Constipation And Kidney Disease
If you're one of the millions of people in the US suffering from constipation, you may be at risk for chronic kidney disease (CKD).
Constipation is a common digestive issue that affects over 42 million Americans and has been linked to a 13% higher risk of developing CKD. This is because gut health is closely tied to kidney health, as uremic toxins associated with CKD can originate in gut bacteria.
Long-term constipation can have negative effects on your overall health and well-being. It can lead to complications such as hemorrhoids, fecal impaction, and anal fissures. Additionally, if left untreated or managed improperly, it can increase your risk of other medical issues such as cardiovascular risks (exercise for healthy heart).

However, there are non-pharmacological strategies you can employ to prevent and treat constipation in CKD patients, including maintaining a balanced diet rich in fiber and staying hydrated.
In this article, we will explore the link between constipation and CKD and provide practical tips for managing this condition effectively.
Jump to:
- Key Takeaways
- What is Constipation?
- Association Between Constipation and CKD
- Negative Effects of Long-term Constipation
- Prevention and Treatment
- CKD and Cardiovascular Disease
- Gut Health and CKD
- Prevalence in CKD
- Diagnosis of Constipation in CKD
- 5 Ways On How to Prevent Constipation and Promote Good Gut Health
- Pharmacologic Approaches to Constipation in CKD
- Complications of Constipation in CKD
- FAQs Constipation and CKD
- Constipation Is Common, But Don’t Let It Stop You!
Key Takeaways
- Constipation increases the risk of developing chronic kidney disease (CKD) and severity of constipation increases the risk further.
- Gut health is linked to kidney health and uremic toxins linked to CKD can originate in gut bacteria.
- Eating a well-balanced diet with fiber-rich foods, staying hydrated, and avoiding skipping meals can prevent constipation and promote gut and kidney health.
- Adequate management of constipation may provide additional therapeutic benefits beyond defecation control in CKD patients.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
What is Constipation?
A person is said to have constipation if either of the following are true:
- Less than 3 bowel movements each week
- Bowel movements containing stools which are hard and/or dry, which makes this difficult to pass from the body
Did you also know that this condition can increase the risk of developing chronic kidney disease and negatively affect gut health?
Constipation can be caused by a variety of factors, including low dietary fiber intake, dehydration, a sedentary lifestyle, and certain medications. Constipation-related symptoms include difficulty passing stool, infrequent bowel movements, abdominal discomfort or pain, bloating, and other gastrointestinal symptoms.
To manage constipation, increasing dietary fiber intake through a well-balanced diet with fruits and vegetables can promote healthy bowel movements and balance of bacteria growth in the gut. Prebiotic foods containing fiber or complex carbs that gut bacteria use for energy can also aid in prevention.
Additionally, staying hydrated with at least 64 ounces of water per day helps keep things moving smoothly through the gut.
Proper management of constipation is important as prolonged constipation can lead to complications such as hemorrhoids and rectal prolapse. Taking proper precautions like maintaining a healthy diet and staying hydrated can reduce the chances of constipation and other medical issues.
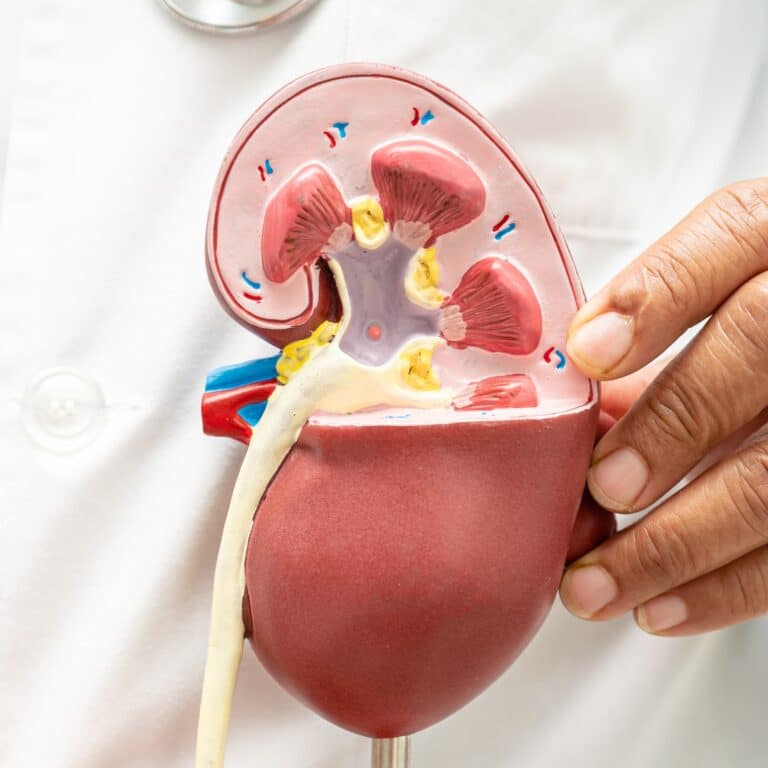
Association Between Constipation and CKD
If you're struggling to stay regular, it's important to know that there's a relationship between constipation and the health of your kidneys.
Constipation sufferers have a 13% higher risk of developing chronic kidney disease, and the severity of constipation increases this risk. This is because gut health is linked to kidney health, and uremic toxins linked to CKD can originate in gut bacteria. Thus, the pathophysiology of constipation is especially complex among those with low glomerular filtration rate.
Research has shown that gut microbiota in patients with constipation play a role in kidney disease progression. Sedentary lifestyle, dietary restrictions, concomitant medications, and multiple comorbidities make constipation common in CKD patients.
Severe constipation negatively affects quality of life and imposes social and economic burden. It's independently associated with adverse clinical outcomes like End-Stage Renal Disease or kidney failure, cardiovascular events, and mortality. Alteration of fecal microflora and increased production of metabolites may contribute to these adverse events.
Therefore, adequate management may provide additional therapeutic benefits beyond defecation control for CKD patients suffering from constipation.
Predisposing factors for constipation in CKD include strict dietary restrictions on potassium content/phosphate intake/fiber intake/high fluid intake requirements, frequent use of constipation-inducing medications, uremic toxins, and altered gut microbiota due to comorbidities like diabetes (ckd and diabetes medications) or obesity or other conditions such as liver cirrhosis or inflammatory bowel disease.
However, non-pharmacological strategies are considered the first-line treatment for constipation in CKD due to their low cost and fewer side effects compared to laxative drugs.
Negative Effects of Long-term Constipation
Long-term constipation can have detrimental effects on a person's overall health and wellbeing. Prolonged periods of constipation can lead to hemorrhoids, rectal prolapse, and an increased cardiovascular risk in older adults. Furthermore, research shows that chronic constipation is linked to the development of chronic kidney disease (CKD).
The negative effects of chronic constipation are especially relevant for CKD patients. In addition to the physical discomfort caused by long-term constipation, it can also exacerbate existing symptoms (progression of symptoms for CKD) associated with CKD such as hypertension and electrolyte imbalances.
Moreover, studies suggest that alteration of gut microbial flora and increased production of fecal metabolites may contribute to adverse renal outcomes in CKD patients.
Targeted treatment for gut dysbiosis may be helpful in alleviating symptoms associated with both chronic constipation and CKD.
However, preventive measures should also be taken into consideration to reduce the prevalence of these issues in at-risk populations. These measures include increasing fiber intake through a well-balanced diet containing prebiotic foods, staying hydrated through proper hydration practices, and incorporating regular exercise into daily routines.
Prevention and Treatment
Incorporating high fiber, prebiotic foods into your daily meals can promote gut health and prevent digestive issues.
Foods such as apples, blueberries, navy beans, pears, whole grains, bananas, onions, and garlic are rich in fiber and prebiotics that the gut bacteria feed on for energy.
Increasing your fiber intake promotes healthy bowel movements and good gut bacteria growth. A plant-based diet is a great way to ensure you're getting enough fiber in your daily meals (plant based meat low sodium).
Staying hydrated with 64 ounces of water per day helps keep things moving through the gut. Proper hydration is important for both gut and kidney health.
Skipping meals can cause constipation and disrupt the balance of gut bacteria. Eating small frequent meals throughout the day can help maintain proper hydration levels while also promoting healthy digestion.
In addition to consuming high fiber foods and staying properly hydrated, incorporating physical activity into your daily routine can also help improve gut health and prevent constipation. Aerobic exercise has been shown to improve many health-related outcomes, including quality of life.
Overall, maintaining a healthy lifestyle with regular physical activity and a balanced diet rich in prebiotic foods will go a long way in preventing constipation and promoting overall gut health.
CKD and Cardiovascular Disease
Maintaining a healthy lifestyle through regular physical activity and a balanced diet can have positive effects on cardiovascular health in individuals with CKD.
Proper management of CKD and its associated risk factors, such as hypertension and diabetes, can also reduce the risk of developing cardiovascular disease. In addition, medication management is crucial to controlling blood pressure and reducing the risk of heart attack or stroke.
Dietary interventions are an important aspect of managing CKD and preventing cardiovascular disease. A kidney-friendly diet that's low in sodium, phosphorus, and potassium may be necessary for some individuals with CKD.
Incorporating more fruits, vegetables, whole grains, and lean protein into your diet can also improve overall health and reduce the risk of cardiovascular disease. It's important to consult with a healthcare provider or registered renal dietitian to develop a personalized nutrition plan that meets your individual needs.
Exercise therapy is another key component in maintaining cardiovascular health in individuals with CKD. Regular physical activity can help lower blood pressure, improve cholesterol levels, and decrease body weight - all factors that contribute to improved heart health.
Starting slowly with low-impact activities such as walking or biking is recommended for those who are new to exercise or have limited mobility due to their condition. It's important to speak with your healthcare provider before starting any new exercise regimen to ensure it's safe for you.
Gut Health and CKD
Improving your gut health can have significant positive effects on overall health and well-being, especially for individuals with CKD. The gut microbiota plays a crucial role in maintaining the balance between harmful and beneficial bacteria.
In CKD patients, alterations in gut microbiota can result in increased production of uremic toxins that may contribute to adverse outcomes.
Therefore, maintaining a healthy gut microbiota is essential for preventing constipation, reducing inflammation and oxidative stress, improving renal function, and enhancing quality of life.
Non-pharmacological interventions such as increasing physical activity and fiber intake have been shown to improve bowel habits and overall health in CKD patients. Incorporating plant-based diets into daily meals has also been associated with better outcomes in CKD patients due to their lower potassium and phosphate content compared to animal sources or processed foods.
Additionally, biotics supplementation (prebiotics, probiotics, synbiotics) has been found to be effective in alleviating constipation by restoring a healthy gut microbiota balance.
In implementing these non-pharmacological strategies for improving gut health in CKD patients, it is important to seek guidance from healthcare professionals who specialize in renal nutrition. They can help tailor an individualized plan that meets the patient's specific needs while taking into account any dietary restrictions and medication use (ckd and diabetes medications).
By incorporating these practices into daily routines, individuals with CKD can take steps towards improving their gut health and overall well-being.
| Non-Pharmacological Interventions | Benefits |
| Increasing physical activity | Improves bowel habits; reduces inflammation & oxidative stress |
| Fiber intake | Promotes healthy bowel movements; improves renal function |
| Plant-based diets | Lower potassium & phosphate content than animal sources/processed foods; associated with better outcomes in CKD |
| Biotics supplementation (pre-, pro-, synbiotics) | Effective at alleviating constipation; restores healthy gut microbiota balance |
Prevalence in CKD
You may be surprised to learn about the high prevalence of constipation in individuals with CKD. According to studies, this condition is a prevalent disorder in all stages of CKD, and based on the epidemiology of constipation, up to 71.7% of renal patients are affected.
Risk factors for constipation in this population include advanced age, low fruit intake, presence of diabetes, and medication use.
Despite its high prevalence, there's a lack of research on constipation management in CKD patients. Non-pharmacological strategies, such as dietary interventions and physical activity, are considered first-line treatment options due to their low cost and fewer side effects compared to laxative drugs.
Additionally, biotics supplementation has shown promising results in improving bowel habits. Gut dysbiosis has been identified as a potential contributor to the pathogenesis of constipation in CKD. Characteristics of gut microbiota in individuals with constipation include lower diversity and abundance of beneficial bacteria and higher abundance of pathogenic bacteria.
Targeted treatment for gut dysbiosis through biotics supplementation may help alleviate constipation symptoms in CKD patients. Further research is needed to improve our understanding of the relationship between gut health and kidney disease management (how to manage chronic kidney disease).
Diagnosis of Constipation in CKD
If you have chronic kidney disease and are experiencing symptoms of constipation, the diagnosis and management process may require attention.
Constipation in CKD can be caused by a combination of factors, including reduced fluid intake, dietary restrictions, medications, and decreased physical activity.
To diagnose constipation in CKD, your healthcare provider will likely start by assessing your symptoms and medical history.
They will inquire about the frequency and consistency of your bowel movements, as well as any associated symptoms like abdominal pain or bloating. It is important to provide a comprehensive overview of your symptoms to help guide the diagnosis.
Physical examination may also be conducted to assess the abdomen for any signs of distension, tenderness, or impacted stool.
Laboratory tests, such as blood tests and urinalysis, may be performed to evaluate kidney function and identify any imbalances or abnormalities that could contribute to constipation.
Your healthcare provider may also consider other diagnostic procedures, such as imaging studies like abdominal X-rays or colonoscopy, if they suspect underlying structural abnormalities or complications.
Once constipation is diagnosed, management strategies can be implemented. This may involve increasing fluid intake, adjusting dietary fiber intake, and promoting physical activity.
Your healthcare provider may also recommend over-the-counter or prescription medications to relieve constipation symptoms and improve bowel movements.
It is important to work closely with your healthcare team to develop an individualized plan that addresses your specific needs and minimizes the impact of constipation on your overall well-being.

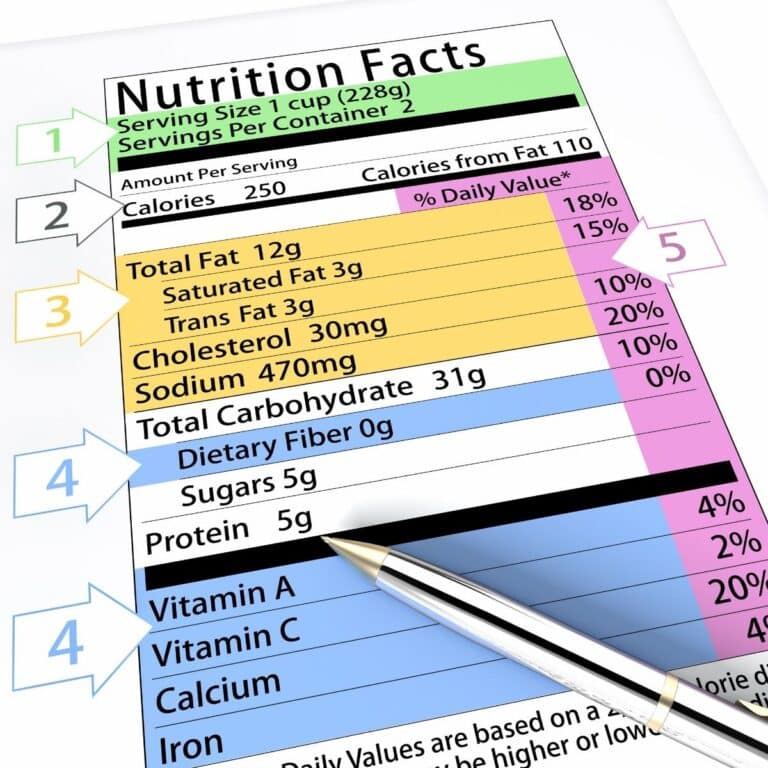
5 Ways On How to Prevent Constipation and Promote Good Gut Health
Activities for preventing constipation and improving gut health are similar. You should do the following in order to help reduce the chances of suffering from constipation as well as creating a healthier gut.
- Eat a well-balanced diet with beans, fresh fruits, and vegetables included.
- Increase your fiber intake. This promotes healthy bowel movements and stimulates the growth of the good gut bacteria. High fiber foods include apples, blueberries, navy beans, pears, and dates.
- Consume prebiotic foods. These foods contain fiber or complex carbs that the body itself cannot digest. The bacteria found in your digestive tract break these down and use them for energy.
- Avoid skipping meals. Eating throughout the day keeps the food moving through your digestive system. If you skip a meal, this process stops, causing your body to retain the wastes longer than it should. This not only causes constipation but can also mess with the healthy balance of gut bacteria.
- Stay hydrated. Getting the recommended amount of 64 ounces (8 cups) of water per day will help keep things moving well through the gut.
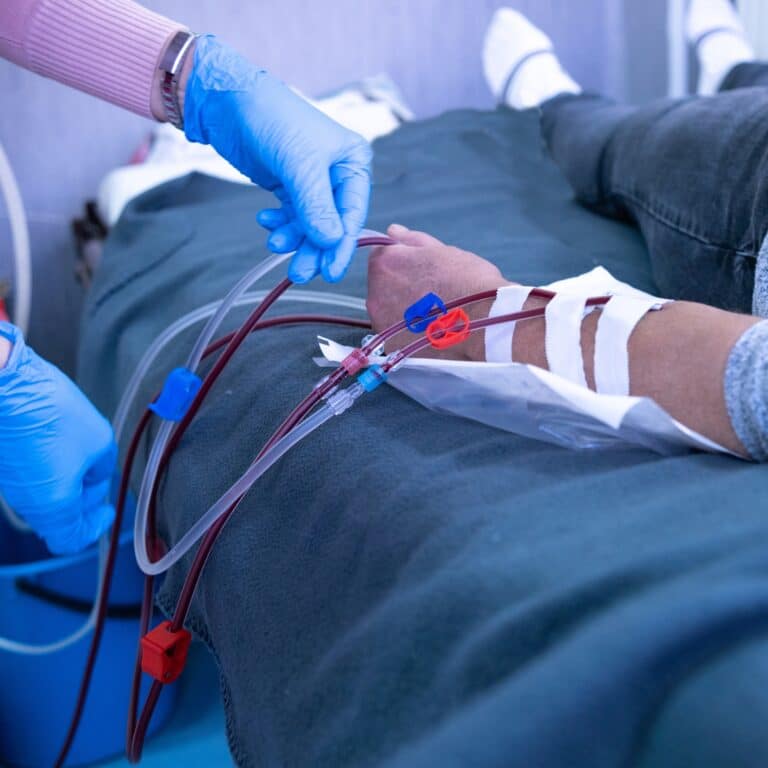
Pharmacologic Approaches to Constipation in CKD
The treatment of constipation in patients with CKD involves various pharmacologic options to alleviate constipation related symptoms and improve bowel movements. Severe constipation in adults can be challenging to manage, especially in patients with constipation-related complications.
Several medications offer therapeutic options to address the presence of constipation and its underlying mechanisms of action. Stool softeners, such as docusate sodium, work by facilitating the incorporation of water into the stool, making it easier to pass. They are commonly used in combination with other therapeutic agents to enhance their efficacy.
Promoting gastrointestinal motility is a key aspect of managing constipation in patients. Prokinetic agents, such as metoclopramide or erythromycin, enhance colonic motility and facilitate stool passage. They are particularly useful in patients with slow transit constipation or reduced colonic motility.
The therapeutic strategy for constipation in CKD patients often involves the use of constipation agents including laxatives.
Osmotic laxatives, such as polyethylene glycol or lactulose, work by drawing water into the colon, softening the stool and promoting bowel movements. Bulk-forming laxatives, such as psyllium husk or methylcellulose, are agents for constipation that increase stool bulk and stimulate peristalsis, aiding in regular bowel movements.
Smooth muscle stimulants, such as bisacodyl or senna, directly target colonic smooth muscles, promoting their contraction and facilitating stool evacuation. These agents are useful in patients with sluggish colonic transit or insufficient muscle activity.
It is important to consider the clinical implications and potential complications associated with constipation agents in CKD patients.
In individuals with impaired kidney function, caution should be exercised when prescribing medications that may alter electrolyte balance or lead to fluid retention. Monitoring kidney function and adjusting doses accordingly is crucial to prevent adverse effects (improving kidney function with diet).
In conclusion, pharmacologic treatment options for constipation in CKD patients involve various mechanisms of action. Stool softeners, prokinetic agents, laxatives, and smooth muscle stimulants are employed to improve gastrointestinal motility and facilitate regular bowel movements.
Careful consideration of individual patient factors and close monitoring are necessary to ensure the safe and effective use of constipation agents in CKD management.
Complications of Constipation in CKD
If you have chronic kidney disease and are experiencing constipation, it is important to be aware of the potential complications, especially bowel disorders that can arise from this condition. Constipation can have significant implications for your health and well-being.
One of the complications of constipation in CKD is the increased risk of developing hemorrhoids. Straining during bowel movements due to constipation can lead to the swelling and inflammation of the blood vessels in the rectal area, resulting in painful hemorrhoids.
Furthermore, constipation can contribute to a condition known as fecal incontinence. When constipation persists, liquid stool may leak around the hardened stool, leading to involuntary bowel movements and potential embarrassment.
Constipation can also worsen gastrointestinal symptoms, such as abdominal pain, bloating, and discomfort. These symptoms can significantly impact your quality of life and overall comfort.
In some cases, chronic constipation can lead to a condition called megacolon. This refers to an enlarged colon that loses its natural muscle tone and becomes unable to propel stool effectively. Megacolon can further exacerbate constipation, leading to more severe symptoms and complications.
Additionally, constipation can affect appetite and nutrient absorption, potentially contributing to malnutrition and electrolyte imbalances, which can further complicate CKD management.
To minimize these complications, it is essential to address constipation promptly. Speak with your healthcare provider to develop an individualized plan that includes appropriate dietary modifications, increased fluid intake, and lifestyle adjustments.
By managing constipation effectively, you can reduce the risk of complications and improve your overall well-being as a CKD patient (exercise for CKD Patients).
FAQs Constipation and CKD
Yes, constipation in CKD patients can potentially lead to other gastrointestinal issues. When constipation persists, it can increase the risk of developing complications such as hemorrhoids, anal fissures, and fecal impaction.
The straining during bowel movements can cause swelling and inflammation of the blood vessels in the rectal area, resulting in painful hemorrhoids. Furthermore, hard and dry stool can lead to the development of anal fissures, which are small tears in the lining of the anus.
Additionally, if constipation becomes severe and prolonged, it can result in fecal impaction, where stool hardens and becomes impacted in the rectum.
These complications can further exacerbate constipation symptoms and cause additional discomfort and pain. It is crucial to address constipation promptly and work with your healthcare provider to develop a management plan to prevent and manage these potential gastrointestinal issues.
To prevent constipation in CKD patients, specific dietary interventions can be beneficial. Increase your dietary fiber intake by including sources such as fruits, vegetables, whole grains, and legumes in your meals and snacks.
Aim for at least 25-30 grams of fiber per day, but be mindful of any dietary restrictions or limitations related to your CKD. Stay well-hydrated by consuming an adequate amount of fluids, primarily water, throughout the day.
Adequate hydration can help soften stool and ease bowel movements. However, be mindful of fluid restrictions that may vary depending on your stage of kidney disease (fluids to hydrate with kidney disorder).
Regularly consume foods rich in natural laxatives, such as prunes or prune juice, which can aid in promoting regularity. Incorporate healthy fats into your diet, like olive oil and avocados, which can lubricate the intestines and facilitate bowel movements.
Consider talking to a renal dietitian who specializes in kidney disease to develop a personalized dietary plan that meets your specific needs. Remember, individual dietary recommendations may vary based on your CKD stage and other health factors, so it's crucial to seek guidance from a healthcare professional.
Yes, there is a link between constipation and an increased risk of infection in CKD patients. When constipation occurs, stool can remain in the intestines for an extended period, providing an environment for bacteria to grow and multiply.
This bacterial overgrowth can potentially lead to infections, such as urinary tract infections (UTIs). Constipation can cause incomplete evacuation of the bowels, increasing the likelihood of fecal contamination and subsequent infections.
It is essential to manage constipation effectively through dietary interventions, adequate hydration, and, if necessary, appropriate medical treatments to minimize the risk of infections and maintain overall health in CKD patients.
Constipation can affect fluid balance in CKD patients. When constipation occurs, it can lead to the retention of stool in the intestines, which can cause an increase in water absorption from the stool back into the body.
This can result in the loss of fluid from the intestinal contents and contribute to fluid imbalance. The increased water absorption (water rich foods) can exacerbate fluid retention in the body, potentially worsening edema and fluid overload.
Managing constipation effectively is important to prevent these complications and maintain fluid balance in CKD patients. Ensuring an adequate fluid intake, incorporating dietary fiber, and following appropriate medical advice can help alleviate constipation and support fluid balance in CKD management.
Surgical options are available for treating chronic constipation, but they should be considered a last resort after trying non-surgical alternatives.
The effectiveness of surgical options varies depending on the specific procedure and individual patient factors. Risks associated with surgery include bleeding, infection, and anesthesia complications.
Recovery time also varies depending on the procedure performed and can range from a few weeks to several months.
Before considering surgery, it's important to explore non-surgical alternatives such as diet modifications, increased fluid intake (fluid restriction diet), fiber supplementation, and physical activity.
Surgery should only be considered if these alternatives have been exhausted or if there are underlying medical conditions that require surgical intervention.
Constipation Is Common, But Don’t Let It Stop You!
Constipation can have a significant impact on kidney health and increase the risk of developing chronic kidney disease. Proper management and prevention of constipation are essential for reducing this risk. This can be achieved through a well-balanced diet, fiber intake, and hydration.
It's crucial to diagnose constipation early in CKD patients and identify any underlying risk factors that may contribute to its development. Addressing these factors with appropriate interventions can improve gut health and reduce the risk of gut-derived uremic toxin accumulation.
Ultimately, taking steps to prevent or manage constipation is an important part of maintaining overall kidney health. This helps to prevent medical complications associated with CKD.