Facts About Chronic Kidney Disease
Chronic Kidney Disease (CKD) is a silent killer affecting millions of people in the United States.
For people with CKD, it's crucial to understand its links to cardiovascular disease and diabetes, how diet can slow its progression (ckd progression), and the role of medication.
In this article, we'll delve into these topics, explore its impact on heart and bone health, and discuss the risks associated with dialysis.
Let's arm ourselves with knowledge to better manage this challenging condition.

Jump to:
- Key Takeaways
- Understanding Chronic Kidney Disease and Its Prevalence
- The Link Between Chronic Kidney Disease and Metabolic Syndrome
- The Possibility of Delaying or Slowing Down Chronic Kidney Disease
- The Importance of Diet in Managing Chronic Kidney Disease
- The Uncommon Knowledge About Chronic Kidney Disease
- The Role of Blood Urea Nitrogen (BUN) in Chronic Kidney Disease
- The Role of Hydration in Chronic Kidney Disease Management
- Understanding the Connection Between Chronic Kidney Disease and Anemia
- The Impact of Chronic Kidney Disease on Mental Health
- The Importance of Exercise in Chronic Kidney Disease Management
- How Chronic Kidney Disease Affects Sleep Quality
- The Role of Medication in Managing Chronic Kidney Disease
- Lifestyle Adaptations Strategies
- The Connection Between Chronic Kidney Disease and Bone Health
- Understanding the Risks of Dialysis in Chronic Kidney Disease
- Diet Is Most Important
Key Takeaways
- Chronic kidney disease affects a significant number of people in the United States, with over 37 million cases.
- One in three people are at risk of developing kidney disease, and many individuals have the disease without even realizing it.
- Kidney disease is a metabolic disorder that is closely linked to other chronic illnesses such as heart disease and diabetes.
- There are five stages of kidney disease, and while there is no cure, the progression can be slowed through proper management, including dietary changes.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding Chronic Kidney Disease and Its Prevalence
Chronic kidney disease (CKD) is a serious health issue affecting millions of people in the United States alone.
It's alarming to realize that one in three people are at risk of developing this metabolic disorder, and many are living with it unknowingly.
Grasping the progression of this illness is crucial; it moves through five stages - from presenting virtually no symptoms to chronic kidney failure - and understanding each stage can help manage its impact effectively (signs and symptoms of kidney failure).

Prevalence of Kidney Disease
You're not alone if you've been diagnosed with CKD. CKD is a common condition with over 37 million people in the United States dealing with this disease. Understanding the risk factors is vital for early detection and to slow its progression.
The effects of CKD on one's life can be substantial. It demands a wide range of lifestyle changes if the progression of the illness is to be slowed or reversed, and the implications can extend far beyond physical health.
From financial costs associated with treatments to emotional impacts such as depression, living with CKD can take its toll.
Understanding Kidney Disease Progression
Let's dive into understanding how kidney-related health issues progress over time. CKD isn't a stand-alone condition; it's part of a chain reaction. One disorder can trigger another, creating a domino effect that can impact overall health. Understanding disease progression is crucial for effective management.
Here's a snapshot of what we can do to prevent:
- Early Detection: Regular screening can help detect kidney disease in its earlier stages.
- Lifestyle Modifications: A balanced diet and regular exercise contribute greatly to kidney disease management.
- Treatment Options: These range from dietary changes to medications, dialysis, or even a kidney transplant.
- Patient Education: Awareness about symptoms, risk factors, and healthy lifestyle choices can make a difference.
Managing the disease through diet plays an essential role in slowing down its advancement. Dietary modifications can either delay or expedite its course, further emphasizing the importance of guided nutritional advice.
Another key aspect to consider is the impact of anemia, often associated with CKD, which needs careful monitoring and management. Regular exercise also holds significance in maintaining overall wellness.
Medication management becomes vital as conditions like high blood pressure and bone weakness could be linked to kidney disease progression.
Remember, healthcare isn't just about treatment but also education and prevention!
The Link Between Chronic Kidney Disease and Metabolic Syndrome
CKD and metabolic syndrome often go hand in hand, creating a complex and challenging health issue for those affected. Metabolic syndrome refer to a range of conditions that affect the body's metabolism, including diabetes, obesity, and high blood pressure.
These disorders can have a significant impact on kidney health and function, leading to the development or progression of CKD. Understanding the link between these two conditions is crucial for both prevention and management.
Diabetes and Chronic Kidney Disease
One of the primary factors linking CKD and the metabolic syndrome is insulin resistance. Insulin is a hormone produced by the pancreas that regulates blood sugar levels. In metabolic syndrome, the body becomes less responsive to the effects of insulin, resulting in elevated blood sugar levels.
Over time, this can cause damage to the blood vessels and the filtering units inside the kidneys. This impairs the ability of the kidneys to process waste as they should. As a result, waste products build up in the body and can lead to complications such as proteinuria (the presence of excess protein in the urine), hypertension (high blood pressure), which causes a further progression of kidney disease.
Hypertension and Chronic Kidney Disease
Hypertension is both a cause and a consequence of CKD. High blood pressure can cause blood vessels in the kidneys to weaken, impairing their ability to filter waste products effectively. On the other hand, CKD can contribute to the development or worsening of hypertension as diseased kidneys are unable to regulate blood pressure as they should.
Obesity and Chronic Kidney Disease
Obesity, another component of metabolic syndrome, also promotes the development of CKD. Excess weight and body fat can lead to the development of conditions like hypertension and diabetes, which are major risk factors for CKD. Additionally, obesity itself can directly contribute to kidney damage by causing inflammation and oxidative stress.
The link between CKD and metabolic disorders is undeniable. Understanding this connection and implementing preventive measures and lifestyle modifications can help reduce the risk of developing CKD or slow down its progression (progression of symptoms for CKD). By addressing metabolic disorders and maintaining overall health, individuals can take proactive steps towards preventing impairment of kidney function and maintaining healthy kidneys.
Chronic Kidney Disease Management
Managing the link between CKD and metabolic syndrome requires a multifaceted approach. Lifestyle modifications, such as adopting a healthy diet and engaging in regular physical activity, are crucial in preventing and managing both conditions.
A diet rich in fruits, vegetables, whole grains, and lean proteins can have many benefits for kidney patients, which include helping control blood levels of sugar, reducing inflammation, and promoting overall kidney health.
Additionally, maintaining a healthy weight is essential in preventing the progression of both metabolic syndrome and CKD. Weight loss, achieved through a combination of dietary changes and increased physical activity, can improve insulin sensitivity and reduce the strain on the kidneys.
Hydration management is another important aspect of CKD care. While it's essential to stay hydrated, overhydration can strain the kidneys further. Therefore, it's a careful balance one must strike.
Medications are also an important part of CKD management. The type and dosage of medications used to treat metabolic disorders and CKD may vary depending on the individual's condition. Some of the medications that may be prescribed by your healthcare provider include anti-hypertensives, anti-diabetics, statins, and phosphate binders.
Remember, early intervention and comprehensive management strategies can significantly improve your quality of life despite this diagnosis.
The Possibility of Delaying or Slowing Down Chronic Kidney Disease
While CKD is a progressive condition, there are several strategies that can help slow down its progression and preserve normal kidney function.
It's not just about medication, though they are effective in managing symptoms and complications. But adopting a healthier lifestyle, proper diet, regular exercise, stress management, can make a huge difference in overall health and well-being.
Lifestyle Modifications Impact
Lifestyle modifications can significantly impact the progression of CKD, especially when combined with proper dietary changes. The dietary impact on this metabolic disorder cannot be overstated. Consuming a low-salt diet, along with limiting potassium and phosphorus intake, can effectively slow down kidney damage.
Don't overlook hydration's role either; maintaining an adequate fluid intake is key to keeping kidneys functioning well. Besides diet, mental health plays a crucial part too. Stress management techniques such as meditation or yoga can help reduce high blood pressure, one of the leading causes of kidney disease.
Lastly, the benefits of regular exercise cannot be understated. It helps control blood sugar levels, reduces weight, and keeps your heart healthy - all critical in managing kidney disease. Remember: small lifestyle changes make big differences!
The Importance of Diet in Managing Chronic Kidney Disease
For people living with CKD, it's important to understand the paramount role of diet in managing this condition.
The impact of what we ingest cannot be overstated; it has the potential to either exacerbate or significantly slow down ckd progression.
Navigating through nutrition management options can be complex, but it's a crucial aspect that offers a measure of control and hope in an otherwise irreversible condition.
Dietary Impact on Chronic Kidney Disease
You're going to find that your diet plays a pivotal role in managing CKD, potentially slowing its progression or halting it altogether.
- Nutritional guidelines: An informed approach to dietary changes can make a world of difference. Understanding and following nutritional guidelines is crucial; they're not just suggestions but lifelines.
- Importance of protein intake: Managing protein consumption is vital as excess protein can burden the kidneys, yet too little may cause malnutrition.
- Role of sodium restriction: Restricting sodium is a key step in controlling blood pressure levels, thus reducing strain on your kidneys.
In serving others, let's spread awareness about the significant impact our diet choices have on CKD management (CKD Diet plan).
Role of Dietitians
If you have kidney disease, you should work closely with dietitians specializing to develop individualized nutrition plans that help slow the progression of CKD, manage complications, and improve overall health and quality of life.
Here are some key roles of dietitians in managing CKD patients:
- Assess nutritional needs, including dietary intake, body composition, and lab values.
- Develop personalized meal plans considering CKD stage, kidney function, and medical conditions.
- Control protein intake, guiding patients on sources and portion sizes.
- Manage fluid and electrolyte balance, educating patients on sodium, potassium, and phosphorus sources.
- Monitor micronutrient intake and address deficiencies through supplements or dietary modifications.
- Educate patients on CKD, dietary restrictions, and adherence to meal plans.
- Collaborate with healthcare team for comprehensive care and adjust nutrition plans as needed.
Overall, dietitians can be instrumental in helping you manage your renal diet and nutritional needs. Their expertise in renal nutrition plays a crucial role in the overall management and well-being of individuals with kidney disease.
The Uncommon Knowledge About Chronic Kidney Disease
People are often unaware of the unexpected risk factors that contribute to CKD, apart from the commonly known culprits like diabetes and high blood pressure.
Many people still believe that medication (diet vs medication for CKD improvement) is the only solution when in fact, dietary changes can be transformative.
It is crucial to delve into these lesser-known aspects of kidney disease to equip yourself with vital knowledge that can help you manage this debilitating condition more effectively.
Unexpected Risk Factors
Besides the commonly known risk factors, there are unexpected ones that can increase your chances of developing CKD. Unusual causes such as prolonged exposure to certain environmental factors, like heavy metals, can inadvertently damage your kidneys.
Additionally, long-term use of some medications, such as non-steroidal anti-inflammation drugs, may interact negatively with your renal system.
A genetic predisposition also plays a significant role. If you have family history of kidney disease, you're unfortunately at higher risk of kidney disease. This doesn't mean it's a certainty, but rather something to be mindful of and discuss with medical professionals.
Lastly, occupational hazards are often overlooked. Some jobs involving agricultural production can put you under increased risk of developing CKD. Awareness and prevention are key in these situations for reducing risks.
Treatment Misconceptions
It's disheartening to witness how misinformation can lead patients astray.
- Misunderstanding about medication effectiveness: Some might believe that medications can reverse the damage, which unfortunately isn't true.
- Alternative therapies misconception: Others may turn to unproven alternatives hoping for a miracle cure. It's essential to understand that while some therapies may help manage symptoms, they won't reverse kidney damage.
- Overlooking lifestyle modifications: This is perhaps the most common misconception. Diet and lifestyle changes are often undervalued in their potential impact.
Understanding the correct information about your kidney health is critical for reducing your risk and managing your condition. Being aware of unexpected risk factors, as well as treatment misconceptions, can be life-changing.
The Role of Blood Urea Nitrogen (BUN) in Chronic Kidney Disease
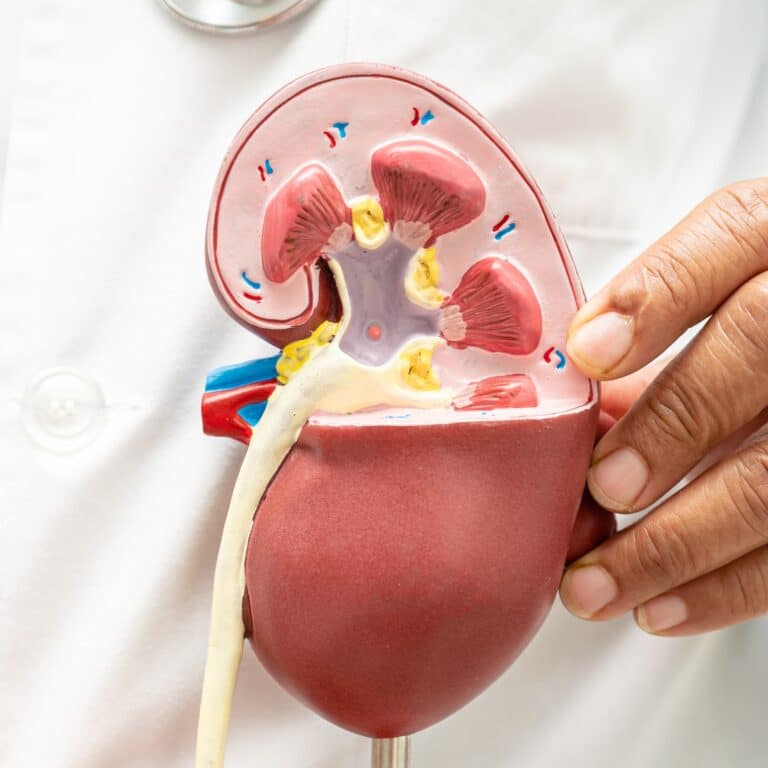
As we delve into CKD, it's crucial to understand the role of blood urea nitrogen (BUN) in this condition. BUN levels are a key indicator of kidney function, and as such, they become particularly important when dealing with CKD.
We'll also be exploring how BUN (how to improve bun level) can be regulated in CKD patients, providing valuable insight into managing this complex metabolic disorder.
BUN Levels and Chronic Kidney Disease
BUN (how to improve bun level) is a waste product that is produced when the body breaks down protein that. Normally, the kidneys filter wastes like urea nitrogen and excrete it in the urine. However, when kidney function is impaired, BUN levels can rise, which is why it's measured when assessing kidney function.
However, it's important to note that BUN levels can be influenced by factors other than kidney function, such as diet, hydration status, and certain medications.
To get a more accurate assessment of kidney function, other blood tests, such as serum level of creatinine and glomerular filtration rate (GFR) may be used along with BUN. These tests provide a more comprehensive picture of kidney function.
The Role of Hydration in Chronic Kidney Disease Management
As we delve further into understanding CKD, it's crucial to acknowledge the role hydration plays in managing this condition.
It's well-known that proper hydration has a profound impact on our kidneys, helping them flush out toxins and maintain balance in our bodies.
However, what isn't as widely discussed are the specific water intake guidelines for those with kidney disease - an element that could greatly influence the progression of this illness (fluids to hydrate with kidney disease).
Hydration's Impact on Kidneys
Proper hydration is crucial in managing kidney disease as it helps the kidneys clear toxins from the body effectively. Understanding fluid intake recommendations and adhering to hydration guidelines can make a significant difference in maintaining good kidney health. Thus, the importance of staying hydrated cannot be overstated for those with CKD.
However, managing fluid intake isn't just about drinking more water, it can also be about avoiding extra fluid intake. The impact of water overload on can be quite severe, as it can cause swelling and even difficulty breathing.
Water Intake Guidelines
It's crucial to understand the guidelines for water intake when managing a metabolic disorder like kidney disease. The importance of staying hydrated cannot be stressed enough, as proper fluid intake aids in preventing dehydration and preventing loss of kidney function over time (ckd diet guidelines).
Here are hydration guidelines according to your stage of kidney disease:
| Stage | Water Consumption Recommendations | Notes |
| Stages 1-2 | 64 ounces of fluids/day | Maintain adequate hydration |
| Stages 3-5 (not on dialysis) | Between 64 and 32 ounces of fluids/day | Restrict your fluid intake |
| Dialysis | 32 ounces of fluids/day | Further restrict fluids |
These fluid intake recommendations may vary depending on other health factors. It's always best to consult your healthcare provider about your specific situation. Remember, good water consumption habits can significantly help manage kidney disease progression.
Understanding the Connection Between Chronic Kidney Disease and Anemia
As we delve deeper into the complexities of CKD, it's crucial to understand its connection with anemia.
Addressing and treating anemia in patients with kidney disease is critical to manage their overall health and slow down the deterioration of renal functions.
Kidney Disease's Impact on Anemia
Kidney disease can have a significant impact on anemia. Anemia is a condition characterized by a low level of red blood cells or hemoglobin in the blood, which reduces the blood's ability to carry oxygen to the body's tissues.
The kidneys play a crucial role in the production of erythropoietin, a hormone responsible for stimulating the production of red blood cells in the bone marrow.
In individuals with kidney disease, the kidneys' ability to produce erythropoietin is impaired. This leads to decreased production of red blood cells, resulting in anemia.
Anemia is also more common in the following groups: females, African-Americans, diabetic people, and people with advanced stages of kidney disease (stages 3-5).
Anemia can cause many symptoms, such as :
- Fatigue
- Poor appetite
- Paleness
- Insomnia
- Headaches
- Dizziness
- Shortness of breath
Kidney disease can have a profound impact on anemia due to the impaired production of erythropoietin and subsequent reduction in red blood cell production. Regular checkups and collaboration with healthcare professionals are essential to effectively address anemia (anemia and dialysis) and minimize its impact on the overall well-being of people with kidney disease.
Treating Anemia in Chronic Kidney Disease
Dealing with anemia when you've got CKD can feel overwhelming, but there are various treatment options available that can help manage both conditions. Let's break down the main ones:
- Iron Supplementation: Iron is essential for red blood cell production. If you're deficient, your doctor may recommend iron supplements.
- Erythropoiesis Stimulating Agents: These medications stimulate your bone marrow to produce more red blood cells, which can alleviate anemia symptoms.
- Blood Transfusions: In severe cases, this might be a necessary step to increase your red blood cell count quickly.
- Nutritional Interventions: Eating a balanced diet rich in iron and other essential nutrients can have a positive effect on your health.
Remember, managing underlying causes of CKD like diabetes or hypertension is also crucial in treating anemia in CKD effectively.
The Impact of Chronic Kidney Disease on Mental Health
Living with CKD can take a toll on your mental health. It's not uncommon for CKD patients to grapple with depression, a debilitating condition that can further exacerbate their physical symptoms and overall quality of life.
Additionally, the constant worry about kidney function, treatment options, and potential complications often leads to heightened levels of anxiety. It's a tough battle on multiple fronts
Depression in Chronic Kidney Disease Patients
It's not uncommon for patients with CKD to experience depression, given the physical and emotional toll this illness can take. The prevalence of depression among CKD patients is 3-4 times higher when compared with the general population.
The co-existence of these health conditions emphasizes the need for comprehensive mental health support in managing both illnesses. Psychological interventions play a critical role in depression management among CKD patients. Effective coping strategies are key elements that can greatly enhance their emotional well-being.
It's therefore crucial for healthcare providers to offer guidance and resources that go beyond physical health. This includes fostering an environment where mental health is prioritized, so patients feel comfortable seeking help.
In doing so, we can mitigate the impact of depression on CKD patients' lives, ultimately improving their quality of life.
Anxiety and Kidney Disease
Depression isn't the only mental health issue that can burden those with CKD. Anxiety, too, is frequently part of the symptoms of kidney disease. Studies have shown that the prevalence of anxiety is 2 times higher in patients with CKD.
It's crucial to adopt coping strategies like mindfulness or cognitive behavioral therapy; these therapy options have been proven effective in easing anxiety symptoms. Relaxation techniques such as deep breathing exercises or meditation also play a significant role in mitigating stress.
Remember, dealing with CKD isn't just about physical health (exercise for healthy heart), it's equally important to address your emotional well being along this journey.
The Importance of Exercise in Chronic Kidney Disease Management
Engaging in consistent exercise offers numerous benefits for CKD patients, including improved cardiovascular health, better blood pressure control (grilling blood pressure), and an overall boost to their well-being.
However, it's crucial to understand how to properly implement this routine into your daily life without causing undue strain or harm.
Exercise Benefits for Chronic Kidney Disease
Regular physical activity can significantly benefit individuals with CKD. It has the potential to slow the progression of the illness and improve overall health.
One of the key exercise benefits for CKD is that it boosts kidney function and enhances overall well being. Specific exercise recommendations for CKD patients may vary based on their condition's stage and severity. However, most forms of physical activity for CKD can be advantageous.
Regular exercise strengthens heart muscles, improves circulation, and manages blood pressure, all helpful in maintaining kidney health. Exercise also aids in controlling body weight, which can help control progression. Thus, integrating a suitable workout regimen is an essential part of managing this metabolic disorder effectively.
Implementing Regular Physical Activity
It's crucial to weave regular physical activity into your daily routine when you're managing a metabolic disorder like kidney disease. The benefits of exercise extend beyond just the physical. Exercise contributes significantly to your mental well being, by improving your mood, helping you relax, and reducing symptoms of depression and anxiety.
Physical activity recommendations for kidney patients often include continuous activities such as walking, swimming, and bicycling. The National Kidney Foundation recommends exercising at least three days a week on alternate days. Each exercise session should ideally last around 30 minutes.
Strategies for incorporating physical activity into your routine need not be overly complex or strenuous. Simple steps like taking short walks during breaks at work can make a significant difference in managing your condition and slow progression.
How Chronic Kidney Disease Affects Sleep Quality
Insomnia is common in CKD, and it can be quite a struggle. CKD impacts the production of melatonin, the hormone responsible for regulating sleep-wake cycles, which complicates our sleep patterns.
Sleep Disorders in Chronic Kidney Disease
You're likely to experience sleep disorders if you're dealing with CKD, which can further complicate your health situation. The impact of sleep on CKD is significant; poor quality rest can exacerbate the condition due to stress and fatigue. Insomnia is particularly common in CKD patients, causing a vicious cycle of worsening health.
Focus on sleep disorders management becomes crucial for maintaining overall well-being. Working closely with your healthcare provider to understand and follow recommended sleep hygiene tips can make a world of difference. These may include establishing regular bedtime routines, creating a conducive environment for sleep, and addressing issues like anxiety that often accompany insomnia.
Remember, improving your sleep quality isn't just about feeling rested, it can also be part of managing your kidney disease effectively.
The Role of Medication in Managing Chronic Kidney Disease
As we delve into the complex world of managing CKD, it's crucial to consider the role medication plays in this process.
We'll explore not only the common types of medications commonly used and their functions, but also tips on how to manage potential side effects that may arise from these treatments (diet vs medication for CKD improvement).
Medication Types and Functions
In managing your CKD, you'll likely encounter various types of medications, each with specific functions aimed at slowing the progression of the illness. Medication types include blood pressure drugs to manage hypertension, diabetes medications to lower blood sugar, to phosphate binders aimed at controlling dangerous levels of phosphorus in your body. Each medication type serves a crucial role and is effective in its own way.
However, like any treatment plan, it's essential to understand their functions and potential side effects. Some medications can cause dry mouth or fatigue, while others may lead to loss of appetite or changes in skin color. It's all part of medication management, knowing what each pill does and how it affects your body is key to living healthy lives.
Remember that proper medication effectiveness relies on adherence to prescribed dosage and frequency. Always consult your doctor for any concerns about side effects or effectiveness.
Medication Side Effects Management
You might experience various side effects from your medications, but there are ways to effectively manage them.
Always inform your healthcare provider of all the medications and supplements you're taking to avoid harmful interactions.
If the side effects become too severe, discuss alternative treatments with your doctor that might have lesser side effects.
Remember, effective medication management is key in treating CKD.
Lifestyle Adaptations Strategies
Now, let's delve into some crucial lifestyle adaptation tips essential for someone living with CKD. Coping mechanisms are key; they help us navigate the challenges and changes that accompany this illness.
Having a steady support system is invaluable, not only for practical assistance but also for emotional well-being. It's okay to lean on family, friends, or dedicated support groups during this time.
Stress management techniques such as meditation, deep breathing exercises, or gentle yoga can be beneficial in promoting relaxation and better health outcomes.
Prioritizing self-care practices - getting enough sleep, eating well-balanced meals, and taking time for leisure activities, must not be overlooked either. Remember, looking after your mental health is just as important as managing your physical symptoms.
The Connection Between Chronic Kidney Disease and Bone Health
CKD can significantly impact the strength and structure of bones, leading to disorders such as renal osteodystrophy, a condition that causes weak bones.
However, preventative measures can be taken to manage and mitigate these risks, which emphasizes the importance of early detection and proactive care for maintaining bone health while battling this chronic illness (chronic illness and CKD).
Preventing Bone Disorders in CKD
It's absolutely vital to address the risk of bone disorders when managing CKD.
The first step involves maintaining the balance of calcium and phosphorus, as it's crucial for bone health. In CKD, the kidneys may have difficulty regulating these levels. Your healthcare provider may recommend dietary changes, phosphate binders, and medications to help control calcium and phosphorus levels.
Vitamin D helps with the absorption of calcium and phosphorus in the body. In CKD, deterioration in kidney function can lead to vitamin D deficiency. Supplementation with active forms of vitamin D or vitamin D analogs may be prescribed to maintain adequate levels.
Regular weight-bearing exercises, such as walking or resistance training, may promote bone health. Consult with your healthcare provider or a physical therapist to develop an exercise plan suitable for your condition.
By prioritizing these strategies in our care plans, we can significantly improve the quality of life for people with kidney disease and aid their journey towards better overall health.
Understanding the Risks of Dialysis in Chronic Kidney Disease
As we delve into the complexities of chronic renal disease, it's crucial to understand the risks associated with regular dialysis treatment, a common treatment option for end-stage kidney disease (avoid end stage renal disease).
While dialysis serves as a lifeline, preserving life and health when kidneys no longer function properly, it's not without its complications.
It is our responsibility to educate ourselves about these potential issues and actively seek ways to prevent any negative outcomes from arising during our journey with this metabolic disorder.
Dialysis Risk Factors
Patients with advanced stages of kidney disease often need dialysis. However, this treatment comes with its own set of risks.
While there are no ideal dialysis alternatives with no risks yet, research continues in hopes of finding less invasive options.
As for now, adhering to a strict dialysis diet can significantly mitigate some side effects while prolonging life expectancy. This includes limiting excess fluid intake and controlling the consumption of certain nutrients like potassium and phosphorus.
Understanding all available dialysis treatment options is key to making an informed decision that best serves your health needs (why do you need a pre-dialysis diet plan?)
Preventing Dialysis Complications
Dialysis complications can range from anemia to low blood pressure, heart disease, and other cardiovascular complications. It's a tough journey, but being informed about these potential issues can help manage the process better.
You're likely wondering how to best prevent complications that can arise from dialysis. Let's explore some effective strategies.
First off, preventing infection is crucial. This means not only maintaining cleanliness at the site of your dialysis access but also staying up-to-date on vaccinations.
Managing fluid intake (fluid restricted diet menu) is another important aspect. Too much fluid can strain your kidneys and cause other issues, so monitoring your intake is key. Adhering to dietary restrictions also plays a significant role in managing kidney disease and minimizing complications from dialysis.
Don't overlook the importance of medication adherence. Taking prescribed medications correctly helps keep everything in balance.
Lastly, mental health support should not be discounted. Chronic diseases can take a toll emotionally and mentally, so seeking help when needed is essential for overall well-being.
Diet Is Most Important
Chronic kidney disease is not as uncommon as many people think it is. An estimated 37 million people in the United States alone have chronic kidney disease and roughly 1 in 3 people are at risk for developing it.
There is no cure for chronic kidney disease and damage to your kidneys can not be reversed. You can, however, slow the progression of chronic kidney disease through proper management, especially dietary restrictions.
Although there are many factors in the treatment of chronic kidney disease that are all important, diet is perhaps the most important. This is because it is your diet that can either progress or delay your illness. The right dietary changes can slow, or potentially even halt, the progression of chronic kidney disease.
These are all lesser known, but very important, facts about chronic kidney disease. Use this information to start a conversation with your healthcare provider about how you can treat your disease. This conversation could help you avoid end-stage kidney failure and help you live a healthier and more comfortable life.
It Shouldn’t Be This Hard to Understand What To Eat…
Sign up and you’ll get instant access to a free 7 day meal plan designed specifically for your a person with Pre-Dialysis Kidney Disease










I am always glad to find information on Kidney Disease .
Thank you.
I am a patient. I have chronic Kidney Disease Stage 3. My doctor has not recommended a diet or much of anything else. All he has me do is take once a year.
My primary doctor does the same thing. I am not sure if I should be on a renal diet or not.Neither one of my doctors seem to care much either way.
I take Medicine for my High Blood Pressure and Hypo-thyroidism. My youngest son had a Kidney transplant 2 years ago. He had hardening of the arteries in his kidneys.
My Mom had Heart Failure and Kidney Disease She passed away 20 yrs ago from a combination of both.Where I live there isn't any local doctors that are kidney doctors. I have to travel 100 miles just to see my doctor and to be honest am not impressed. The last time I saw him he made reference that with a bp of 155/90 I would live a long life. Good doctors are hard to come by in Northern California where I live which is on the Oregon Border.
Thanks for listening.