Renal Diet Questions
Chronic kidney disease (CKD) is a serious medical condition. With proper diet, planning and treatments, however, it can be managed effectively. Still, it’s normal to have questions about CKD, since you would want to know the ins and outs of the diagnosis.
Aside from CKD itself, one of the most puzzling aspects of management is the renal diet. Hence, you may also have questions around it.
In this article, we’ll discuss some of the most common questions that patients ask their doctors about CKD and the Renal Diet

Jump to:
- Key Takeaways
- All About Chronic Kidney Disease
- What is a renal diet and how does it support kidney function?
- Which foods are restricted or limited in a renal diet?
- How does sodium intake affect kidney function?
- How important is it to monitor potassium and phosphorus levels?
- How does protein intake impact kidney health?
- Are there specific fluid restrictions I should be aware of?
- How do I adjust my diet if I'm on dialysis?
- Are there any supplements or medications that can help manage nutrient levels?
- Are there any specific lab values or tests I should monitor regularly?
- How often should I get my kidney function and nutrient levels tested?
- Where can I find renal diet recipes and meal plans?
- How advanced is my kidney disease, and how does it specifically impact my dietary needs?
- What medication interactions should I be aware of if I am on a renal diet?
- Given my overall health and other medical conditions, are there additional dietary considerations I should be aware of?
- What signs or symptoms should prompt me to seek immediate medical attention or adjustments in my renal diet?
- Is It Possible to Follow a Vegetarian or Vegan Renal Diet?
- How Can I Manage My Cravings for Foods That Are Not Recommended in a Renal Diet?
- Are There Any Specific Physical Activities or Exercises That Can Support a Renal Diet and Kidney Health?
- Do You Have Questions About CKD and the Renal Diet? Don’t Hesitate To Ask!
Key Takeaways
- Renal diet is a specialized dietary plan for managing kidney disease and supporting kidney function.
- High-protein foods like red meat, poultry, and dairy products should be limited in a renal diet.
- Sodium plays a significant role in fluid balance and blood pressure, and overconsumption can lead to hypertension and kidney disease.
- Balancing potassium and phosphorus levels is crucial for maintaining kidney health, and certain foods should be limited in kidney disease.
All About Chronic Kidney Disease
What is chronic kidney disease?
Chronic kidney disease is a progressive medical disorder in which the kidneys lose the ability to function properly. The condition typically comes on in five stages, and the advancement of stages varies between patients.
As the patient’s condition worsens, the ability of the kidneys to filter waste from the blood is lessened. In its final stage, known as end stage renal disease (ESRD), the patient requires dialysis or a kidney transplant in order to live.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.

What are the causes of CKD?
Most (about ⅔) of the cases of CKD in the U.S. are caused by two primary factors. The first is diabetes – as high blood sugar levels can be damaging to the kidneys over time. High blood pressure is the second, and when not treated, it can cause damage to your blood vessel including those in the kidneys.
What are the symptoms of CKD?
Many chronic kidney disease sufferers don’t have symptoms in the earlier stages. It can be a “silent” disorder until profound kidney damage has occurred.
Signs you may be suffering from CKD include high blood pressure, severe fatigue, loss of appetite, muscle cramps during rest, changes in amount of urine, sleep problems, swelling in the feet and ankles, and trouble concentrating.
How is CKD diagnosed?
Your doctor will begin by doing a personal and family health assessment. Your doctor will take note of your symptoms, and may ask if you suffer from high blood pressure. A physical exam is also performed, checking for signs of blood vessel issues.
To accurately diagnose chronic kidney disease, a series of tests may be given. These include a blood test to check the creatinine and urea levels in the blood, a urine test to check for abnormalities that may indicate CKD, and an ultrasound to check the kidneys’ size and structure.
Is there a cure for CKD?
While there is no cure for chronic kidney disease, there are treatments that can help you manage and treat the condition. The method of treatment prescribed to you by your doctor will depend on the underlying cause of the CKD.
You may be given medicine to reduce blood pressure, cholesterol, and swelling. It’s also common to be placed on a renal diet (daily renal diet menu plan) that is low in protein when you are suffering from CKD. Lower levels of protein allow your kidneys a break from working so hard to filter wastes.
What happens in the final stage of CKD?
If you progress to the last stage of the condition, known as end stage renal disease (ESRD Prognosis), your kidneys have reached complete and permanent failure in working for your body. The result may require dialysis, which is the process of using a machine to remove wastes and fluids from the blood.
Questions about kidney transplant? A kidney transplant may also be an option for some patients with ESRD. You will also need to take medication with a kidney transplant, to prevent your body from rejecting the organ.
What is a renal diet and how does it support kidney function?
A renal diet, also known as a kidney diet, is a specialized eating plan designed for individuals with kidney disease, particularly those with impaired kidney function. It involves careful management of protein, sodium, potassium, phosphorus, and fluid intake to reduce the strain on the kidneys and maintain overall health.
A renal diet aims to minimize waste buildup in the bloodstream, control blood pressure, and manage electrolyte imbalances, all of which are common challenges for individuals with kidney disease.
This dietary regimen is typically tailored to the patient's specific stage of kidney disease and individual medical needs, with the guidance of a renal dietitian or healthcare provider.
Renal Diet: Key Benefits
A renal diet offers several key benefits for individuals with kidney disease:
- Kidney Function Preservation: It helps reduce the workload on the kidneys by controlling protein intake, which minimizes waste product buildup and preserves kidney function.
- Blood Pressure Management: A renal diet is low in sodium (how much sodium per day for renal diet), helping to regulate blood pressure, a crucial factor in kidney health. Lower blood pressure reduces the risk of kidney damage.
- Electrolyte Balance: By monitoring potassium and phosphorus levels, a renal diet prevents dangerous imbalances that can lead to complications such as heart problems and bone disorders.
- Symptom Control: Managing fluid intake helps prevent fluid overload, alleviating symptoms like swelling, high blood pressure, and shortness of breath.
- Improved Quality of Life: A well-planned renal diet can enhance overall well-being, reduce complications, and empower individuals to take an active role in managing their kidney disease effectively.
Which foods are restricted or limited in a renal diet?
In a renal diet, several foods are restricted or limited due to their impact on kidney function and electrolyte balance. These include:
- High-Protein Foods: Excessive protein intake can lead to increased waste product production, so foods like red meat, processed meats, and high-protein dairy products are often restricted.
- High-Sodium Foods: Sodium can raise blood pressure and cause fluid retention, so salty foods like canned soups, processed snacks, and restaurant/fast-food items are limited.
- High-Potassium Foods: Elevated potassium levels can be harmful to the heart, so foods like bananas, oranges, potatoes, and tomatoes are restricted.
- High-Phosphorus Foods: Excess phosphorus can lead to bone and heart problems, so foods like dairy products, colas, and certain beans are limited.
- High-Sugar Foods: Sugary items can contribute to weight gain and diabetes, which can further harm kidney function, so they are generally restricted.
- Fluids: Fluid intake, including water, is controlled to prevent fluid overload and swelling. The amount allowed varies based on individual circumstances.
A renal diet focuses on balancing these nutrients and monitoring portion sizes to maintain optimal kidney function and overall health in individuals with kidney disease. Consulting with a renal dietitian helps customize dietary restrictions to suit each patient's specific needs.
How does sodium intake affect kidney function?
Sodium intake significantly affects kidney function. The kidneys play a vital role in regulating sodium levels in the body. When sodium levels in the blood rise, it attracts water, increasing blood volume. This, in turn, elevates blood pressure. High blood pressure can damage blood vessels in the kidneys, reducing their ability to function effectively.
Moreover, consuming excess sodium can lead to fluid retention, increasing the workload on the kidneys. Over time, this can strain kidney function, potentially causing damage. In individuals with existing kidney disease, excessive sodium can worsen their condition. Damaged kidneys struggle to eliminate excess sodium (renal diet sodium limit), leading to further complications.
Reducing sodium intake through dietary modifications is a crucial aspect of managing kidney health, especially for individuals at risk of kidney disease or those already diagnosed with kidney issues. It helps maintain blood pressure within a healthy range and eases the burden on the kidneys, preserving their function.
How important is it to monitor potassium and phosphorus levels?
You're about to delve into the significance of balancing your body's potassium and phosphorus levels. This might seem like a daunting task, but it's crucial for maintaining optimal health, particularly when it comes to kidney function.
We'll break down how these two elements interact within the body, why balance is key, and what can happen if they're out of sync - an essential discussion that you won't want to miss. Here are some tips for a low potassium diet.
How important is it to monitor potassium levels?
Monitoring potassium levels is of paramount importance, especially for individuals with kidney disease. Potassium is an electrolyte that plays a crucial role in muscle and nerve function, including the heart. However, maintaining proper potassium balance is vital for overall health. Yes, there are some high potassium foods to avoid.
Abnormal potassium levels can disrupt the heart's rhythm, leading to arrhythmias or even cardiac arrest, which is especially concerning for kidney disease patients who may have difficulty regulating potassium. Additionally, potassium imbalances can result in muscle weakness, nerve issues, and can serve as an indicator of kidney dysfunction.
Regular blood tests and adherence to dietary recommendations for potassium intake are critical in managing these levels effectively and preventing serious health complications.
How important is it to monitor phosphorus levels?
Monitoring phosphorus levels is critical, particularly for individuals with kidney disease. Phosphorus is an essential mineral involved in various bodily functions, including bone health, energy production, and cell maintenance. Maintaining proper phosphorus balance is vital because elevated levels can lead to several issues.
High phosphorus levels can result in calcium removal from bones, weakening them and increasing the risk of fractures. Moreover, excessive phosphorus is linked to cardiovascular problems, including heart disease (ckd and heart disease) and blood vessel calcification.
In kidney disease, impaired kidney function can hinder the removal of excess phosphorus, causing levels to rise. Regularly monitoring phosphorus levels and adhering to dietary recommendations is essential for preventing complications and maintaining overall health, particularly for those with compromised kidney function.
How does protein intake impact kidney health?
Protein intake significantly impacts kidney health, and its management is crucial for individuals with kidney disease. Proteins are essential for various bodily functions, but their metabolism produces waste products like urea and creatinine, which the kidneys must filter and excrete.
Here's how protein intake affects kidney health and the adjustments needed as kidney disease progresses, especially for those on dialysis:
- Early Stages of Kidney Disease: In the early stages, protein intake is usually moderated to strike a balance between providing necessary nutrients and not overburdening the kidneys. High protein intake can increase the workload on the kidneys and potentially accelerate the progression of kidney disease.
- Advanced Kidney Disease (Dialysis): As kidney function declines to the point where dialysis is necessary, protein requirements may increase. Dialysis itself removes waste products from the blood, but it can also lead to protein loss during treatments. Therefore, many individuals on dialysis may require slightly higher protein intake to compensate for these losses and to prevent malnutrition and muscle wasting.
- Monitoring and Adjustments: Protein intake is carefully monitored and adjusted based on the stage of kidney disease, residual kidney function, and the individual's specific nutritional needs. Regular assessments by a renal dietitian are essential to determine the appropriate protein intake for each patient.
- High-Quality Protein: Emphasis is placed on consuming high-quality protein sources like lean meats, fish, poultry, and egg whites, as they produce fewer waste products during metabolism compared to protein from plant sources.
Protein intake impacts kidney health, and the amount of protein needed can vary depending on the stage of kidney disease and whether a person is on dialysis.
Individualized dietary plans, guided by healthcare professionals, help strike the right balance between maintaining nutritional needs and preserving kidney function.

Are there specific fluid restrictions I should be aware of?
Fluid restrictions in the context of Chronic Kidney Disease are an essential aspect of managing the condition. These restrictions are tailored to an individual's specific stage of CKD and their residual kidney function. Here's what you should be aware of:
- Individualized Guidelines: Fluid restrictions are not one-size-fits-all. They are highly individualized and determined by your healthcare provider or renal dietitian. They take into account your stage of CKD, the presence of other health conditions, and your overall health status.
- Preventing Fluid Overload: CKD can impair the kidneys' ability to regulate fluid balance effectively. Excessive fluid intake can lead to fluid overload, causing symptoms like swelling, high blood pressure, and difficulty breathing. Fluid restrictions are designed to prevent these complications.
- Monitoring Fluid Intake: Adhering to prescribed fluid restrictions requires diligent monitoring of your fluid intake. Keeping a fluid journal can help you keep track of how much you are consuming daily.
- Thirst Management: Managing thirst is part of fluid restriction. Your healthcare team can provide strategies to help you control thirst without exceeding your fluid allowance.
Fluid restrictions in CKD are essential for preventing fluid overload and preserving kidney function. Working closely with your healthcare team is crucial to ensure you receive personalized guidance that aligns with your specific health needs and stage of CKD.
How do I adjust my diet if I'm on dialysis?
The transition from a pre-dialysis renal diet to a dialysis diet involves significant dietary adjustments to accommodate the needs of individuals with End-Stage Renal Disease (ESRD Prognosis) who are undergoing regular dialysis treatments. Here's a comprehensive overview of the dietary changes and the transition process:
Dietary Adjustments for Dialysis:
- Protein Intake: During dialysis, protein needs often increase to compensate for protein losses during treatment. This adjustment helps prevent malnutrition and muscle wasting. High-quality protein sources like lean meats, poultry, fish, and egg whites are emphasized.
- Fluid Restrictions: Dialysis patients usually have strict fluid restrictions. Managing thirst is crucial, and drinking within the prescribed limits is essential to avoid fluid overload.
- Sodium Control: Sodium intake is limited to manage blood pressure and fluid balance. Reducing or avoiding high-sodium processed foods is critical.
- Potassium and Phosphorus Control: Managing these electrolytes is vital for heart and bone health. Foods high in potassium (e.g., bananas) and phosphorus (e.g., dairy products) are limited.
Transition Process:
- Collaboration with Healthcare Team: The transition should be a collaborative effort with your healthcare provider, renal dietitian, and dialysis care team. They will assess your individual needs and adjust your diet accordingly.
- Education: You will receive comprehensive education on the dietary changes, including portion control, food choices, and meal planning. This education helps you understand the importance of adhering to your new diet.
- Monitoring: Regular monitoring of lab values (e.g., potassium, phosphorus, and albumin) ensures that dietary adjustments are effective and tailored to your specific needs.
- Support: Seek support from support groups or dietitians who specialize in renal nutrition. They can provide valuable guidance and practical tips for managing the transition effectively.
The transition to a dialysis diet requires dedication and adherence to dietary restrictions, but it is essential for maintaining overall health and managing the unique challenges that ESRD presents.
Collaborating with healthcare professionals and staying informed about your dietary requirements will help you successfully navigate this transition.
Are there any supplements or medications that can help manage nutrient levels?
Yes, there are supplements and medications commonly used to manage nutrient levels in individuals with Chronic Kidney Disease (CKD) and especially in those on dialysis. These include:
- Phosphate Binders: People with advanced CKD or those on dialysis often experience elevated phosphorus levels. Phosphate binders are medications that help control phosphorus absorption from the diet by binding to dietary phosphates in the digestive tract. This prevents them from being absorbed into the bloodstream.
- Calcium Supplements: CKD patients may experience low calcium levels, which can lead to bone problems. Calcium supplements are prescribed to maintain proper calcium levels. However, these supplements should be used under close medical supervision to avoid calcium overload, which can occur in individuals with impaired kidney function.
- B-Complex Vitamins: CKD patients may have lower levels of B-complex vitamins, including B1 (thiamine), B6 (pyridoxine), and B12 (cobalamin), due to dietary restrictions. B-complex supplements can help address these deficiencies.
- Amino Acid Supplements: In cases of malnutrition or muscle wasting, amino acid supplements may be recommended to provide essential protein building blocks.
It's essential to emphasize that these supplements and medications should only be taken under the guidance of a healthcare provider or renal dietitian. They are prescribed based on individual needs and the specific nutrient imbalances identified through blood tests.
Self-supplementation can lead to unintended consequences, so it's crucial to work closely with your healthcare team to determine the appropriate supplements and dosages for your unique circumstances. Regular monitoring of nutrient levels through blood tests is essential to ensure the effectiveness and safety of these interventions.
Are there any specific lab values or tests I should monitor regularly?
If you have Chronic Kidney Disease (CKD) and are following a renal diet, regular monitoring of specific lab values and tests is crucial to ensure your health and the effectiveness of your dietary management. Here are some key parameters to monitor:
- Estimated Glomerular Filtration Rate (eGFR meaning): eGFR is a critical measure of kidney function. It helps determine the stage of CKD and guides treatment decisions. Regular eGFR tests are essential to track changes in kidney function over time.
- Serum Creatinine: This blood test provides additional information about kidney function and helps eGFR. It's important to monitor serum creatinine levels regularly.
- Serum Albumin: Albumin is a protein in the blood, and low levels can indicate malnutrition or inflammation. Regular monitoring helps assess your nutritional status.
- Serum Phosphorus and Calcium: These tests help evaluate bone health and the effectiveness of phosphate binders, phosphorus restriction, and calcium supplements in your renal diet.
- Serum Potassium: High potassium levels (hyperkalemia) can be dangerous. Monitoring potassium is crucial, especially if you have stage 3 or higher CKD.
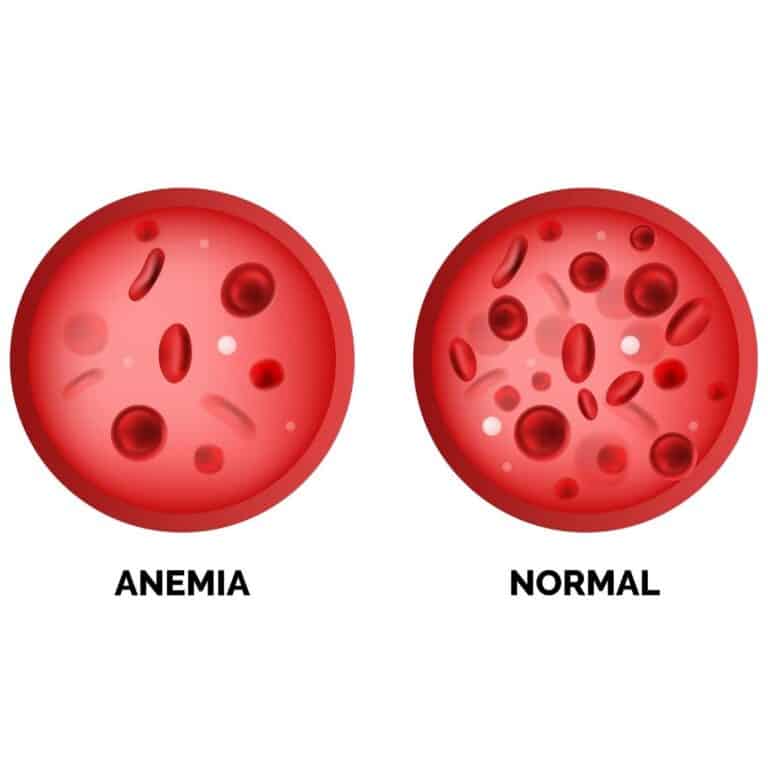
- Hemoglobin and Hematocrit: Anemia is common in CKD due to decreased production of erythropoietin. Regular monitoring helps guide treatment with erythropoiesis-stimulating agents or iron supplements.
- Urine Protein: Proteinuria (excess protein in urine) can indicate kidney damage. Regular urine protein tests help assess kidney health.
- Urine Creatinine Clearance: This test provides information about the rate at which your kidneys are filtering waste. It helps determine the severity of kidney dysfunction.
Monitoring these lab values and tests in coordination with your healthcare provider or renal dietitian is essential for managing CKD effectively and making timely adjustments to your renal diet and medication regimen as needed. Feel free to study what chronic kidney disease laboratory tests mean.
It allows for early detection of potential issues and helps ensure that your kidney disease is managed optimally.
How often should I get my kidney function and nutrient levels tested?
The frequency of kidney function tests and laboratory assessments for patients on a renal diet depends on several factors, including the stage of Chronic Kidney Disease, the presence of comorbidities, and individualized treatment plans. Here is a general guideline:
- Early Stages of CKD (Stages 1-3): In the early stages, when kidney function is relatively stable, kidney function tests (e.g., eGFR, serum creatinine) and laboratory assessments (e.g., serum albumin, calcium, phosphorus) are typically done every 3-12 months. The frequency may increase if there is a change in health status or treatment plan.
- Advanced CKD (Stages 4-5): As CKD progresses, and especially when approaching end-stage renal disease (ESRD), the frequency of testing usually increases. Tests are often done every 1-3 months to closely monitor kidney function, manage complications, and adjust medications and the renal diet accordingly.
- Dialysis Patients: For individuals on dialysis (hemodialysis or peritoneal dialysis), laboratory assessments are done more frequently, often before each dialysis session or at least monthly. This close monitoring ensures the adequacy of dialysis and helps manage nutrient imbalances.
- Post-Kidney Transplant: After a kidney transplant, kidney function tests and assessments are done more frequently initially to monitor graft function. Over time, the frequency may decrease but will still involve regular follow-ups.
- Individualized Assessments: Patients with CKD often have comorbidities like diabetes or hypertension, which require additional monitoring of related parameters such as blood glucose, hemoglobin A1c, and blood pressure.
Ultimately, the frequency of tests and assessments should be determined by your healthcare provider specifically your nephrologist based on your specific health status and treatment plan.
Regular monitoring is essential for timely intervention, ensuring that your renal diet and medications are effective, and addressing any complications that may arise as CKD progresses.
Where can I find renal diet recipes and meal plans?
Navigating the complexities of a renal diet can be daunting, but you're not alone in your journey. With an array of resources at your fingertips, finding tailored meal plans and recipes that align with your kidney health needs isn't as tough as it seems.
Let's delve into where you can find these valuable renal diet resources, ensuring each bite you take is one step closer to optimal kidney health.
Finding Renal Diet Resources
There's a wealth of renal diet resources available online and in print to help manage your kidney health. Renal cookbook suggestions are plentiful, offering diverse recipes tailored to reduce strain on the kidneys. Nutritionist consultations can provide personalized advice that fits your lifestyle and dietary needs.
Consider these resources:
- Renal cookbooks with meal plans suited for varying stages of kidney disease
- Consultations with nutritionists specializing in renal diets
- Support groups where you can share experiences, challenges, and solutions
- Lifestyle changes that positively impact kidney health, like exercise and quitting smoking
- Family meal adaptations making it easy for everyone at home to enjoy nutritious meals
How advanced is my kidney disease, and how does it specifically impact my dietary needs?
The stages of kidney disease, ranging from stage 1 to stage 5, are crucial determinants of the renal diet's composition and restrictions:
- Stage 1 (Kidney Damage, Normal GFR): In this early stage, kidney damage may exist, but kidney function is normal. The renal diet primarily focuses on preventing further damage by managing underlying conditions like diabetes or hypertension. Dietary adjustments may include controlling blood pressure and blood sugar levels.
- Stage 2 (Mild Kidney Damage): Kidney function remains normal, but there is mild kidney damage. The diet emphasizes maintaining overall health by controlling risk factors like hypertension, hyperlipidemia, and obesity. Sodium and protein intake may be moderately restricted.
- Stage 3 (Moderate Kidney Damage): Kidney function starts to decline in this stage. The renal diet becomes more restrictive, with sodium, potassium, and phosphorus intake being closely monitored. Protein intake may be adjusted to prevent further kidney damage.
- Stage 4 (Severe Kidney Damage): Kidney function significantly declines, and the renal diet becomes even more restrictive. Protein intake may need to increase to counter protein loss. Fluid intake is restricted, and careful management of potassium and phosphorus is critical.
- Stage 5 (End-Stage Renal Disease): At this point, kidney function is severely impaired, and many patients require dialysis or a kidney transplant. The diet becomes highly specialized, with strict restrictions on protein, sodium, potassium, and phosphorus. Fluid intake is severely limited to prevent fluid overload during dialysis.
Throughout all stages, close collaboration with a renal dietitian and healthcare provider is essential to tailor the diet to individual needs. Dietary adjustments aim to manage symptoms, slow disease progression (progression of symptoms for CKD), and maintain overall health as kidney function declines.
Regular monitoring and adherence to dietary recommendations are crucial for effective management of kidney disease.
What medication interactions should I be aware of if I am on a renal diet?
If you are on a renal diet, it's essential to be aware of potential medication interactions that can affect the absorption, metabolism, and elimination of drugs due to dietary restrictions or nutrient imbalances. Here are some key considerations:
- Phosphate Binders: Phosphate binders, commonly used in kidney disease management, can bind to medications and reduce their absorption. It's crucial to take medications either an hour before or several hours after taking phosphate binders to avoid interactions.
- Iron Supplements: Iron supplements, often prescribed for anemia in CKD, can interact with certain antibiotics, thyroid medications, and antacids. They should be taken separately from these medications to prevent reduced absorption.
- Vitamin and Mineral Supplements: Some supplements, like calcium and magnesium, can interact with medications, particularly antibiotics and certain heart medications. It's important to discuss the timing of supplement intake with your healthcare provider.
- Potassium-Binding Medications: If you are prescribed medications like sodium polystyrene sulfonate (Kayexalate) to manage high potassium levels, be cautious with high-potassium foods, as they can counteract the medication's effects.
- Sodium and Blood Pressure Medications: If you are on medications to control blood pressure, sodium intake should be closely monitored, as high sodium levels can interfere with the effectiveness of these medications.
- Grapefruit Juice: While not directly related to the renal diet, grapefruit juice can interact with various medications by affecting liver enzymes responsible for drug metabolism. Discuss the use of grapefruit products with your healthcare provider.
To avoid potential interactions, always inform your healthcare provider and pharmacist about your dietary restrictions and medications (diet vs medication for CKD improvement). They can provide guidance on the timing of medication administration and any necessary adjustments to your renal diet to ensure the safe and effective use of medications.
Given my overall health and other medical conditions, are there additional dietary considerations I should be aware of?
Patients on a renal diet with additional comorbidities should consider dietary factors beyond the standard restrictions for comprehensive health management. Specifically, they should focus on heart and gut health:
- Fatty Foods: Individuals with kidney disease and cardiovascular issues should be cautious about consuming high-fat foods. These can contribute to elevated cholesterol levels and increase the risk of heart-related complications. Opting for lean protein sources and healthy fats like those found in avocados and fatty fish can support heart health.
- Dietary Fiber: Incorporating dietary fiber is beneficial for both heart and gut health. High-fiber foods like fruits, vegetables, whole grains, and legumes can help regulate blood sugar, lower cholesterol levels, and promote healthy digestion. Adequate fiber intake can also prevent constipation, a common issue in kidney disease.
- Portion Control: Controlling portion sizes is crucial for managing weight and preventing overconsumption of calories, which can contribute to heart disease and obesity, both common comorbidities in kidney disease patients.
- Processed Foods: Reducing processed and convenience foods is advisable, as they often contain unhealthy fats, sodium, and additives that can exacerbate cardiovascular and digestive issues.
Patients should work closely with a renal dietitian to create a dietary plan that considers these factors while addressing their specific comorbidities. Regular monitoring and adjustments based on lab results and symptom management remain essential for achieving optimal health outcomes.
What signs or symptoms should prompt me to seek immediate medical attention or adjustments in my renal diet?
Several signs or symptoms should prompt individuals on a renal diet to seek immediate medical attention or dietary adjustments. These include:
- Sudden Swelling: If there is rapid and significant swelling of the legs, ankles, or face, it may indicate fluid overload, which can be dangerous for kidney patients.
- Shortness of Breath: Difficulty breathing or shortness of breath can result from fluid overload and is a serious concern, especially for those with heart issues.
- Chest Pain or Palpitations: Any chest discomfort, pain, or irregular heartbeats should be evaluated promptly, as they can signify heart strain or other cardiac problems.
- Confusion or Altered Mental State: Cognitive changes or confusion can be related to electrolyte imbalances, such as high potassium levels, and should be addressed urgently.
- Nausea and Vomiting: Persistent nausea and vomiting may signal a variety of issues, including electrolyte disturbances or medication side effects.
- Blood in Urine: The presence of blood in the urine can indicate kidney problems or other issues and should be investigated immediately.
- Severe Fatigue: Overwhelming fatigue can be a sign of anemia or worsening kidney function.
- Uncontrolled Blood Pressure: If blood pressure is consistently above recommended levels, it may require adjustments in medications or dietary sodium intake.
- Changes in Urine Output: Drastic changes in urine volume or color should be reported, as they can indicate kidney function changes.
- Cramping or Muscle Weakness: Muscle issues may relate to imbalances in minerals like potassium.
It's crucial for individuals on a renal diet to recognize these warning signs and promptly seek medical attention when they arise. Timely intervention can prevent complications, guide dietary adjustments, and improve overall health outcomes.
Additionally, regular communication with healthcare providers and renal dietitians is essential for addressing these symptoms and managing kidney disease effectively.
Is It Possible to Follow a Vegetarian or Vegan Renal Diet?
Yes, it is possible to follow a vegetarian or vegan renal diet, but it requires careful planning and monitoring of nutrient intake, particularly protein and certain minerals.
- Protein Sources: Vegetarians can obtain their protein from plant-based sources like legumes (beans, lentils, chickpeas), tofu, tempeh, and seitan. Vegans can include these sources as well as plant-based protein powders, nuts, and seeds.
- Phosphorus Control: Many plant-based foods are rich in phosphorus, which can be a concern for kidney patients. Careful selection and portion control of high-phosphorus foods like whole grains, nuts are necessary.
- Potassium Management: Plant-based diets can be high in potassium, so it's essential to limit potassium-rich foods like bananas, oranges, and potatoes.
- Sodium Restriction: Vegans and vegetarians should also be cautious about sodium intake, especially when using processed or packaged plant-based products.
- Nutrient Supplements: Depending on individual needs and lab results, supplements for essential nutrients like vitamin B12, iron, and omega-3 fatty acids may be required.
Consulting a renal dietitian is highly recommended for individuals following vegetarian or vegan renal diets. They can help create a customized meal plan that meets nutrient requirements while adhering to dietary restrictions.
Regular monitoring of lab results is crucial to ensure dietary adjustments are effective in managing kidney disease while adhering to vegetarian or vegan principles.
How Can I Manage My Cravings for Foods That Are Not Recommended in a Renal Diet?
Managing cravings for foods not recommended in a renal diet can be challenging but is crucial for your kidney health. Here are some strategies to help you deal with these cravings:
- Mindful Eating: Pay attention to your body's hunger and fullness cues. Before indulging in cravings, ask yourself if you're genuinely hungry or just craving the taste.
- Substitute Smartly: Find kidney-friendly alternatives that mimic the flavors or textures you crave. For example, if you crave salty chips, try baked whole-grain crackers with low-sodium dip.
- Portion Control: If you decide to indulge occasionally, practice portion control. Limit the quantity and frequency of forbidden foods to avoid excessive intake.
- Stay Hydrated: Sometimes, thirst can be mistaken for hunger or cravings. Drinking water can help quell cravings.
- Distraction: Engage in activities that divert your attention from cravings, such as taking a walk, reading, or pursuing a hobby.
- Support: Seek support from friends, family, or support groups. Sharing your challenges with others who understand can be motivating and reassuring.
Remember, managing cravings is a part of a long-term commitment to your kidney health. Consult with a renal dietitian for personalized advice and strategies tailored to your specific cravings and dietary restrictions.
Are There Any Specific Physical Activities or Exercises That Can Support a Renal Diet and Kidney Health?
Yes, physical activity and exercise can play a supportive role in maintaining kidney health and complementing a renal diet. Here's how:
- Improved Cardiovascular Health: Regular aerobic exercises like walking, jogging, or cycling can help manage blood pressure and reduce the risk of heart disease, common comorbidities in kidney disease.
- Weight Management: Staying physically active can help control body weight, which is important for overall health and can reduce the burden on the kidneys.
- Strengthening Muscles: Strength training exercises can help build and maintain muscle mass, which may be beneficial for kidney patients who often experience muscle wasting.
- Enhanced Blood Sugar Control: For individuals with diabetes and kidney disease, physical activity can help regulate blood sugar levels, reducing the risk of further kidney damage.
- Stress Reduction: Regular exercise can reduce stress, anxiety, and depression, which are common among kidney patients.
- Improved Overall Well-being: Exercise can boost energy levels, improve sleep quality, and enhance overall quality of life for individuals with kidney disease.
However, it's essential to consult with a healthcare provider or a renal dietitian before starting any exercise program, especially if you have advanced kidney disease or other health conditions. They can help you tailor an exercise plan that's safe and appropriate for your specific needs and limitations.
Do You Have Questions About CKD and the Renal Diet? Don’t Hesitate To Ask!
Managing your kidney health through a renal diet is crucial. It involves limiting certain foods and monitoring sodium, potassium, phosphorus, and protein intake.
Regular lab tests are key to track your ckd progression. Be mindful of how your medications interact with your diet, considering other health conditions too. Stay alert for any concerning symptoms that may require immediate attention or dietary adjustments.
Hopefully these common questions about chronic kidney disease shed some light on the condition for you. As always, consult with your doctor or read through the rest of our blog here if you need more information!