How Kidney Disease Is Diagnosed
Diagnosing kidney disease should be done as early as possible to slow the progression of kidney damage and increase your life expectancy. Early detection can also help reduce the risk of related medical conditions, including high blood pressure, diabetes, heart disease, or stroke.
In this article, you'll understand the importance of early detection, get familiar with the symptoms, tests, and stages, and identify who's at risk for kidney disease.
You'll also discover how to maintain kidney health and cope with a diagnosis.

Jump to:
- Key Takeaways
- What is CKD?
- Recognizing the Symptoms of Kidney Disease
- Understanding the Role of Blood and Urine Tests in Diagnosis
- Detailed Examination: Additional Diagnostic Tests for CKD
- Knowing the Five Stages of Kidney Disease
- The Critical Role of Early Detection
- Chronic Kidney Disease: An Overview and Global Impact
- Identifying Who Is at Risk for Chronic Kidney Disease
- Living With Chronic Kidney Disease: Management and Coping Strategies
- Taking Charge: Steps to Ensure Kidney Health
- Frequently Asked Questions
- Early Diagnosis Is Important In CKD
Key Takeaways
- Blood and urine tests are crucial diagnostic tools for kidney disease.
- Understanding the five stages of kidney disease is important for diagnosis and management.
- Glomerular Filtration Rate (GFR) calculation plays a key role in diagnosing kidney disease.
- Diagnostic tests such as ultrasound, CT scan, MRI, contrast studies, and kidney biopsy can provide further information about kidney health and function.
What is CKD?
Chronic Kidney Disease (CKD) is a long-term, progressive condition in which the kidneys gradually lose their ability to function properly. The kidneys play a crucial role in filtering waste products and excess fluids from the blood, regulating blood pressure, and maintaining a balance of electrolytes in the body.
CKD typically develops over an extended period, often with no noticeable symptoms in its early stages. As the disease progresses, waste products and fluids can build up in the body, leading to a range of symptoms and complications. The common causes of CKD include diabetes, high blood pressure, glomerulonephritis, and polycystic kidney disease.
CKD is categorized into five stages based on the Glomerular Filtration Rate (GFR), which measures kidney function. In the early stages, kidney damage may be present, but symptoms are minimal. In later stages, as kidney function declines, symptoms become more apparent, and treatment focuses on managing complications and slowing disease progression.
Early detection and management are crucial in preventing CKD from advancing to end-stage renal disease (ESRD), where kidney function is severely impaired, and life-sustaining treatments like dialysis or kidney transplant are required. Regular check-ups, blood pressure control, and lifestyle modifications are essential for managing CKD effectively.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.

Recognizing the Symptoms of Kidney Disease
Recognizing the symptoms of kidney disease is crucial in its early diagnosis and management. You've got to understand the early warning signs, which often go unnoticed due to their subtlety.
Also, it's important to gauge the severity of these symptoms, as this can indicate the progression of the disease.
Identifying Early Warning Signs
Chronic Kidney Disease often exhibits subtle early warning symptoms that can be easily overlooked. These subtle signs may include unexplained fatigue and a persistent lack of energy, which can result from the accumulation of waste products in the bloodstream due to reduced kidney function.
Changes in urine color or the presence of foamy urine may also indicate kidney issues. Additionally, individuals might experience slight changes in urinary frequency or urgency. Swelling, particularly in the hands, ankles, or feet, can occur due to fluid retention, a consequence of the kidneys' reduced ability to remove excess fluids.
Another subtle sign is the onset of high blood pressure, which can be both a cause and a result of kidney damage. Increased protein levels in the urine, known as proteinuria, is another subtle but important early indicator of kidney dysfunction.
These symptoms can be subtle and easily attributed to other factors, making regular medical check-ups crucial for early detection and intervention.
Understanding Symptom Severity
Severe Chronic Kidney Disease or End-Stage Renal Disease (ESRD) often presents with more pronounced and concerning symptoms. These can include extreme fatigue, nausea, vomiting, and a loss of appetite. Individuals may experience muscle cramps, weakness, and persistent itching due to the buildup of waste products and toxins in the body.
Additionally, there may be significant changes in urine output, with some patients producing very little urine (oliguria) or even none at all (anuria). Swelling, known as edema, can become severe and affect the legs, arms, and face due to fluid retention. High blood pressure and shortness of breath may also worsen. Cognitive changes, like confusion, may occur due to the accumulation of toxins.
These advanced symptoms often necessitate immediate medical attention and may lead to the consideration of renal replacement therapies such as dialysis or kidney transplantation.
Understanding the Role of Blood and Urine Tests in Diagnosis
In diagnosing kidney disease, your doctor will likely rely heavily on blood and urine tests. These tests can reveal crucial information about your kidney's health, such as creatinine levels in your blood and the presence of abnormal substances in your urine.
Understanding how to interpret these results can give you a clearer picture of your kidney function and disease progression.
Significance of Creatinine Levels
Serum creatinine levels play a crucial role in diagnosing kidney disease because they serve as a reliable indicator of kidney function. Creatinine is a waste product generated by muscle metabolism and is typically filtered out of the blood by the kidneys. When kidney function declines, creatinine accumulates in the bloodstream.
Measuring serum creatinine levels allows health care providers to calculate the estimated glomerular filtration rate (eGFR), which provides an estimate of how efficiently the kidneys are filtering blood. A low eGFR indicates reduced kidney function, potentially signaling the presence of kidney disease.
Regular monitoring of serum creatinine levels and eGFR is vital for tracking the progression of kidney disease, adjusting treatment plans, and assessing the effectiveness of interventions. It helps health care providers detect kidney dysfunction in its early stages when interventions are most effective at slowing or managing the disease.
Other Blood Tests
In addition to serum creatinine levels and estimated glomerular filtration rate, several other blood tests are important in diagnosing and assessing chronic kidney disease (CKD):
- Blood Urea Nitrogen (BUN): BUN measures the level of nitrogen in the blood that comes from urea, a waste product generated by the liver during protein metabolism. Elevated BUN levels can indicate kidney dysfunction.
- Serum Albumin: Low serum albumin levels, a protein produced by the liver, may suggest kidney disease as the kidneys play a role in regulating protein balance in the blood.
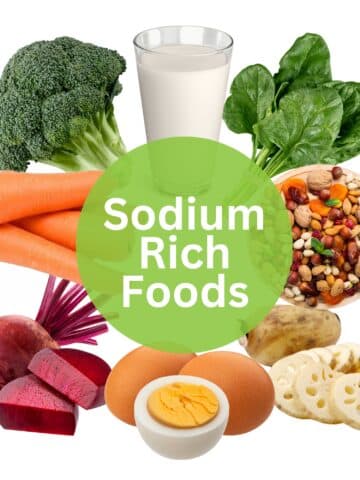
- Serum Electrolytes: Abnormal levels of electrolytes like potassium, sodium, and calcium can occur with CKD, as the kidneys are responsible for maintaining electrolyte balance.
- Complete Blood Count (CBC): A CBC is helpful for evaluation for anemia, a common complication of CKD, by measuring levels of hemoglobin and red blood cells.
- Phosphorus and Calcium Levels: Imbalances in these minerals can occur with CKD and may lead to bone and cardiovascular problems.
- Parathyroid Hormone (PTH): Elevated PTH levels can indicate mineral and bone disorders associated with CKD.
These blood tests, when combined with clinical evaluation and imaging studies, provide a comprehensive assessment of kidney function and help diagnose CKD, determine its stage, and guide treatment decisions. Regular monitoring of these parameters is crucial for managing CKD effectively.
Urine Tests
Urine tests play a crucial role in the diagnosis of chronic kidney disease (CKD). Some of the important urine tests for CKD diagnosis include:
- Urinary Albumin-to-Creatinine Ratio (UACR): This test measures the amount of albumin (a protein) in the urine relative to creatinine (a waste product). Elevated UACR levels suggest kidney damage, particularly in the early stages of CKD.
- Urinalysis: A simple urine dipstick test can detect the presence of blood, protein, or abnormal levels of white blood cells or red blood cells in the urine, all of which can indicate kidney problems.
- Microalbuminuria Test: This test is specifically designed to detect small amounts of albumin in the urine and is often used to detect early kidney damage in individuals with diabetes or hypertension.
- Urine Sediment Examination: This involves examination of sediment from a urine specimen under a microscope to identify the presence of abnormal cells, crystals, or cellular casts, which can provide additional insights into the underlying cause of kidney disease.
These urine tests, when combined with blood tests and clinical evaluation, help diagnose CKD, determine its cause, and assess its severity. Early detection through urine testing is crucial for timely intervention and management of CKD to prevent further kidney damage.
Albumin:Creatinine Ratio Significance
The Albumin-to-Creatinine Ratio (ACR) is a vital diagnostic tool in assessing kidney health, especially in the context of chronic kidney disease. ACR measures the levels of albumin, a protein, relative to creatinine, a waste product, in a urine sample. Elevated ACR levels indicate the presence of excess albumin in the urine, a condition known as albuminuria or proteinuria.
ACR is significant because it helps in the early detection of kidney damage, often before noticeable symptoms occur. It is particularly valuable for individuals at risk of CKD, such as those with diabetes or hypertension, as it allows for timely intervention and management to prevent further kidney deterioration. Monitoring ACR over time is essential in assessing the progression of kidney disease and the effectiveness of treatment strategies.
Here's a quick guide to help you interpret the results.
| Albumin to Creatinine Ratio | Implications |
| <30 mg/g | Normal |
| 30-300 mg/g | Microalbuminuria (early stage kidney disease) |
| >300 mg/g | Macroalbuminuria (advanced kidney disease) |
Understanding these levels is key in managing and treating kidney disease effectively.
Detailed Examination: Additional Diagnostic Tests for CKD
In addition to standard blood and urine tests, diagnosing and monitoring chronic kidney disease often involves a range of additional diagnostic tools. These include imaging tests and kidney biopsies, which provide deeper insights into the condition of the kidneys.
Understanding these supplementary diagnostic methods is crucial for a comprehensive assessment of CKD's progression and its underlying causes. In this section, we'll explore these additional diagnostic tests, their significance, and how they contribute to a more accurate diagnosis and treatment of CKD.
Imaging Tests Importance
Imaging plays a crucial role in the diagnosis and management of chronic kidney disease. Several imaging modalities are employed to assess kidney health and provide valuable insights into the structural aspects of the kidneys which may be seen as imaging abnormalities.
Ultrasound or renal ultrasonography is a common choice, as it is non-invasive, widely available, and cost-effective. It helps visualize kidney size, shape, and any structural abnormalities, aiding in the initial assessment of CKD.
Computed Tomography (CT) scans offer detailed cross-sectional images of the kidneys, helping detect tumors, cysts (which can be simple cysts or complex cysts), or urinary tract obstructions that might be impacting kidney function.
Magnetic Resonance Imaging (MRI) provides high-quality images without radiation exposure, making it suitable for certain patients and specific diagnostic needs.
These imaging options are essential in identifying structural issues, guiding treatment decisions, and monitoring disease progression in CKD. They complement blood and urine tests, contributing to a comprehensive diagnostic approach that enables health care providers to offer the most effective management strategies for patients with kidney disease.
Kidney Biopsy Necessity
Kidney biopsy is a valuable diagnostic tool in certain cases of chronic kidney disease when more detailed information is needed beyond blood and urine tests. It involves the removal of a tiny tissue sample from the kidney for examination under a microscope. This procedure is typically recommended when the cause of CKD is unclear, or when the severity and type of kidney damage need to be precisely determined.
Kidney biopsy helps identify the underlying disease or condition causing CKD, such as glomerular diseases or autoimmune diseases. It provides critical insights into the extent of damage, inflammation, and scarring in the kidneys, guiding treatment decisions and predicting disease progression.
While kidney biopsy carries some risks and is not necessary for all CKD patients, it is a valuable tool for nephrologists and health care teams to ensure accurate diagnosis and tailored management plans for those with more complex or severe kidney conditions.
Knowing the Five Stages of Kidney Disease
Now, let's turn our focus to the five stages of kidney disease and how they're identified, specifically through understanding the Glomerular Filtration Rate (GFR) calculation.
It's crucial to comprehend how each stage progression impacts overall kidney function and health.
Understanding GFR Calculation
Glomerular filtration rate (GFR) is a crucial measure for diagnosing and staging chronic kidney disease (CKD). It estimates how efficiently your kidneys are filtering waste from your blood, providing valuable information about kidney function.
GFR can be calculated using various equations, with the Modification of Diet in Renal Disease (MDRD) and the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equations being commonly used.
These equations take into account factors such as serum creatinine levels, age, gender, and race to estimate GFR. A lower GFR indicates reduced kidney function, and if this reduced GFR persists for over three months, it can lead to a diagnosis of CKD.
Accurate GFR estimation is vital as it helps determine the stage of CKD, guiding treatment decisions and monitoring disease progression. It also aids in assessing the effectiveness of interventions to slow down CKD's advancement.
Stage Progression
There is a GFR chart widely used in the medical profession that determines what stage of kidney disease you are in once you are diagnosed.
The numbers that go with each stage are:
Stage 1: 90+ GFR, 90-100% Kidney Function
Stage 2: 89-60 GFR, 89-60% Kidney Function
Stage 3: 59-30 GFR, 59-30% Kidney Function
Stage 4: 29-15 GFT, 20-15% Kidney Function
Stage 5: 15 or under GFR, Less than 15% Kidney Function, also known as End-Stage Kidney Disease
When your doctor has calculated your GFR, this chart is used to determine just how bad the kidney disease is. Your numbers will continue to drop as your kidney health declines over time.
Once you have landed into one of the above 5 stages, you are said to have chronic kidney disease. The damage done to the kidneys is typically not reversible, but you and your doctor can create a plan to help reduce the symptoms and prevent rapid progression of renal failure.
The Critical Role of Early Detection
Recognizing the signs of kidney disease early is of utmost importance. It's essential to understand that timely detection can improve your prognosis significantly, offering various treatment options that could potentially slow down the disease's progression.
Let's discuss the advantages of early detection and the ways to expedite the diagnosis process.
Benefits of Early Detection
Early detection of chronic kidney disease offers numerous benefits for individuals at risk or experiencing kidney problems. Firstly, it allows for timely intervention, enabling health care providers to implement strategies to slow or prevent further kidney damage. Lifestyle modifications, medication management, and blood pressure control are more effective when initiated early, potentially preserving kidney function.
Secondly, early detection can help identify the underlying causes of CKD, such as diabetes or hypertension. Addressing these root causes through proper management can have a significant impact on kidney health.
Thirdly, it provides an opportunity for patients to actively engage in their healthcare. Being aware of CKD allows individuals to make informed choices about their diet, exercise, and medication adherence. This proactive approach can improve their overall quality of life and potentially delay the progression of the disease.
In summary, early detection empowers both healthcare providers and patients to take action, offering the best chance to manage CKD effectively and prevent its complications.
Improving Diagnosis Timeliness
Improving the timeliness of chronic kidney disease (CKD) diagnosis hinges on regular check-ups and proactive healthcare engagement. Individuals at risk for CKD, such as those with diabetes, high blood pressure, or a family history of kidney disease, should prioritize routine health visits. Here's how regular check-ups aid in timely diagnosis:
- Early Detection: Regular check-ups facilitate the monitoring of key indicators like blood pressure, serum creatinine levels, and urine albumin. Any deviations from normal values can prompt further evaluation for kidney disease.
- Risk Assessment: Health care providers can assess an individual's risk factors and tailor their medical care accordingly. This includes providing guidance on managing conditions like diabetes and hypertension that contribute to CKD.
- Preventive Measures: Timely check-ups allow for preventive measures, such as lifestyle changes and medication management, which can slow CKD progression or prevent its development.
- Patient Education: Regular visits provide opportunities for patients to learn about CKD risk factors, symptoms, and self-care strategies, promoting proactive engagement in managing their kidney health.
Incorporating regular check-ups into one's healthcare routine is crucial for early CKD detection and improved outcomes.
Chronic Kidney Disease: An Overview and Global Impact
Understanding the global prevalence of chronic kidney disease is paramount in addressing this silent epidemic. CKD transcends borders and affects millions worldwide. This section delves into CKD's global footprint.
By examining its prevalence on a global scale, we gain insights into the magnitude of the issue, informing public health initiatives, early detection strategies, and better management to reduce its impact on individuals and healthcare systems globally.
Global Prevalence of CKD
Chronic kidney disease is a global health crisis, affecting over 10% of the world's population, which amounts to more than 800 million individuals. This prevalence is influenced by various factors, with higher rates seen in older adults, women, racial minorities, and those grappling with diabetes mellitus and hypertension.
Alarmingly, CKD disproportionately burdens low- and middle-income countries, where healthcare resources and infrastructure to address it are often limited.
In recent years, CKD has emerged as a leading cause of mortality on a global scale. What's particularly concerning is that it stands out as one of the few non-communicable diseases that has witnessed a significant increase in associated deaths over the past two decades.
This underscores the urgency of addressing CKD on a global scale, highlighting the need for awareness, early detection, and effective management strategies to mitigate its impact on both individuals and healthcare systems worldwide.
CKD in the USA
Chronic kidney disease is a prevalent health issue in the United States, affecting a significant portion of the population. Recent estimates indicate that approximately 14% of U.S. adults, which translates to around 35.5 million people, grapple with CKD. It's alarming to note that a substantial proportion of these individuals remain unaware of their condition, with up to 9 in 10 adults with CKD being undiagnosed.
Age plays a significant role in CKD prevalence, with a higher incidence among those aged 65 years or older, affecting about 34% of this demographic. It's noteworthy that CKD is slightly more common in women (14%) than in men (12%).
Furthermore, the prevalence of CKD varies among racial and ethnic groups, with non-Hispanic Black adults experiencing a higher incidence at 20%, while non-Hispanic Asian adults stand at 14%, and non-Hispanic White adults at 12%. About 14% of Hispanic adults also grapple with CKD.
These statistics emphasize the need for increased awareness, regular check-ups, and proactive management to address this widespread health concern in the U.S. population.
Identifying Who Is at Risk for Chronic Kidney Disease
Understanding the risk factors for chronic kidney disease is paramount for early intervention and prevention. Various factors, such as underlying health conditions and lifestyle choices, can elevate your risk of developing CKD. In this section, we'll delve into these risk factors and provide insights into what you can do if you find yourself in a high-risk category. Awareness and proactive steps can significantly mitigate the chances of CKD, making it essential to recognize and address these potential vulnerabilities.
Risk Factors for CKD
Chronic kidney disease is a complex condition influenced by various risk factors. Some of these factors can be modified through lifestyle changes, while others are non-modifiable:
- Diabetes: Individuals with uncontrolled diabetes are at a significantly higher risk of developing CKD (diabetic kidney disease or diabetic nephropathy). Elevated blood sugar levels can damage the tiny blood vessels in the kidneys, impairing their function over time.
- Hypertension: High blood pressure can strain the kidneys, leading to kidney damage. Conversely, CKD can also contribute to hypertension, creating a harmful cycle.
- Age: CKD is more prevalent in older adults, as kidney function naturally declines with age.
- Family History: A family history of kidney disease may increase an individual's susceptibility.
- Ethnicity: Some ethnic groups, such as African Americans, Hispanics, and Native Americans, have a higher risk of CKD.
- Obesity: Excess body weight can stress the kidneys and increase the risk of CKD.
- Smoking: Smoking damages blood vessels and can promote more loss of kidney function.
- Cardiovascular Disease: Heart disease and CKD often coexist, with each condition contributing to the progression of the other. Ventricular hypertrophy is a common finding especially in hypertensive patients.
- Kidney Infections and Stones: Repeated urinary tract infections and kidney infections or the presence of kidney stones can lead to CKD.
- Prolonged Medication Use: Some medications, especially nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics, can harm the kidneys when used over an extended period.
Understanding these risk factors is crucial for early detection and implementing preventive measures, such as managing chronic conditions, adopting a healthy lifestyle, and regular medical check-ups.
What To Do If You’re At Risk
If you are at risk for chronic kidney disease, taking proactive steps is essential to safeguard your kidney health.
Here's what you can do:
Regularly visit your health care provider for comprehensive check-ups. Monitoring your blood pressure, blood sugar, and kidney function through blood and urine tests can help detect any issues early. If you have conditions like diabetes or hypertension, work closely with your healthcare team to keep them under control.
Properly managing these conditions can reduce the risk of kidney damage. Adopt a kidney-friendly lifestyle by maintaining a balanced diet low in salt, managing your weight, staying physically active, and avoiding tobacco products. Adequate hydration is crucial, but consult your doctor if you have specific fluid restrictions due to kidney problems.
Be cautious with over-the-counter medications, especially NSAIDs, which can harm your kidneys when used excessively. Consider working with a dietitian to create a kidney-friendly diet plan that suits your specific needs, especially if you have early signs of CKD. Understanding your family's medical history can provide insights into your risk factors.
Early detection and management play a pivotal role in preventing CKD from progressing to more advanced stages. Being proactive about your health and following your health care provider's guidance can help preserve your kidney function and overall well-being.
Living With Chronic Kidney Disease: Management and Coping Strategies
Living with chronic kidney disease requires more than medical treatments. It also demands significant lifestyle changes and emotional resilience. You'll need to adapt your diet, exercise regimen, and daily routine to cope with the nuances of this condition.
Additionally, we'll explore strategies to garner emotional support. This aspect is often overlooked but is crucial in managing CKD.
Lifestyle Changes for CKD
You'll need to make significant lifestyle changes when managing chronic kidney disease, and these alterations can greatly help in slowing disease progression.
Here's a 4-point list of adjustments you can make:
- Dietary modifications: You'll need to adjust your diet to manage your CKD. This might involve reducing sodium, phosphorus, and potassium intake. A dietitian can help create a meal plan tailored to your needs.
- Exercise importance: Regular physical activity can improve your cardiovascular health, control your weight, and boost your overall wellbeing. Always consult your doctor before starting a new exercise routine.
- Stress management: Techniques like meditation, yoga, and deep breathing can help manage stress levels, which is crucial in controlling your CKD.
- Quitting smoking and limiting alcohol: Both smoking and excessive alcohol can worsen kidney damage. It's important to quit smoking and limit alcohol consumption.
Emotional Support Strategies
Dealing with chronic kidney disease isn't just about managing physical symptoms, it's also about taking care of your emotional health. Emotional resilience and proper coping mechanisms play a vital role in your overall mental health. Stress management techniques can help ease the burden of CKD, while family support can provide a comforting shield on tougher days.
Here's a quick guide to keep in mind:
| Emotional Resilience | Family Support |
| Develop coping skills to handle stress | Engage family in your care journey |
| Practice mindfulness and positive thinking | Share feelings and concerns openly |
Taking Charge: Steps to Ensure Kidney Health
As you navigate the complex landscape of kidney health, it's crucial to stay vigilant for symptoms of kidney disease and take proactive measures.
The recognition of early warning signs - such as proteinuria, hematuria, or hypertension - can significantly impact your journey.
Moreover, incorporating renal-protective strategies into your daily routine, like maintaining a balanced diet and regular exercise, can fortify your kidneys against potential diseases.
Recognizing Kidney Disease Symptoms
In maintaining your kidney health, it's crucial to recognize potential kidney disease symptoms early on. Early detection can lead to disease prevention, dietary changes, exercise importance, stress management, and even herbal remedies that can help maintain your kidney health.
Here are four symptoms to watch out for:
- Persistent Fatigue: If you're continually feeling tired or have a lack of energy, it could be a sign of kidney disease.
- Swollen Ankles or Feet: This swelling could be due to kidneys failing to remove extra fluids.
- Changes in Urination: If you're urinating more often or less often, it might indicate a problem.
- Loss of Appetite: Loss of appetite or an unusual change in your weight might mean your kidneys aren't working properly.
Always consult with your healthcare provider if you notice these symptoms.
Proactive Kidney Health Measures
Taking proactive steps to prevent chronic kidney disease (CKD) is essential for maintaining optimal kidney health. Here are some key measures to consider:
- Regular Health Check-ups: Schedule routine check-ups with your healthcare provider to monitor blood pressure, blood sugar levels, and kidney function through blood and urine tests. Early detection can help prevent CKD progression.
- Manage Chronic Conditions: If you have conditions like diabetes or hypertension, work closely with your healthcare team to keep them under control. Properly managing these conditions can significantly reduce the risk of kidney damage.
- Healthy Lifestyle: Adopt a kidney-friendly lifestyle by maintaining a balanced diet low in salt, managing your weight, staying physically active, and avoiding tobacco products.
- Stay Hydrated: Adequate hydration is crucial, but consult your doctor if you have specific fluid restrictions due to kidney problems.
- Medication Awareness: Be cautious with over-the-counter medications, particularly nonsteroidal anti-inflammatory drugs, which can harm your kidneys if used excessively.
- Dietary Guidance: Consider working with a dietitian to create a kidney-friendly diet plan tailored to your specific needs, especially if you have early signs of CKD.
- Know Your Family History: Understanding your family's medical history is important, as genetics can play a role in kidney disease risk factors.
By taking these proactive measures, you can reduce the risk of CKD and safeguard your kidney health for the long term.
Frequently Asked Questions
Managing kidney disease through dietary changes is vital. Start by controlling protein intake to lessen the strain on your kidneys. Keep a close eye on phosphorus and potassium-rich foods to maintain mineral balance. Reducing sodium helps manage blood pressure and fluid retention. Monitor fluid intake per your doctor's advice to prevent excess fluid buildup. Maintain a balanced diet with limited processed foods and saturated fats. Practice portion control to prevent kidney strain. Collaborate with a registered dietitian for a personalized meal plan tailored to your CKD stage. Control sugar intake, especially with diabetes. Opt for high-quality protein sources like lean meats and fish. Always consult your healthcare team for personalized guidance.
Yes, there have been significant advancements in kidney disease treatment. Precision medicine is becoming more common, allowing for tailored treatments based on individual genetics and disease characteristics. Additionally, there are ongoing studies into novel drugs targeting specific pathways involved in kidney disease progression. The field of regenerative medicine holds promise for kidney regeneration. Telemedicine and remote monitoring are improving patient care and accessibility. However, it's important to note that these advancements are part of ongoing research, and consultation with healthcare providers remains crucial for the most up-to-date treatment options.
Yes, it is generally safe to exercise if you have kidney disease, but it should be done with caution and under the guidance of a healthcare professional. Exercise can have various benefits for kidney health, including improving cardiovascular fitness and overall well-being. However, it's essential to tailor your exercise routine to your individual condition, considering factors like your stage of kidney disease, comorbidities, and fitness level. A healthcare provider or a physical therapist can help design an exercise plan that suits your specific needs and ensures your safety during workouts.
Yes, kidney disease can have a significant impact on mental health. The challenges of living with a chronic condition, managing treatments, and facing uncertainty about the future can lead to feelings of anxiety, depression, and stress. Additionally, physical symptoms like fatigue and sleep disturbances can exacerbate these mental health issues. It's crucial for individuals with kidney disease to seek emotional support, which may include counseling, support groups, or therapy, to address these psychological aspects and improve their overall well-being and quality of life.
Medications used to treat kidney disease can have various side effects, which can vary depending on the specific drug. Common side effects may include gastrointestinal issues like nausea and diarrhea, changes in blood pressure, electrolyte imbalances, and potential interactions with other medications. Some drugs can also affect the function of other organs, like the liver or cardiovascular system. It's crucial for individuals with kidney disease to work closely with their healthcare team to monitor and manage these potential side effects, adjusting treatment plans as needed to ensure the best possible outcomes while minimizing risks.
Early Diagnosis Is Important In CKD
As you can see, it’s important to diagnose kidney disease as early as possible for the best prognosis. The sooner you are diagnosed, the faster your CKD and its symptoms can be managed. Familiarize yourself with the warning signs of kidney disease and discuss any problems you are having with your doctor.