Kidney Failure Meal Plan
No matter what stage of kidney disease you are currently in, you have the potential to effectively halt the progress of your disease and prevent kidney failure.
Yes, you read that correctly -- you can prevent kidney failure. How you can do this starts with a sensible and well thought out meal plan.

Jump to:
- Key Takeaways
- Understanding Kidney Disease
- Nutritional Management Goals
- Appropriate Fat Choices
- Carbohydrate Selection Tips
- Sodium and Portion Control
- Potassium and Phosphorus Balance
- Fluid Management Strategies
- Kidney-Friendly Recipe Ideas
- Adapting Meals to CKD Stages
- Frequently Asked Questions
- Slow Your Progression with a Kidney Failure Meal Plan
Key Takeaways
- A kidney-friendly eating plan helps protect your kidneys from more damage.
- It helps manage kidney disease and slow down kidney damage.
- It prevents certain minerals from building up in your body.
- Following a kidney-friendly eating plan involves eating the right amount and types of protein, choosing the right types of fat, choosing whole grain carbohydrates, limiting unhealthy carbs, and practicing portion control and mindful eating.
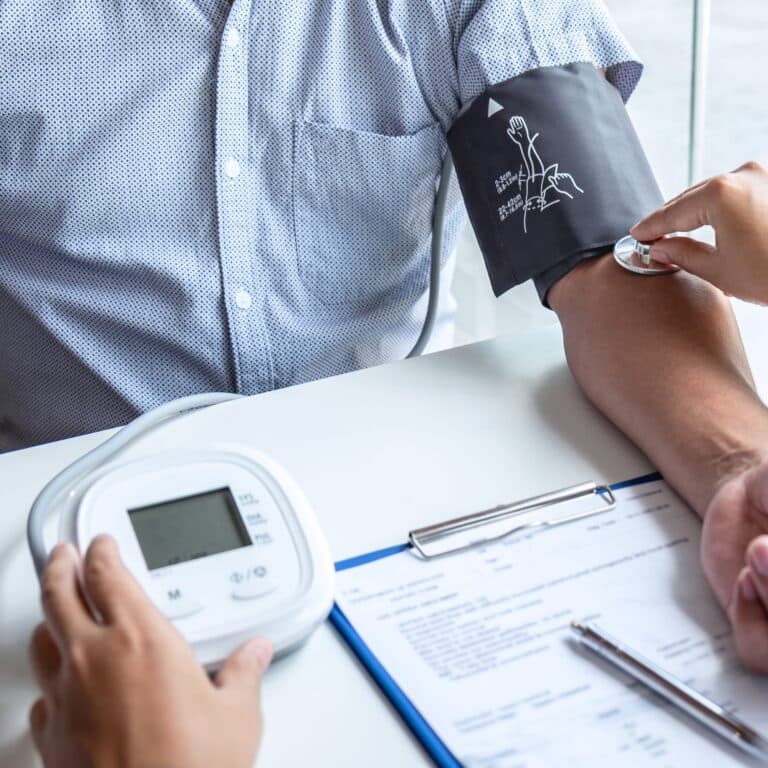
Understanding Kidney Disease
Let's talk about an overview of kidney disease and its intricate interplay with diet. Understanding the nuances of kidney function and the role nutrition plays in disease progression is vital. Exploring how dietary choices influence kidney health, you are able to navigate the complexities of managing kidney disease through tailored nutrition.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Kidney Disease Progression
Chronic Kidney Disease (CKD) is a long-term condition characterized by a gradual loss of kidney function. It's often silent in early stages, making early detection challenging. CKD progresses through five stages, determined by glomerular filtration rate (GFR), a measure of kidney efficiency. In the initial stages (1 and 2), kidney function is mildly reduced, and patients may not exhibit noticeable symptoms.
However, subtle signs like fatigue or changes in urine might occur. As CKD advances to stages 3 and 4, symptoms become more pronounced, including swelling, high blood pressure, anemia, and bone disorders. Kidney function continues to deteriorate, leading to an accumulation of waste products in the body. The final stage, stage 5, is end-stage renal disease (ESRD), where kidney function is critically low, and dialysis or a kidney transplant becomes necessary.
CKD is primarily caused by diabetes and hypertension, and its progression can be slowed with proper management including medication, lifestyle changes, and dietary adjustments.
Dietary Restrictions Importance
Dietary restrictions play a pivotal role in managing Chronic Kidney Disease, aiming to alleviate strain on compromised kidneys and mitigate complications. Limiting specific nutrients like sodium, potassium, phosphorus, and protein helps regulate blood pressure, fluid balance, and minimize waste buildup in the body.
High sodium intake elevates blood pressure, while excess potassium or phosphorus can lead to dangerous imbalances, impacting heart and bone health. Controlling protein intake reduces the kidneys' workload, managing waste production without overburdening renal function. Tailoring the diet to individual kidney function and disease stage is crucial, as dietary adjustments evolve with disease progression.
Adhering to prescribed dietary restrictions slows CKD progression, reduces the risk of complications like cardiovascular disease and bone disorders, and significantly improves the overall quality of life for individuals navigating CKD. Regular monitoring and guidance from healthcare providers optimize dietary plans for effective kidney disease management.
Nutritional Management Goals
Your nutritional management goals are crucial in combating kidney failure. You'll need to balance essential minerals and optimize your protein intake, always considering your unique health needs.
Achieve Mineral Balance
Achieving mineral balance in Chronic Kidney Disease is critical for maintaining overall health. Imbalances in minerals like phosphorus, potassium, and calcium significantly impact kidney function and overall well-being.
Elevated phosphorus levels, common in CKD, can lead to bone and heart complications, contributing to cardiovascular disease. Potassium imbalances affect heart rhythm, potentially causing life-threatening arrhythmias. Calcium regulation is crucial for bone health and muscle function. Managing mineral balance through dietary modifications, medication, and sometimes, phosphate binders, is pivotal in CKD management.
Striking the right balance ensures optimal kidney function, reduces the risk of complications such as bone disease, cardiovascular issues, and electrolyte imbalances, enhancing the quality of life for individuals navigating CKD. Regular monitoring and tailored interventions help maintain mineral balance, mitigating complications associated with imbalances in CKD.
Optimize Protein Intake
Optimized protein intake in Chronic Kidney Disease varies depending on the stage of the disease, reflecting a balance between nutritional needs and kidney health. In the early stages of CKD (stages 1-3), protein intake is often maintained at normal levels, aligning with general dietary recommendations, to ensure adequate nutrition and muscle maintenance.
However, as CKD progresses to more advanced stages (stages 4-5), the focus shifts towards reducing protein intake. This adjustment helps decrease the kidneys' workload and slow the progression of kidney damage. The recommended protein intake in these stages typically ranges from 0.6 to 0.8 grams per kilogram of body weight per day, tailored to individual needs and nutritional status.
In cases of dialysis, protein needs increase to compensate for protein loss during treatment. Patients are advised to consume higher amounts, often 1.2 grams per kilogram of body weight or more, to maintain muscle mass and overall health. Dietitians play a crucial role in individualizing dietary plans, ensuring patients with CKD receive the right amount of protein at each stage of the disease.
Regular monitoring and adjustments based on the progression of CKD, nutritional status, and treatment modalities are essential for optimal dietary management.
Appropriate Fat Choices
When managing your kidney failure meal plan, it's essential to choose fats wisely; focus on incorporating healthy fat sources like olive oil and avocados.
You should limit saturated fats found in foods such as butter, cheese, and fatty cuts of meat, as they can contribute to heart disease, which often accompanies kidney issues.
Your dietitian can help you tailor fat choices to your specific health needs, ensuring your diet supports both kidney function and overall well-being.
Healthy Fat Sources
In your journey to manage kidney disease, choosing healthy fats is crucial for your meal plan. Understanding the benefits of fats and incorporating healthy fats into your diet can significantly enhance your nutritional status while also being kind to your kidneys.
Cooking with healthy fats not only adds flavor but also provides essential fatty acids and helps with the absorption of fat-soluble vitamins.
Here are some fat alternatives that can be included:
- Olive oil: a heart-healthy monounsaturated fat
- Avocado: rich in beneficial fats and a versatile ingredient
- Ground flaxseed: a good source of omega-3 fatty acids
- Soft, non-hydrogenated margarines: low in trans and saturated fats
These options offer a balance of taste and health benefits, making them ideal for your condition-specific needs.
Limit Saturated Fats
You'll need to limit saturated fats in your diet to keep your kidneys healthy and functioning properly. Saturated fat sources, like red meat and full-fat dairy products, can have a significant impact on kidney health. Reducing saturated fat intake is crucial in managing your condition. Instead, focus on incorporating healthy fats into your diet, which can support kidney function without the added stress of saturated fats.
Alternatives to saturated fats include:
| Saturated Fat Sources | Healthier Alternatives |
| Butter | Olive oil |
| Fatty cuts of meat | Lean poultry |
| Full-fat dairy | Plant-based milks |
These substitutions not only cater to your kidney health but also align with a desire to nurture and care for your body.
Carbohydrate Selection Tips
When managing kidney failure, it's essential to select carbohydrates carefully to maintain your health. Opt for low glycemic index options, which help control blood sugar levels and reduce strain on your kidneys.
Including whole grains in your diet can provide additional benefits, such as essential nutrients and fiber that support overall well-being.
Low Glycemic Index Choices
Selecting carbohydrates with a low glycemic index is essential for stabilizing your blood sugar levels and protecting your kidney function. Understanding the glycemic index helps in managing blood sugar levels effectively.
The benefits of low glycemic foods are numerous, especially for kidney health, as they prevent spikes in glucose that can stress your kidneys. Be aware of the impact of high glycemic foods on kidney health and focus on incorporating low glycemic choices into your meal plan.
Consider these options:
- Whole grain breads instead of white bread
- Steel-cut oats over instant oatmeal
- Legumes like lentils and chickpeas
- Non-starchy vegetables such as leafy greens and peppers
Tailor your diet to include these nutrient-dense, low glycemic foods to serve your body's needs and support kidney function.
Whole Grain Benefits
Transitioning from low glycemic index choices, it's essential to zero in on the benefits of whole grains as part of your kidney-friendly carbohydrate selection. Whole grains are packed with fiber, which can help in maintaining bowel health and controlling blood sugar levels. Including whole grain foods in your diet means you're also getting more nutrients and healthy fat sources, contributing to overall well-being.
When managing kidney disease, it's crucial to ensure optimal protein amounts in your meals. Whole grains can be a complementary part of this balance, providing necessary energy without overburdening your kidneys. Remember to focus on portion control and limiting fluid intake, as whole grains can contribute to your daily fluid consumption.
Selecting whole grains is a proactive step in sustaining your kidney health and managing CKD effectively.
Sodium and Portion Control
Managing your sodium intake is crucial to prevent fluid retention and control blood pressure, which can be especially challenging with kidney failure.
You'll need to be mindful of portion sizes to ensure you're consuming nutrients without overloading your kidneys.
Limit Salt Intake
Limiting salt intake is crucial in a kidney diet due to its impact on blood pressure and kidney health. In Chronic Kidney Disease, kidneys lose the ability to filter excess sodium effectively, leading to fluid retention, hypertension, and further kidney damage. High blood pressure exacerbates kidney deterioration, making sodium restriction vital for slowing CKD progression.
To limit sodium intake in a CKD diet, it’s important to:
- Avoid high-sodium foods like processed meats, canned soups, fast foods, and snacks.
- Read food labels carefully, choosing products with lower sodium content.
- Use herbs and spices instead of salt for seasoning.
- Prepare meals at home, where sodium can be controlled.
- Be cautious with condiments and sauces, which often contain high sodium levels.
- Limit use of salt substitutes, as they may contain potassium, another mineral that needs monitoring in CKD.
Consistently following these guidelines can help manage blood pressure and fluid balance, reducing strain on the kidneys and supporting overall health in CKD management.
Practice Mindful Portions
Mindful portion control is essential in limiting sodium intake, especially for individuals with kidney issues or hypertension. It involves being aware of the sodium content in foods and adjusting serving sizes accordingly. Here are key strategies:
- Read Labels: Understand the sodium content per serving listed on food labels. This awareness helps in adjusting portion sizes to keep within recommended limits.
- Cook at Home: Home-cooked meals allow for complete control over ingredients and sodium levels. Use fresh, unprocessed ingredients as much as possible.
- Measure Ingredients: Use measuring spoons for added salt and high-sodium condiments. This helps avoid unintentional overuse.
- Use Fresh or Frozen Produce: Opt for fresh or frozen fruits and vegetables over canned varieties, which often contain added sodium.
- Portion Size Awareness: Serve food in smaller plates to naturally encourage smaller portions.
- Limit Processed Foods: Many processed foods are high in sodium. Reducing their consumption is key to controlling sodium intake.
- Season Creatively: Experiment with herbs, spices, and salt-free seasoning blends to enhance flavor without adding sodium.
By incorporating these practices, individuals can significantly reduce their sodium intake, which is beneficial for both kidney health and overall well-being.
Potassium and Phosphorus Balance
Balancing your potassium and phosphorus intake is crucial for managing kidney disease, as your kidneys can struggle to maintain proper levels of these minerals.
You'll need to adjust your diet to include foods that are lower in potassium and phosphorus while still meeting your nutritional needs.
Working closely with your dietitian, you can create a meal plan that supports your kidney health without compromising on flavor or variety.
Managing Mineral Levels
Managing mineral levels, particularly potassium and phosphorus, is a crucial aspect of a renal diet for those with kidney disease. Kidneys regulate these minerals; however, compromised kidney function can lead to imbalances, posing health risks.
Potassium: High levels can cause cardiac issues. Opt for lower potassium foods like apples, berries, and green beans, and limit high-potassium items like bananas, oranges, and potatoes. Leaching vegetables can also reduce their potassium content.
Phosphorus: Excess phosphorus can weaken bones and damage blood vessels. It's abundant in dairy products, nuts, and whole grains. Patients should opt for limited amounts of these foods and avoid phosphorus additives often found in processed foods.
Careful monitoring and portion control are essential. Consulting a dietitian who specializes in kidney disease can provide personalized guidance for managing these mineral levels effectively within a renal diet, ensuring both dietary satisfaction and health benefits.
Dietary Adjustment Strategies
In chronic kidney disease, managing dietary potassium and phosphorus is vital to prevent complications. Here are strategies to adjust these levels:
- Potassium Control: Since kidneys in CKD can't effectively eliminate excess potassium, leading to hyperkalemia and heart issues, it's important to choose lower potassium foods. Include apples, carrots, green beans, and white bread while avoiding high-potassium foods like bananas, oranges, and potatoes. Cooking methods like boiling can help reduce potassium in vegetables.
- Phosphorus Management: As CKD progresses, phosphorus can accumulate, leading to bone and cardiovascular problems. Limit intake of dairy, nuts, seeds, and whole grains, which are high in phosphorus. Beware of phosphorus additives in processed foods and colas. Read labels to identify additives like 'phosphates'.
- Portion Control and Balance: Consuming smaller portions and balancing your meals can help manage these minerals.
- Consultation and Monitoring: Regular blood tests and consulting a dietitian or nephrologist are essential for personalized dietary adjustments.
These dietary strategies, alongside medications to control potassium and phosphorus levels, are integral in managing CKD.

Fluid Management Strategies
As you manage kidney failure, it's crucial to monitor and limit your fluid intake to reduce the strain on your kidneys.
You'll need to keep a close eye on all beverages you drink throughout the day, ensuring they align with your dietitian's recommendations.
This tailored approach helps prevent fluid overload, which can lead to complications in your condition.
Limiting Fluid Intake
In kidney failure, a crucial aspect of the meal plan involves limiting fluid intake. When kidneys are impaired, they lose the ability to effectively balance fluid levels, leading to fluid retention and swelling (edema), high blood pressure, and heart strain. Excess fluid can accumulate in the lungs, causing shortness of breath, and may exacerbate heart conditions.
A restricted fluid intake helps prevent these complications. This includes not only beverages but also foods with high water content, like soups, ice cream, and certain fruits and vegetables. Patients are typically advised to measure and record their fluid intake, including small amounts consumed with medication.
Balancing fluid intake requires a delicate approach, considering the individual's urine output, residual kidney function, and dialysis schedule, if applicable. Healthcare professionals provide personalized guidance on the exact fluid restrictions. Adhering to these guidelines is a key component of managing symptoms and improving the quality of life in kidney failure.
Monitoring Daily Beverages
Monitoring daily beverage intake is vital for patients with Chronic Kidney Disease, especially when fluid restrictions are necessary. This involves being mindful of all fluids consumed throughout the day, not just water. Beverages like tea, coffee, soft drinks, and even liquid foods such as soups or gelatin count towards the fluid quota.
Patients should begin by understanding their individual fluid allowance, usually prescribed by a healthcare provider. Keeping a daily fluid diary is an effective way to track intake. This diary should include every liquid consumed, even small sips, and the quantity should be accurately measured. Using specific-sized containers can help in estimating the amount consumed more easily.
Additionally, patients can employ strategies to manage thirst, like sucking on ice chips or a lemon wedge, as these contribute less to fluid intake than drinking a glass of water. It's also important to avoid salty or spicy foods that can increase thirst. Regular consultation with a healthcare provider helps in adjusting the fluid allowance based on changes in health status or kidney function.
Kidney-Friendly Recipe Ideas
You'll need to focus on low-potassium food options to keep your kidneys from working too hard.
Phosphorus-controlled meal suggestions can help prevent the mineral from accumulating in your body, which is crucial for your health.
Let's explore some kidney-friendly recipes that are both nutritious and tailored to your dietary needs.
- Herb-Grilled Chicken: Marinate chicken breasts in a blend of olive oil, garlic, and herbs like rosemary and thyme. Grill or bake until cooked through. Herbs enhance flavor without adding sodium. Eat with our peas and carrots recipe.
- Quinoa Salad: Combine cooked quinoa with diced cucumbers, bell peppers, and parsley. Dress with lemon juice and a touch of olive oil for a refreshing, low-phosphorus salad.
- Vegetable Stir-Fry: Use kidney-friendly vegetables like green beans, bell peppers, and carrots. Cook in a low-sodium sauce made with low-sodium soy sauce, ginger, and garlic. Serve over rice or noodles. You can also use our roasted red bell pepper sauce that is low in sodium, potassium and phosphorus.
- Baked Fish Fillet: Season fish fillets with herbs, lemon juice, and a sprinkle of dill. Bake until flaky for a low-fat, low-phosphorus protein source.
- Low-Potassium Fruit Salad: Create a refreshing fruit salad with low-potassium fruits like apples, berries, and pineapple. Avoid high-potassium fruits like bananas or oranges.
- Cauliflower Mashed "Potatoes": Steam cauliflower and mash with a touch of low-sodium chicken broth, garlic, and a sprinkle of herbs for a potassium-friendly alternative to mashed potatoes.
- Homemade Vegetable Soup: Use kidney-friendly vegetables like cabbage, onions, and zucchini. Flavor with herbs and spices instead of salt.
These recipes focus on fresh, whole ingredients and use herbs and spices to enhance flavor without relying on salt or high-potassium ingredients. It's essential to consult a dietitian or healthcare provider for personalized meal planning based on individual dietary restrictions and needs in kidney failure management.
Adapting Meals to CKD Stages
As your CKD progresses through its stages, your meal plan needs to adapt to manage nutrients more precisely. You'll work closely with a dietitian to tweak your diet, ensuring it's aligned with your current health needs and kidney function.
This stage-specific approach helps prevent the buildup of minerals and maintains your body's balance, protecting your kidneys from further damage.
Stage-specific Dietary Adjustments
Dietary adjustments in Chronic Kidney Disease vary across stages, emphasizing the evolving needs of individuals as kidney function declines:
- Early Stages (1-3): Focus on maintaining a balanced diet with controlled sodium, phosphorus, and protein. Limiting processed foods is crucial.
- Intermediate Stages (4-5): As kidney function declines further, restrict protein intake to reduce the kidneys' workload. Monitor phosphorus and potassium levels more closely, reducing high-phosphorus foods and high-potassium fruits.
- End-Stage Renal Disease (ESRD): For those on dialysis, protein needs may increase. Sodium and fluid restrictions become more critical due to compromised fluid balance.
- Post-Transplant: Post-kidney transplant, dietary restrictions may ease, but medications and overall health considerations persist. Focus on a well-balanced, nutrient-rich diet to support overall health.
These stage-specific adjustments aim to manage complications and support overall health throughout the progression of CKD, underscoring the importance of personalized dietary guidance from healthcare professionals.
Progressive Nutrient Management
Nutrient management in Chronic Kidney Disease evolves through its stages, reflecting the kidney's diminishing ability to regulate various substances:
- Early Stages (1-2): Emphasis is on a balanced, heart-healthy diet. Controlling blood pressure and blood sugar is key, with moderate sodium and protein intake.
- Moderate Stage (3): Increased focus on reducing sodium, phosphorus, and potassium intake to prevent fluid retention, heart issues, and bone disease. Protein intake may need slight adjustment.
- Advanced Stages (4-5): Restricting phosphorus becomes crucial to prevent bone disease. Potassium levels are closely monitored to avoid heart issues. Protein intake is more restricted to lessen kidney burden. Sodium and fluid restrictions become stringent to manage swelling and blood pressure.
- Dialysis Stage: Dialysis alters nutrient needs. Higher protein is often required, while potassium, phosphorus, and sodium must be carefully managed due to reduced kidney function.
- Post-Transplant: Nutrient needs may normalize somewhat, but a balanced diet remains essential, considering any ongoing medications.
Throughout all stages, individualized dietary plans by healthcare professionals are vital for optimal management, as CKD's complexity demands tailored approaches.
Frequently Asked Questions
Managing food cravings while adhering to a kidney-friendly diet involves strategic choices. Opt for healthier alternatives to satisfy cravings, like frozen grapes instead of ice cream or baked sweet potato fries instead of regular fries. Portion control is key; indulge in small servings occasionally. Distract cravings by staying busy, practicing mindfulness, or enjoying herbal teas. Planning meals in advance helps control cravings by ensuring nutrient-dense, satisfying options are readily available, reducing temptation for non-kidney-friendly foods.
When traveling or away for extended periods, plan ahead by researching local eateries for kidney-friendly options. Pack non-perishable snacks like nuts, rice cakes, or dried fruits. Consider portable, low-sodium meals such as salads with protein or sandwiches made with kidney-friendly ingredients. Communicate dietary needs to accommodations or restaurants. Carry prescribed medications and a list of dietary restrictions. If possible, bring a small cooler for perishable items. Staying hydrated with water helps maintain kidney health while on the go. Consulting a dietitian for personalized travel tips ensures adherence to a kidney-friendly meal plan away from home.
Involve your family by incorporating kidney-friendly meals with customizable elements. Prepare a base meal everyone enjoys, then add separate components like sauces, cheeses, or seasonings for variety. Educate them about your dietary restrictions, encouraging understanding and support. Plan meals with shared sides like vegetables or grains, allowing individual additions. Experiment with flavorful herbs and spices instead of salt, benefitting everyone’s health. Communicate openly about your dietary needs while ensuring everyone can enjoy meals together, accommodating both your kidney-friendly choices and their preferences.
Slow Your Progression with a Kidney Failure Meal Plan
A sensible meal plan can help you stick to a healthy, kidney safe diet, which in turn can help you avoid kidney failure. Of course, whenever you have questions or concerns or are making changes to your diet, you should speak to your physicians first.
You want to make sure you are eating the healthiest diet for your situation, so you too can avoid kidney failure.