequences and potential harm.
Special dietary considerations for elderly chronic kidney disease patients may be necessary due to factors such as age-related physiological changes, comorbidities, and medication interactions.
Common considerations include adjusting protein intake based on individual needs, managing sodium and fluid intake to prevent fluid overload and hypertension, monitoring potassium and phosphorus levels, and ensuring adequate nutritional intake to prevent malnutrition.
Elderly CKD patients may also benefit from regular visits with a renal dietitian to assess their specific needs, provide education, and make appropriate dietary adjustments.
Collaboration with healthcare providers is essential to address the unique challenges and optimize the nutritional management of CKD in the elderly population.
Yes, the advice provided by a renal dietitian is different from that of a regular dietitian due to the specialized focus on managing chronic kidney disease. Renal dietitians have in-depth knowledge and expertise in renal nutrition and are trained to provide tailored dietary recommendations specific to the needs of individuals with CKD.
They consider factors such as the stage of CKD, lab results, medications, and other medical conditions when developing dietary plans. Renal dietitians are familiar with the complexities of managing protein intake, sodium and fluid restrictions, potassium and phosphorus control, and other nutritional considerations unique to CKD, ensuring optimal management of the disease through nutrition.
A Renal Dietitian’s Guidance Can Make A World Of Difference In Your CKD Management
As a CKD patient, you can count on the expertise of a renal dietitian to provide you with tailored advice and personalized meal plans. They can also help you become more aware of your fluid intake and protein management (why low protein diet in kidney disease).
In addition to providing guidance on dietary adjustments at each stage of CKD, a renal dietitian is an invaluable resource. With their support, you'll be able to make the necessary lifestyle changes for improved kidney health. Don't hesitate to take advantage of this resource in order to achieve better outcomes in your treatment plan.
With the guidance of a renal dietitian, you have a better chance at an improved quality of life even with chronic kidney disease.