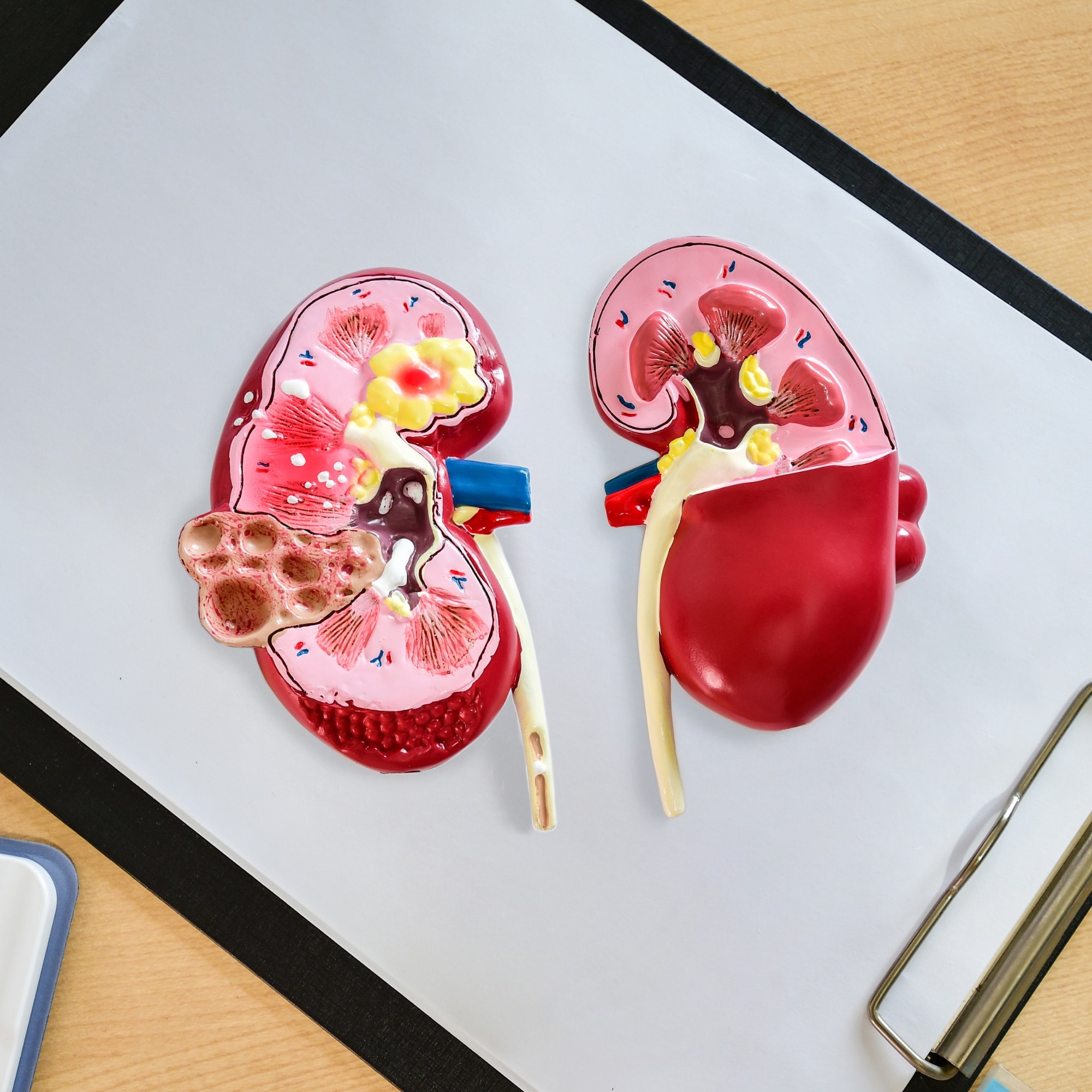
Chronic Renal Failure Diet
You're battling chronic renal failure, and diet plays a crucial role in managing your condition. Understanding how sodium, phosphorus, and potassium affect your kidneys can help slow disease progression.
Let's explore how to customize your meal plan, swap salt for healthier seasonings, and adapt to a low potassium diet while you have Chronic Kidney Disease.
You'll learn to balance nutrients for optimal kidney health while serving up delicious food that benefits you. You're going to find out things like salt substitutes, waste products, phosphate binders, levels of potassium, and so much more.
Jump to:
- Key Takeaways
- Understanding the Importance of Diet in Chronic Renal Failure
- Dietary Adjustments for Kidney Health Improvement
- Slowing Kidney Disease Progression With Nutritional Changes
- The Role of Sodium, Phosphorus, and Potassium in Renal Failure
- Customizing Your Diet Plan for Chronic Renal Failure
- The Impact of Fluid Intake on Kidney Function
- Proteins and Their Role in a Renal Failure Diet
- Alternatives to Salt in a Renal Diet
- Adapting to a Low Potassium Diet in Kidney Disease
- Useful Resources for Managing Chronic Renal Failure Diet
- Why would you need resources for managing chronic renal failure diet?
- Frequently Asked Questions
- Following a Chronic Renal Failure Diet is Possible
Key Takeaways
- A chronic renal failure meal plan can help comfort and reduce complications of kidney disease disorders.
- It is manageable with medical assistance from doctors and dietitians.
- The meal plan can prevent further health problems and kidney malfunctions.
- It helps maintain adequate levels of sodium, phosphorus, and potassium, and improves overall kidney function.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding the Importance of Diet in Chronic Renal Failure
You've got to understand dietary approaches, your diet plays a crucial role in managing chronic renal failure. It can help reduce complications, prevent further kidney malfunctions, and improve overall kidney function. Everything from food labels to fresh foods to canned foods can be understood with a renal dietitian.
Hydration is vital. However, you must balance fluid intake to avoid overloading your kidneys. Whether you get in touch with a kidney dietician to talk about your dietary requirements or you want to focus on a healthy diet, a heart-healthy and kidney diet can go hand in hand together.
Dietary restrictions become necessary too. Limiting high sodium foods reduces pressure on the kidneys while on a kidney diet.
Vitamins and minerals are essential for health but should be consumed with caution. Too much potassium or phosphorus can be detrimental since impaired kidneys struggle to remove these from your body. You'll need professional advice on supplementation and a nutrition plan during kidney failure.
Managing weight in renal failure is crucial as obesity exacerbates renal issues. A well-planned diet helps maintain a healthy weight, while delivering the nutrients required by your body.
Incorporating exercise into a renal diet not only aids weight management, but also improves overall health and wellbeing. Remember though, any physical activity should complement rather than strain your condition.
Your commitment to learning about and adhering to dietary guidelines can make a significant difference in managing this disease effectively. It's not just about eating right, it's about creating an environment for your kidneys where they can perform their best under challenging circumstances for people with kidney disease.
Dietary Adjustments for Kidney Health Improvement
Adjusting what's on your plate can greatly improve kidney health and slow down the progression of the disease. Your meal planning strategies for renal health should adhere to nutritional guidelines for kidney disease management. Incorporating healthy fluids into a renal diet is crucial, as is understanding the importance of portion control in a renal diet.
Here are four key steps you should take:
- Redesign your meals with low-sodium items, restricting phosphorus-rich foods to manage phosphorus levels in chronic renal failure diets.
- Prioritize hydration, but balance fluid intake carefully to prevent overloading your kidneys.
- Practice portion control vigilantly, limiting quantities of proteins, potassium, and sodium.
- Consult regularly with your dietician or healthcare provider to adjust and fine-tune your meal plan, according to your current health status.
Remember that everyone's body responds differently to dietary changes, what works for one may not work for another. Stay patient and persistent with these adjustments; it'll be worth it when you see the improvements in your kidney function tests!
Keep serving yourself nutritiously balanced plates because you're not just eating food, you're nurturing healthier kidneys too. Make sure you're also paying attention to dairy foods, animal protein, and so much more!
Slowing Kidney Disease Progression With Nutritional Changes
Slowing the progression of kidney disease often hinges on making smart nutritional changes. Your focus should be on preventing complications associated with poor renal health. Dietary guidelines play a significant role in this area, helping you maintain balance and control over your condition.
Managing fluid intake is crucial in slowing down kidney disease. Consuming too much liquid can cause swelling, high blood pressure, and further strain on your kidneys. You'll need to limit fluids, but remember, what's right for others may not be right for you, each person's needs are unique.
Next up is evaluating protein requirements. While protein is vital for overall health, excessive amounts can create more work for your kidneys. If you're undergoing dialysis though, increased protein intake becomes essential due to loss during treatment sessions.
Phosphorus control also plays a big part in keeping your kidneys healthy. High phosphorus levels can lead to bone disease over time if left unchecked. Avoid foods high in this mineral or opt for phosphorus binders as suggested by your healthcare provider.
Remember, that these steps are part of an ongoing process requiring perseverance and diligence. Your dedication will pay off as you effectively slow the progression of kidney disease through informed dietary choices.
The Role of Sodium, Phosphorus, and Potassium in Renal Failure
In managing kidney disease, it's crucial to understand the role of sodium, phosphorus, and potassium. Sodium helps maintain fluid balance but too much might strain your kidneys. Thus, dietary restrictions for kidney health often include reducing sodium intake.
Phosphorus is another mineral to watch, excessive levels can cause bone problems in renal failure cases. You'll need to manage phosphorus levels carefully, which may mean avoiding certain high-phosphorus foods like dairy products.
Potassium plays a role in nerve function and muscle control, but its impact on kidney function is significant. High potassium levels can be dangerous for those with renal issues. Hence, tailor your meal plan to limit potassium-rich food.
Hydration plays an essential role in renal failure as well, no matter what stage of kidney disease. Not only does it help the kidneys clear toxins from your blood but also prevents further damage by keeping urine diluted.
Customizing your meal plan for renal failure isn't just about restriction,it's also about making healthier choices that support kidney function, while providing necessary nutrition. Consult with a dietitian or doctor for guidance tailored specifically to you, they can help strike the right balance between nutritional needs and kidney health.
Customizing Your Diet Plan for Chronic Renal Failure
You'll find that personalizing your meal plan to your specific health condition can greatly improve your kidney function and overall well-being. Chronic renal failure meal plans are a lifesaver, especially when it comes to managing fluid intake and complying with dietary restrictions in kidney disease.
Here's how you can customize your diet:
- Fluid Management
- Limit fluids to manage swelling and high blood pressure issues.
- Note that certain foods like ice cream or soup also count as fluid intake.
- Protein Intake
- If you're on dialysis, increase protein intake due to losses during treatment.
- Non-dialysis patients should limit protein to slow down kidney damage.
Dietary restrictions go beyond just fluids and proteins though. For instance, you need to be mindful of phosphorus levels. Too much phosphorus leads to bone disease in renal failure patients.
- Watch Out for High Phosphorus Foods.
- Dairy products often contain high levels of phosphorus, so choose alternatives when possible.
- Opt for fresh fruits and vegetables over processed foods which tend to have added phosphorus.
The Impact of Fluid Intake on Kidney Function
Managing your fluid intake can have a significant impact on your kidney function, particularly if you're dealing with kidney disease. Balancing hydration plays a critical role in renal failure, as both insufficient and excessive fluid levels can strain your kidneys.
| Strategies for Maintaining Hydration | Effects on Kidney Health |
|---|---|
| Drinking adequate water daily | Supports kidney function by flushing out toxins |
| Limiting high-sodium foods | Prevents water retention and reduces burden on kidneys |
| Monitoring liquid in meals | Ensures accurate tracking of total fluid intake |
| Avoiding caffeine and alcohol | Reduces risk of dehydration and kidney damage |
| Regularly checking body weight | Helps detect sudden changes due to fluid accumulation |
Monitoring the amount, type, and timing of fluids you consume is vital for managing kidney disease. This practice can help control blood pressure, prevent swelling, and slow down the progression of chronic renal failure. Overdoing it though can overwork your kidneys leading to health complications.
Understanding the impact of hydration on kidney function is crucial. Keep track of your consumption diligently while maintaining proper hydration strategies. After all, every sip counts when it comes to protecting your kidneys.
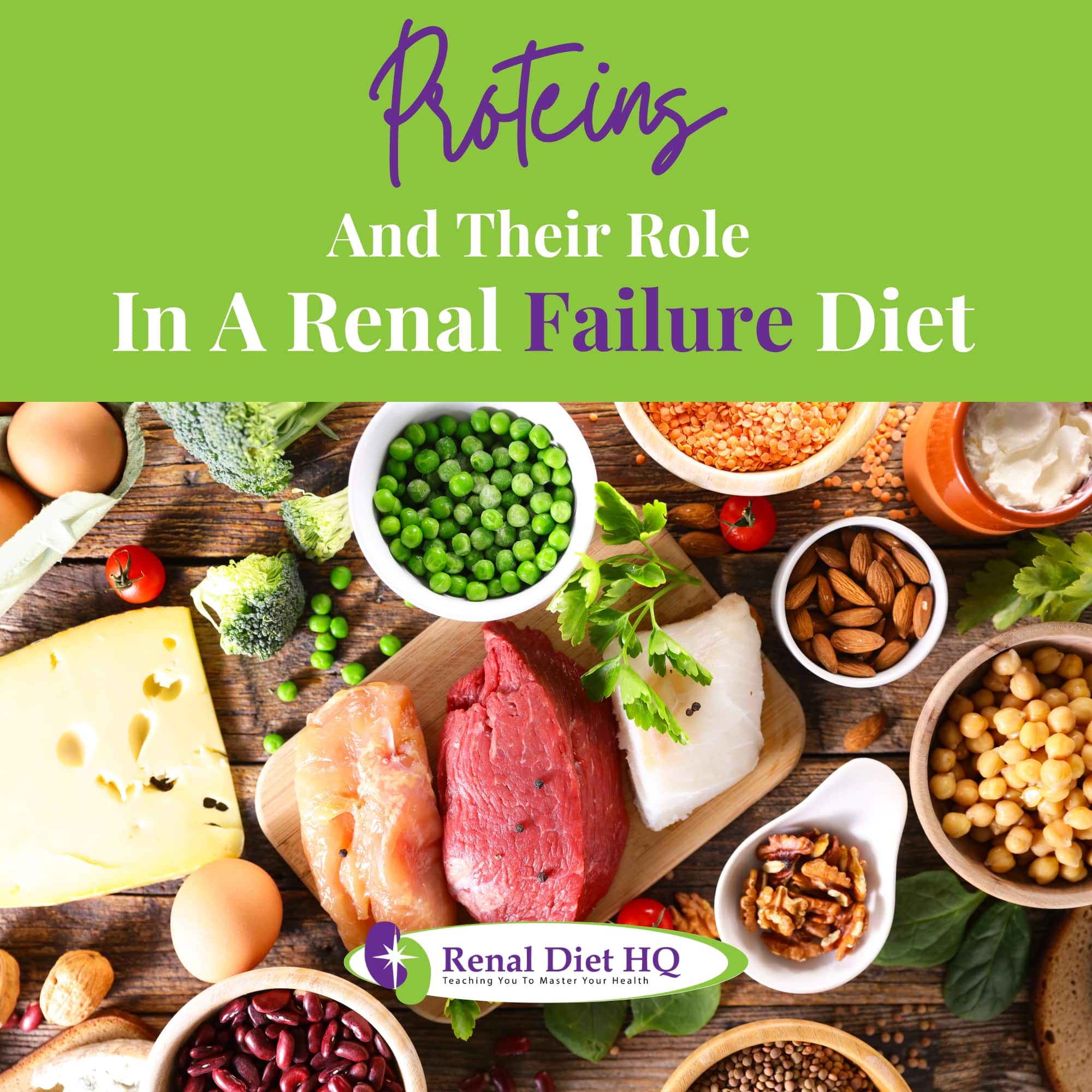
Proteins and Their Role in a Renal Failure Diet
Proteins play a critical role in a kidney-friendly meal plan, particularly for dialysis patients who need to compensate for protein loss. When managing renal health, it's crucial that you understand the connection between proteins and your kidneys.
With dietary restrictions in renal failure, you're not just cutting back on certain foods, but actively improving your body's ability to process waste. That's why managing fluid intake is so important, overloading your system can lead to complications.
Here are some key points about proteins and renal health:
- High-quality proteins (like fish and lean meats) ease the burden on your kidneys.
- Balancing protein intake with hydration helps flush out toxins.
- Over-consuming proteins can strain kidneys, exacerbating issues in renal failure.
- Certain plant-based proteins may help manage potassium levels in a renal diet.
- Dialysis patients often require more protein to offset losses during treatment.
Remember, every individual's needs will vary based on their specific condition. Always consult with healthcare providers when crafting a meal plan tailored to support renal health, they're there to guide you as you navigate this journey towards better wellbeing.
Alternatives to Salt in a Renal Diet
In your quest for kidney health, it's essential to explore alternatives to salt as part of a balanced meal plan. Reducing milligrams of sodium intake is a crucial step in protecting your kidneys and managing fluid levels effectively. But don't worry, flavoring without salt doesn't mean sacrificing taste!
| Low Sodium Alternative | Usage |
|---|---|
| Lemon Juice | Brightens up dishes |
| Vinegar | Adds tanginess |
| Herbs & Spices | Infuses aromatic flavors |
By using these options, you're not only reducing sodium but also introducing new and exciting flavors into your meals.
Now let's talk about low phosphorus options and protein sources. It's important to keep phosphorus at bay while ensuring enough proteins are included in your diet.
| Protein Source | Phosphorus Level |
|---|---|
| Egg Whites | Low |
| Tofu | Moderate |
These are just some examples. Remember, it's all about balance! Always consult with a dietitian or healthcare professional before making drastic changes to your renal diet. They've got the expertise to help navigate through this journey towards better kidney health with you!
Adapting to a Low Potassium Diet in Kidney Disease
Adapting to a low potassium meal plan is crucial for individuals battling kidney disease. It's your chance to safeguard the health of your kidneys and maintain your overall well-being.
Consider the following three steps:
- Explore Low Potassium Alternatives: Many fruits and vegetables are high in potassium, but there are alternatives you can enjoy. Swap bananas for apples, or spinach for green beans.
- Master Fluid Management: Too much fluid could strain your kidneys. Monitor how much you drink, including soups or other liquid-based foods.
- Balance Protein Intake: Dialysis patients often need more protein, but it's important not to overdo it.
But it doesn't stop there. Sodium reduction is another critical aspect of managing kidney disease – use herbs and spices instead of salt where possible.
You're not on this journey alone though, there are plenty of renal diet resources available to guide you through this process, from online guides and cookbooks to trained dietitians who specialize in kidney health.
Remember, every step you take towards managing your diet better contributes significantly towards slowing down the progression of kidney disease while enhancing the quality of your life.
Useful Resources for Managing Chronic Renal Failure Diet
You'll find countless resources available to help you manage your kidney health through nutrition, from informative websites and detailed cookbooks to experienced dietitians specializing in this specific area. They understand hydration's crucial role in renal health, helping you balance fluid intake to prevent overworking your kidneys.
Why would you need resources for managing chronic renal failure diet?
- Diseased kidneys
- Damaged kidneys
- Kidney disease treatment
- Kidney-friendly food
- Blood phosphorous levels
- Risk of heart disease
- Blood sugar levels
- Blood phosphorous levels
Managing phosphorus levels can be a tricky part of a kidney-friendly diet, but they'll guide you in identifying and controlling high-phosphorus foods. This knowledge is key to preventing further kidney damage.
Renal diet education is another invaluable tool these resources provide. You'll learn about the intricacies of your condition and how dietary adjustments can significantly improve your quality of life. They'll offer meal planning tips tailored specifically for chronic renal failure patients like yourself.
Understanding the benefits of dietary adjustments may seem overwhelming at first, but remember that even small changes can have big impacts on your health. The right resources will empower you with the knowledge to take control of your disease through proper nutrition.
Frequently Asked Questions
If you're experiencing persistent kidney pain, unexpected weight loss, or swelling due to fluid imbalance, it might indicate a need for intervention. Perhaps your salt intake is too high or you're not getting enough nutritional supplements.
Maybe you've noticed changes in urination patterns or fatigue from protein restriction. These symptoms could suggest that a specialized meal plan might be beneficial for managing chronic renal failure.
Yes, physical activities are highly recommended to complement your diet. Exercise benefits include improved muscle function and blood pressure control. However, be aware of activity limitations due to your condition.
Yoga's effectiveness in stress reduction can be particularly helpful. Walking also has a positive impact on heart health while swimming offers low-impact advantages for joints.
Always consult your doctor before starting any exercise regimen.
Adhering to a strict meal plan can impact your mental health, causing stress or feelings of restriction. It's essential to develop emotional resilience and use coping mechanisms like seeking psychological support or practicing stress management techniques as your diet approaches.
Yes, medication can interfere with a chronic renal failure meal plan. You'll need to manage medication adjustments and be wary of herbal interactions and supplement risks that could affect your diet.
Drug absorption may also vary based on what you eat. Polypharmacy challenges can arise too, especially with multiple medications interacting negatively with certain foods.
Always consult your healthcare provider for personalized advice to prevent these issues from disrupting your renal health management plan.
Following a Chronic Renal Failure Diet is Possible
Managing your kidney health with a Chronic Renal Failure Meal Plan can be the key to slowing disease progression and enhancing your overall well-being.
Remember, it's not just about restricting certain nutrients, it's also about consuming enough protein and finding tasty salt alternatives to help preserve healthy kidneys.
Adapting to a low potassium diet may seem challenging, but plenty of resources are available for guidance.
Always customize your diet plan according to your specific needs and conditions. Eat as many leafy vegetables as you can and get on a healthy eating plan that will help you get the right source of fiber and the right source of phosphorous.











“A Chronic Renal Failure Meal Plan Is Important in Pre-Dialysis Kidney Disease” in fact
causes myself contemplate a tiny bit further. I admired every particular section of it.
Many thanks -Annie