Hyperparathyroidism Diet Restriction
If you're living with both hyperparathyroidism and chronic kidney disease (CKD), you may be wondering what dietary restrictions are necessary to keep your condition in check. It's important to know that diet plays a significant role in managing these conditions, and understanding the relationship between the two can help you create a balanced diet plan that works for you.

In this article, we'll look at how to create an appropriate diet plan for hyperparathyroidism and CKD, as well as lifestyle changes that can help support it. We'll also provide tips on monitoring and adapting your diet over time with these two conditions (kidney diet plan).
Jump to:
- Key Takeaways
- Understanding Hyperparathyroidism and Chronic Kidney Disease (CKD)
- The Connection Between Hyperparathyroidism and CKD
- Importance of Diet in Managing Hyperparathyroidism and CKD
- Nutrients to Monitor in a Hyperparathyroidism and CKD Diet
- Calcium and Phosphorus Balance in Hyperparathyroidism and CKD
- Vitamin D and its Role in Hyperparathyroidism and CKD
- Management And Treatment of PTH and SHPT
- Protein Intake: A Key Consideration in Hyperparathyroidism and CKD
- Sodium and Fluid Restrictions in Hyperparathyroidism and CKD Diet
- What Should I Do About My SHPT?
- Creating a Balanced Diet Plan for Hyperparathyroidism and CKD
- Lifestyle Changes to Support a Hyperparathyroidism and CKD Diet
- Monitoring and Adapting Your Diet Over Time with Hyperparathyroidism and CKD
- FAQs for Secondary Hyperparathyroidism
- Diet Is Key In Managing Hyperparathyroidism
Key Takeaways
- Limit foods high in calcium, phosphorus, and sodium to reduce symptoms associated with hyperparathyroidism and chronic kidney disease.
- Pay attention to nutrient intake, including calcium, phosphorus, vitamin D, protein, sodium, potassium, and magnesium.
- Dietary adjustments can improve overall health by including anti-inflammatory foods like fruits, vegetables, legumes, and fish.
- Mindful tracking of food intake can help identify areas where dietary modifications are needed for effective management of hyperparathyroidism and chronic kidney disease.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding Hyperparathyroidism and Chronic Kidney Disease (CKD)
If you have hyperparathyroidism and CKD, understanding how the two conditions affect each other can help you make dietary changes that'll support your health. Hyperparathyroidism is caused by an overactive parathyroid gland, leading to increased calcium levels in the blood. Symptoms include fatigue, bone loss, and kidney stones.
Chronic Kidney Disease (CKD) is a progressive decrease in kidney function due to damage. It can be caused by infection, injury, or certain medical conditions.
Diagnosis and testing for both hyperparathyroidism and CKD involve physical exams, blood/urine tests, and imaging scans. Treatment for hyperparathyroidism may include medication or surgery to remove part of the abnormal tissue.
For those with CKD, treatment may involve lifestyle changes such as diet restrictions or dialysis treatments. Risk factors for developing either condition include age, family history, diabetes mellitus type 2, and hypertension.
It's important to take steps towards emotional support when dealing with these conditions, as depression and anxiety are common side-effects. Finding someone who understands what you're going through can be incredibly helpful in managing stress levels.
The key takeaway is that having hyperparathyroidism with chronic kidney disease requires careful consideration when making dietary choices. Understanding how they interact is essential when determining what food options best suit your individual needs within a healthy eating plan. This supports overall wellbeing through proper nutrition while reducing risk factors wherever possible.
The Connection Between Hyperparathyroidism and CKD
You're probably wondering how kidney disease and parathyroid issues are connected. Hyperparathyroidism is a condition in which the body produces too much of the hormone parathyroid hormone (PTH).
First, let me explain what SHPT (secondary hyperparathyroidism) is. Your parathyroid glands are responsible for keeping your bones and calcium levels in your blood at a healthy range. They are located in your neck on the back of your thyroid gland.
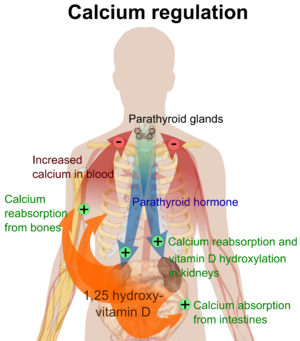
Most of the time, you don't even know they are there. They are near your thyroid gland, but work separately and produce PTH (Parathyroid hormone). PTH is responsible for maintaining the correct amount of calcium in the blood and bones, as well as ensuring optimal gastrointestinal absorption of calcium, and finally controlling urinary calcium excretion (That is the connection to kidney disease).
The amounts of other minerals that are part of bone growth - phosphorus and Vitamin D - are also critically important to the parathyroid. Doctors measure the amount of PTH as an indicator of bone disease.
Secondary Hyperparathyroidism (SHPT) as related to kidney disease is an overactive parathyroid hormone secretion. This is caused by renal insufficiency affecting other mineral levels in the blood and causing the body to overproduce PTH. In persons with CKD starting in stage 3, damage to the kidney affects the functioning of the kidney and causes these changes to possibly occur.
So, what causes the body to produce more PTH?
While that is a complicated question, I would like to answer it in a way that is easier to understand. Please remember - I am not your doctor!
Initially, your functioning kidney mass is decreased. This happens because of the damage over time to the nephrons in your kidneys. Your doctor may have told you a percentage of your kidneys that are still functioning. Once the amount of your kidneys that are working is decreased beyond a certain level (not exactly clear how much and it varies by individual), 2 things happen:
- Kidneys are responsible for activating the Vitamin D in our body so it works. With less functional kidney, lower amounts of vitamin D3 are available in the bloodstream.
- Kidneys also excrete the phosphorus in our bodies, and with a lower capacity to produce urine, phosphorus builds up in the bloodstream.
Those two events that happen together bring about a decrease in serum (blood level) calcium. A decrease in the amount of calcium, plus a decrease in the amount of Vitamin D3 and an increase in the amount of phosphorus in the blood cause your body to think you need more PTH (because it needs to increase the amount of calcium in your bloodstream to a normal level).
It's essential to have regular check-ups with your doctor if you suffer from CKD or hyperparathyroidism so that potential complications can be identified early on. Keeping track of changes in symptoms and adjusting lifestyle accordingly will improve quality of life and help prevent long-term damage caused by this condition.
Importance of Diet in Managing Hyperparathyroidism and CKD
Taking control of your nutrition is essential in managing the symptoms of both chronic kidney disease and hyperparathyroidism, so don't ignore the importance of diet. Managing your dietary intake can help you to better manage your phosphorus levels (low phosphorus foods) and maintain an optimal lifestyle even with a chronic condition.
By following dietary guidelines and keeping track of what you eat, you can make sure you're getting all the essential nutrients while avoiding those that could aggravate your symptoms.
When it comes to managing hyperparathyroidism and CKD, there are some important dietary restrictions to take into consideration.
It's recommended to limit foods high in phosphorus such as dairy products, nuts, beans, lentils, dark-colored soft drinks and beers as well as processed foods like ready meals or fast food.
Additionally, high sodium intake should be avoided since it increases the risk of fluid retention which can worsen CKD-related health problems like swelling in legs or ankles.
Adopting a healthy lifestyle with a proper diet is key for symptom management when living with these two conditions. Making small changes such as reducing salt intake or limiting unhealthy snacks will help you get on top of your nutrition needs while managing hyperparathyroidism and CKD simultaneously.
Nutrients to Monitor in a Hyperparathyroidism and CKD Diet
Struggling with a chronic condition can be overwhelming, but monitoring your nutrient intake is an essential part of managing hyperparathyroidism and CKD.
To do this effectively, it's important to keep tabs on calcium supplementation, phosphorus control, vitamin D intake, protein sources, and sodium regulation.
- Levels of calcium should be monitored closely since it helps regulate the parathyroid hormone levels in those with hyperparathyroidism.
- Phosphorus control is another important factor to pay attention to when managing both conditions as it can cause complications if left unchecked. This means avoiding processed foods and high-phosphorus animal proteins like organ meats and shellfish.
- Vitamin D intake is also key since it helps reduce the risk of developing fractures due to bone loss caused by hyperparathyroidism or CKD-associated osteoporosis. For people who lack sufficient sunlight exposure, supplements may be necessary for adequate doses of vitamin D (Protein for CKD Patients by stage).
- Lastly, protein sources should be selected carefully as too much protein can worsen kidney disease symptoms such as fatigue and nausea while not enough can lead to muscle wasting in people with CKD. Individuals must keep an eye on their sodium intake as high amounts are often associated with increased blood pressure which exacerbates both diseases' symptoms in some cases.
It's not always easy to stay on top of managing a chronic condition like hyperparathyroidism or CKD but getting into the habit of monitoring one's nutrient intakes can help make life more manageable over time, even if small changes are made every day towards healthier eating habits that comply with these guidelines!
With guidance from healthcare providers and support from family & friends alike, anyone struggling with these ailments will soon find themselves equipped with the knowledge they need to manage their dietary requirements more effectively for greater overall health outcomes down the road!
Calcium and Phosphorus Balance in Hyperparathyroidism and CKD
Maintaining a healthy blood calcium levels and phosphorus balance is essential when managing hyperparathyroidism and CKD, so it's important to track your intake of these nutrients.
What does eGFR stand for in a blood test? When the estimated Glomerular Filtration Rate (eGFR) decreases to less than 60 ml/min, your ability to remove phosphorus from your blood via your kidneys becomes altered.
The part of your nephrons that are still working compensate by increasing the removal of phosphorus because your blood levels are increased. This helps to maintain normal phosphorus levels in your bloodstream.
Once you progress further in kidney disease, your nephrons eventually become unable to excrete enough phosphorus to compensate, and that is when you start to notice hyperphosphatemia (elevated levels of blood phosphorus).
So, as the amount of phosphorus increases in your blood, PTH is secreted to compensate. Calcium can bind with phosphorus (if they are out of balance) in the blood stream and form particles that then are deposited in organs and blood vessels.
As phosphorus levels increase, this risk is higher, so your body reacts by breaking down bones and increasing serum calcium level. This causes the bones to weaken over time, and calcium particles (those bound with phosphorus) to deposit in areas of the body such as the heart.
Dietary interventions are key to keeping your levels in check since some foods can interfere with phosphorus absorption or mineral deficiencies can cause an imbalance. If you're having trouble getting enough calcium through diet alone via intestinal calcium absorption, consider taking a supplement to help support bone health.
Making sure you get the right amount of both minerals is important for preventing complications associated with hyperparathyroidism and CKD.
It's essential that you monitor your calcium consumption and dietary phosphate intake on a daily basis. Understanding how much of each nutrient is in various food sources will help you create meals that promote balance between them. Pay attention to portion sizes as well, as too much of one nutrient can throw off the delicate equilibrium required for optimal health outcomes.
Consider talking to a nutritionist or medical professional who specializes in hyperparathyroidism and CKD diets if you need extra assistance creating meal plans tailored for your specific needs.
Knowing which supplements to take can be tricky, especially when dealing with two separate conditions at once. Speak with your doctor about any recommended products they suggest for maintaining balance of calcium and phosphorus levels, such as multivitamins or individual minerals like iron or magnesium.
They may also suggest switching up your existing medications if there could be possible interactions with other components within them causing an imbalance between these two nutrients (commonly prescribed medications for CKD).
Vitamin D and its Role in Hyperparathyroidism and CKD
You can't overlook the importance of Vitamin D for managing both hyperparathyroidism and CKD. It's essential for keeping your levels in check and improving your overall health. Without adequate levels, your body won't be able to properly absorb minerals like calcium and phosphorus, which are necessary for bone health.
PTH works to "normalize" your serum calcium concentrations or the amount of calcium available in your bloodstream. Calcium is used for many things in your body, and it needs to be available to your cells. So, an increased amount of PTH will cause your bones to be broken down more quickly to makes its calcium content available in your bloodstream.
Vitamin D3 happens to be very important in the actions and levels of PTH in our body. You may be aware that our bodies can "make" vitamin D by exposing our skin to sunlight for 10-20 minutes every day. That vitamin D our skin makes has to be transported to the kidney to be changed into the "active" form our body uses. It keeps us from overdosing on Vitamin D with too much sunlight.
Once vitamin D becomes activated, it can work in our bodies. It stimulates some other hormones that tell the parathyroid we have enough PTH. It also decreases PTH indirectly by increasing the amount of calcium we absorb in our "gut" through our gastrointestinal tract.
This increases the amount of calcium in our blood stream, and keeps the amount of PTH at a normal level. But once you have a decreased level of vitamin D in your body, it does not work to increase the level of calcium in your bloodstream as efficiently (you don't absorb as much) so your body starts increasing the amount of PTH to accommodate your calcium needs.
When it comes to treating hyperparathyroidism and CKD, Vitamin D supplementation is often recommended as part of dietary guidelines. Here are a few ways you can make sure you're getting enough:
- Spend more time outside in direct sunlight – UV rays from sunlight help form Vitamin D3.
- Incorporate foods rich in Vitamin D into your diet such as fatty fish (e.g., salmon), egg yolks, fortified milk products, certain mushrooms, and organ meats like liver.
- Take a supplement if needed – sometimes doctors will recommend a Vitamin D supplement if dietary sources aren't enough or if there's an underlying medical issue causing deficiencies.
It's easy to see why maintaining healthy levels of Vitamin D is so important when managing conditions like hyperparathyroidism and CKD. If you think you might be deficient or have any questions about how much you should be getting each day, talk to your doctor right away!
Management And Treatment of PTH and SHPT
KDOQI guidelines have recommended target ranges for PTH and calcium levels in renal patients with Stage 3 - 5 kidney disease. Based on those target ranges, the first course of action to improve the health of a patient with SHPT and suppress the levels of PTH is thought to be Vitamin D therapy.
As vitamin D plays such a role in our absorption of calcium, if a person can take in and absorb appropriate amounts of "active" vitamin D (doesn't have to be processed by the kidneys), their calcium absorption rate should also improve.
In addition to Vitamin D, dietary therapy includes reduction of high phosphate foods. Foods that are high in phosphate content include dairy products, meats, beans, dark sodas, beer and nuts. Many of these foods are great sources of protein, so it is important to be cautious when eliminating foods. You should focus on removing foods that are high in phosphate yet lower in protein, such as dark colas, cheese, milk, ice cream and beer.
You have to be careful about sources of protein because that can lead to malnutrition which affects outcomes once people start on dialysis. Also, dietary phosphate restriction may not be adequate since most of our food contains phosphates. Many doctors also recommend the use of phosphate binders as well.
Phosphate binding agents are taken with foods, up to 3-4 times per day, and attach to phosphate in the foods we eat causing it to remain in the digestive system and be excreted through stool.
They have to be taken with food or they don't work effectively, yet it is difficult for people to be consistent and remember to take the medications.
Sometimes doctors use several different types of binders to achieve success. Some phosphate binders can be found over the counter such as calcium carbonate and aluminum hydroxide. But, you should talk to your doctor about it prior to initiating any additional intake.
Protein Intake: A Key Consideration in Hyperparathyroidism and CKD
Managing your protein intake is essential for keeping hyperparathyroidism and CKD in check, so it's important to be mindful of how much you're consuming each day. To do this, it's important to understand the sources of dietary protein as well as the dietary guidelines that must be followed for hyperparathyroidism and CKD.
| Protein Sources | Dietary Guidelines |
| Lean meats, poultry, fish, eggs, dairy products, legumes, nuts/seeds | Limit saturated fat intake; Choose low-fat options; Avoid processed foods; Eat more fruits & vegetables; Incorporate nutritional supplements such as vitamin D & calcium into diet if needed |
When having hyperparathyroidism and CKD together, diet modifications are key. Making smart food choices while focusing on lean proteins is recommended in order to ensure proper nutrition.
In addition to dietary changes like limiting unhealthy fats and avoiding processed foods, adding nutritional supplements such as vitamin D or calcium can help maintain balance between healthy eating habits and necessary nutrients. Remember though that supplements should only be taken after consulting with a medical professional first.
Considering all these factors is vital when managing your protein intake while living with both hyperparathyroidism and CKD. Eating a balanced diet full of nutrient-rich proteins can help keep symptoms at bay while still providing enough energy throughout the day for everyday activities.
Sodium and Fluid Restrictions in Hyperparathyroidism and CKD Diet
When living with both hyperparathyroidism and CKD, it's essential to keep a watchful eye on sodium and fluid intake in order to maintain balanced levels. For those with kidney disease and hyperparathyroidism, the right balance of sodium is especially important as too much can cause fluid overload, while too little can lead to dehydration.
Keeping an eye on sodium sources such as table salt, processed foods (processed foods and CKD), and canned goods is key for maintaining proper sodium levels in the body. Additionally, keeping track of water consumption throughout the day is also necessary.
In addition to monitoring sodium intake for those with both hyperparathyroidism and CKD, making sure that there is enough potassium and magnesium in the diet is also important. Potassium helps regulate electrolyte balance in cells while magnesium helps activate enzymes related to energy production.
What Should I Do About My SHPT?
First of all, discuss what it means with your doctor. Develop that relationship so you can ask. If you cannot, consider finding another doctor who will work with you. If you need to make a longer appointment, you should tell the person booking the appointment that you have a lot of questions and request a longer appointment time. That will keep your physician from feeling rushed.
At this point - if you have CKD Stage 3, it is recommended that you work with a nephrologist. They are experts and will manage your kidney disease very well. You may also want to find a local dietitian or check into a meal plan that meets your nutritional needs.
Decreasing the amount of phosphate in your diet, in addition to treatment with an active vitamin D medication can provide a great deal of improvement and reduce your risk of bone and cardiac complications.
Creating a Balanced Diet Plan for Hyperparathyroidism and CKD
Creating a balanced diet plan for your hyperparathyroidism and CKD can be an important step in managing your health. With the right modifications to your habits, you can ensure that you are getting the nutrition you need while avoiding any potential complications.
It is important to make sure that you are following guidelines from both your healthcare team and dietician when creating this plan. A wide variety of food should be included in order to ensure that all of your nutritional needs are being met.
| Food Groups | Foods to Include |
| Fruits & Vegetables | Apples, Bananas, Carrots, Spinach |
| Grains & Starch | Breads, Rice, Potatoes, Oatmeal |
| Protein Foods | Chicken Breast, Fish Fillet, Eggs, Legumes |
| Dairy Products | Milk, Yogurt Cheese cubes/slices/shredded |
It is important to keep track of what foods you eat and drink throughout the day so that you can make sure that all food groups as listed above are covered. You may also want to take into account portion sizes (portion control for CKD patients) as well as how often each type of food is consumed in order to have a more balanced diet overall.
By making small changes over time and following these dietary guidelines it will become easier for you to create healthy eating patterns and maintain them long term.
Lifestyle Changes to Support a Hyperparathyroidism and CKD Diet
Taking charge of your lifestyle can help you manage hyperparathyroidism and CKD, so it's important to make small changes that support a balanced diet. The good news is there are many ways to do this without feeling overwhelmed or deprived.
Tracking food intake, making dietary adjustments, and incorporating lifestyle changes are all effective tools for managing the condition. Food tracking involves keeping a record of what you eat as well as the quantity and quality of nutrients consumed daily.
This helps you gain insight into your eating habits, identify areas where improvements can be made, and monitor how foods affect your symptoms. Additionally, tracking kidney function with lab tests such as creatinine levels will help gauge diet compliance over time.
Making dietary adjustments may also improve overall health in those with hyperparathyroidism and CKD by promoting nutrient balance from whole foods rather than relying solely on supplements.
Eating anti-inflammatory foods like fruits, vegetables, legumes, and fish; avoiding processed foods; maintaining adequate hydration; and limiting salt intake could all help reduce symptoms associated with the condition while supporting kidney function.
Small lifestyle changes such as reducing stress levels through yoga or meditation can also benefit overall health by improving emotional wellbeing, which may directly impact physical health outcomes over time.
Monitoring and Adapting Your Diet Over Time with Hyperparathyroidism and CKD
Monitoring and adapting your diet over time is crucial when managing hyperparathyroidism in renal patients. When dealing with hyperparathyroidism and CKD, it is important to limit certain nutrients in your diet. Phosphorus, for example, needs to be restricted as impaired kidney function can lead to its buildup in the bloodstream.
Foods high in phosphorus, such as dairy products, legumes, and processed foods, should be limited or avoided. Calcium intake should also be monitored. Choosing calcium-rich foods with low phosphorus content, like leafy greens, is beneficial. However, caution on potassium intake must be kept in mind when consuming green leafy vegetables.
Moreover, monitoring protein intake is crucial for individuals with CKD. Restricting protein can help reduce the burden on the kidneys and manage uremic symptoms. High-quality protein sources, such as lean meats, fish, and poultry, should be consumed in moderation. Additionally, sodium intake should be limited to control blood pressure and fluid balance.
Vitamin D plays a vital role in calcium metabolism, but individuals with hyperparathyroidism and CKD often have vitamin D deficiencies. Supplementation may be necessary under the guidance of a healthcare professional.
Regular monitoring of blood levels is essential to assess the effectiveness of dietary modifications. Blood tests can evaluate calcium, phosphorus, parathyroid hormone, and other relevant parameters. Collaborating with a registered dietitian who specializes in renal nutrition can provide valuable guidance in managing your diet effectively.
As the conditions progress, dietary adjustments may be needed. Personalized dietary plans may involve more restrictive phosphorus and protein limits, depending on the severity of kidney dysfunction and parathyroid hormone levels. Adapting to these changes is crucial to maintain the best possible nutritional status and prevent complications.
FAQs for Secondary Hyperparathyroidism
Hyperparathyroidism in the presence of chronic kidney disease (CKD) can lead to various potential complications. Firstly, hyperparathyroidism can cause an imbalance in calcium and phosphorus levels, leading to the development of mineral and bone disorders (egfr blood test).
High levels of parathyroid hormone can cause the bones to release calcium, leading to decreased mineral bone density, weakened bones and an increased risk of fractures. Excessive phosphorus levels can also contribute to bone mineral loss.
Additionally, hyperparathyroidism with CKD can exacerbate cardiovascular complications. Elevated parathyroid hormone levels are associated with increased vascular calcification, which can lead to cardiovascular disease, including heart attacks and strokes.
Furthermore, hyperparathyroidism can impact kidney function. The overproduction of parathyroid hormone can contribute to the progression of CKD, leading to further decline in kidney function.Other complications may include muscle weakness, fatigue, joint pain, and impaired immune function.
It is important for individuals with hyperparathyroidism and CKD to work closely with their healthcare team to manage and monitor these potential complications, through medication, dietary modifications, and other appropriate interventions. Regular check-ups, blood tests, and imaging studies are often necessary to assess the progression of the conditions and to identify and address any complications that may arise.
If you've been diagnosed with hyperparathyroidism and chronic kidney disease (CKD), your doctor may recommend a specific diet to manage your condition. How long to follow the diet depends on individual factors, but it's important to maintain compliance for as long as possible.
This means making attitude changes, managing stress healthily, and adjusting your lifestyle to get the right minerals from food. By following your doctor's recommended diet with dedication and ongoing symptom monitoring, you can improve your quality of life with both conditions.
When following a diet for hyperparathyroidism and chronic kidney disease (CKD), there are several foods that are generally recommended to be avoided or limited. These include:
. High-phosphorus foods: Dairy products, legumes, nuts, seeds, processed meats, and carbonated beverages should be restricted as they are rich in phosphorus, which can accumulate in the blood.
. High-calcium foods with high phosphorus content: Foods like milk, cheese, and yogurt are high in both calcium and phosphorus, so they should be consumed in moderation.
. Sodium-rich foods: Processed and packaged foods, fast food, canned soups, and salty snacks should be limited to control fluid balance and blood pressure.
. Potassium-rich foods (if necessary): Some individuals with advanced CKD may need to restrict potassium. Examples of high-potassium foods include bananas, oranges, potatoes, tomatoes, and certain vegetables.
. Foods high in oxalates (if necessary): Oxalates can contribute to the formation of kidney stones. Spinach, rhubarb, beets, nuts, and chocolate are examples of high-oxalate foods that may need to be limited.
Remember that individual dietary recommendations may vary based on the severity of CKD and other factors. It's crucial to consult with a registered dietitian who specializes in renal nutrition to create a personalized diet plan tailored to your specific needs.
It is generally advisable to limit or avoid alcohol consumption when following a diet for hyperparathyroidism and chronic kidney disease (CKD). Alcohol can have negative effects on kidney function and can interfere with the body's ability to maintain proper mineral and fluid balance.
Alcohol can also interact with medications that may be prescribed for managing hyperparathyroidism or CKD, potentially causing adverse effects or reducing their effectiveness. Furthermore, alcohol can contribute to dehydration and high blood pressure, which are concerns for individuals with CKD.
However, it is important to consult with your healthcare provider or a registered dietitian to determine if moderate alcohol consumption may be acceptable for your specific situation. They can provide personalized guidance based on the severity of your condition, overall health, and any other medications or treatments you are undergoing. It is crucial to prioritize your kidney health and follow the recommendations provided by your healthcare team.
Kidney transplantation can have a positive impact on secondary hyperparathyroidism, but it may not completely cure the condition in all cases. SHPT often develops as a result of end stage renal disease and the associated disturbances in levels of calcium, phosphorus, and vitamin D mineral metabolism.
Kidney transplantation can restore kidney function, leading to improved regulation of these metabolic processes. As a result, many individuals experience a reduction in parathyroid hormone levels after transplantation. However, some individuals may still require ongoing monitoring and management of SHPT, even after kidney transplantation. Some patients even develop tertiary hyperparathyroidism after transplant, which can be even more challenging.
Factors such as the severity of SHPT prior to transplantation, the health of the transplanted kidney, and individual variations in response to the transplant can influence the outcomes. Close follow-up with healthcare providers, including nephrologists and endocrinologists, is necessary to monitor and manage SHPT post-transplantation and ensure optimal outcomes.
Diet Is Key In Managing Hyperparathyroidism
In conclusion, managing hyperparathyroidism and chronic kidney disease (CKD) requires careful attention to diet and lifestyle choices.
Dietary restrictions, such as limiting foods high in calcium, phosphorus, and sodium, can help alleviate symptoms associated with these conditions. Monitoring nutrient intake, including calcium, phosphorus, vitamin D, protein, sodium, potassium, and magnesium, is crucial for maintaining overall health (progression of symptoms for CKD).
Adopting a diet rich in anti-inflammatory foods, such as fruits, vegetables, legumes, and fish, can improve well-being. It is important to understand the connection between hyperparathyroidism and CKD and how they interact.
Regular check-ups, emotional support, and professional guidance are essential for effective management. By taking control of nutrition, monitoring nutrient intake, and balancing calcium and phosphorus levels, individuals can better manage their conditions and improve their quality of life.