Managing Your Kidney Disease
If you were only recently diagnosed with renal disease, managing your new dietary recommendations and restrictions can seem like a difficult task. At first the changes might seem very restrictive or unwelcome, but you will get used to your new way of life and once the diet changes start sinking in, you will notice that you feel better too.
This guide will help you understand what's happening to your body and what steps you can take to maintain or improve your kidney health.
Jump to:
- Key Takeaways
- Understanding the Role of Blood Pressure and Diabetes in Kidney Disease
- Key Steps in Monitoring Your Kidney Health
- Effective Preparation for Healthcare Visits
- The Impact of Medications on Kidney Health
- Adopting Lifestyle Changes for Better Kidney Health
- The Crucial Role of Diet Control in Managing Kidney Disease
- The Challenge of Resistance and the Power of Embracing Change
- The Importance of Seeking Support From Loved Ones
- The Importance of Following Medical Advice in Managing Kidney Disease
- Frequently Asked Questions
- Chronic Kidney Disease Can Be Managed
Key Takeaways
- High blood pressure and diabetes are major factors that can impact kidney health and lead to kidney damage.
- Regular monitoring of kidney function through tests is important for understanding the type and extent of the disease.
- Preparation for healthcare visits should involve creating a list of questions, discussing disease progression and treatment options, and considering alternatives to dialysis.
- Implementing healthy lifestyle habits such as reducing processed foods, incorporating kidney-friendly recipes, staying hydrated, exercising regularly, and managing stress can help support kidney health.
Understanding the Role of Blood Pressure and Diabetes in Kidney Disease
Understanding the role of blood pressure and diabetes in kidney disease is essential for preserving renal health. These two factors, often intertwined, are leading causes of kidney impairment. High blood pressure, or hypertension, places excessive strain on delicate kidney filters, while diabetes can harm blood vessels and nephrons. This section delves into how these conditions contribute to chronic kidney disease (CKD).
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Blood Pressure's Impact
Hypertension, commonly known as high blood pressure, is a significant contributor to the development and progression of chronic kidney disease. The kidneys play a pivotal role in regulating blood pressure, making them highly susceptible to its adverse effects.
Persistent high blood pressure damages the delicate blood vessels in the kidneys, particularly the small arterioles and capillaries. Over time, this vascular injury disrupts the kidneys' ability to filter waste and excess fluids effectively. The result is a condition known as hypertensive nephropathy, a specific form of CKD directly caused by hypertension.
As the kidney's filtration capacity diminishes, waste products accumulate in the bloodstream, leading to further increases in blood pressure. This creates a vicious cycle where hypertension worsens kidney function, and declining kidney function exacerbates hypertension.
Untreated or poorly managed hypertension significantly elevates the risk of developing CKD. Therefore, early detection, lifestyle modifications, and antihypertensive medications are crucial in preventing and managing hypertension-related kidney disease. Regular blood pressure monitoring and adherence to medical advice can help mitigate these risks and preserve kidney health.
Diabetes and Kidney Disease
Diabetes is another major precursor to chronic kidney disease and is among the leading causes of CKD worldwide. The connection between diabetes and CKD is primarily attributed to the prolonged impact of high blood sugar levels on the kidneys.
In diabetes, persistently elevated blood glucose levels can damage the small blood vessels in the kidneys, known as nephrons, and their filtering units. This damage disrupts the kidney's ability to effectively remove waste and excess fluids from the body.
Over time, kidney function deteriorates, leading to the development of diabetic nephropathy or diabetic kidney disease, a specific type of CKD directly caused by diabetes. Initially, individuals with diabetic nephropathy may experience microalbuminuria, a condition characterized by the presence of small amounts of protein in the urine.
As it progresses, kidney function further declines, ultimately resulting in end-stage renal disease (ESRD) if left untreated.
Effective management of diabetes through blood sugar control, lifestyle modifications, and medications can significantly reduce the risk of diabetic nephropathy and slow its progression. Regular monitoring of kidney function through blood and urine tests is essential for early detection and intervention.
Key Steps in Monitoring Your Kidney Health
Maintaining kidney health is crucial for overall well-being, and routine kidney function tests play a pivotal role in achieving this goal. One of the key measures is the calculation of Glomerular Filtration Rate (GFR), which provides insights into how efficiently the kidneys are filtering waste from the blood.
This section delves into the importance of these tests and the calculation of GFR, offering essential information on monitoring kidney function and identifying potential issues before they escalate. Understanding these tests empowers individuals to take proactive steps in preserving their kidney health and preventing the progression of kidney disease.
Regular Kidney Function Tests
Monitoring kidney health through routine tests is essential, helping detect issues early and prevent kidney disease progression. Kidney function tests assess how effectively the kidneys filter waste and maintain vital functions.
- Glomerular Filtration Rate (GFR): This calculation estimates the kidneys' filtration rate and is a key indicator of overall kidney function. A lower GFR may signal kidney impairment.
- Serum Creatinine: Elevated levels can indicate kidney problems as creatinine is a waste product excreted by the kidneys.
- Blood Urea Nitrogen (BUN): High BUN levels suggest poor kidney function, as urea is a waste product excreted by the kidneys.
- Urine Tests: These assess protein, blood, and other substances in the urine, providing insights into kidney function and possible issues like proteinuria or hematuria.
- Electrolyte Levels: Imbalances can point to kidney dysfunction.
- Imaging: Ultrasounds or CT scans can detect structural abnormalities.
- Biopsy: In some cases, a tissue sample for kidney biopsy may be needed for diagnosis of kidney disease.
Regular monitoring helps manage kidney health, especially for those at risk due to conditions like hypertension or diabetes, ensuring timely intervention and a higher chance of preserving kidney function.
GFR Levels
The Glomerular Filtration Rate (GFR) is a crucial measure of kidney function, indicating how well the kidneys are filtering waste from the blood. In individuals with healthy kidneys, a GFR typically ranges from 90 to 120 milliliters per minute per 1.73 square meters (mL/min/1.73m²). However, GFR levels decline with age, and slight variations can occur due to factors like muscle mass and hydration.
In the context of Chronic Kidney Disease (CKD), GFR levels take on even greater significance. CKD is categorized into stages based on GFR:
- Stage 1 (GFR > 90 mL/min/1.73m²): Kidney damage with normal or increased GFR.
- Stage 2 (GFR 60-89 mL/min/1.73m²): Mild reduction in kidney function.
- Stage 3 (GFR 30-59 mL/min/1.73m²): Moderate reduction.
- Stage 4 (GFR 15-29 mL/min/1.73m²): Severe reduction.
- Stage 5 (GFR < 15 mL/min/1.73m²): Kidney failure or End Stage Kidney Disease
GFR levels serve as a critical marker for CKD progression. A lower GFR indicates reduced kidney function, which can worsen over time. At stage 5, kidney failure is already evident and the patient may require hemodialysis, peritoneal dialysis, or kidney transplant.
Regular monitoring of GFR is vital to track CKD development, initiate appropriate interventions, and potentially slow down the progression to preserve kidney function.
Effective Preparation for Healthcare Visits
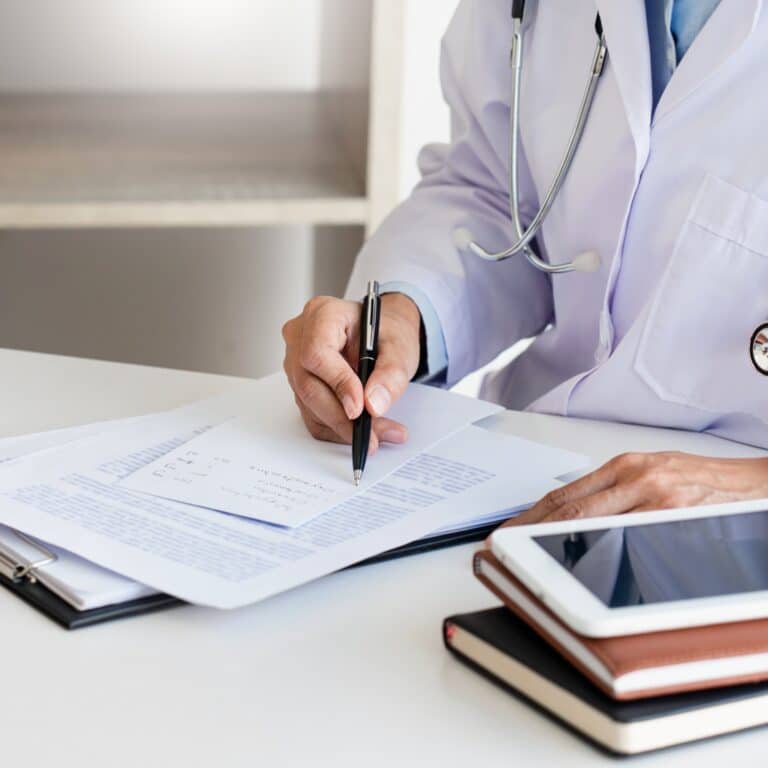
Preparing for healthcare visits is a proactive step in ensuring you receive the best care possible, especially when managing chronic conditions like kidney disease. Effective preparation involves more than just showing up; it's about being informed and engaged in your healthcare journey.
In this section, we'll explore strategies for preparing for healthcare visits, including the importance of having a list of questions ready to ask your doctor and involving support persons in your care. These steps can enhance communication, empower you as a patient, and contribute to better health outcomes.
Question List Creation
Being prepared with questions for your kidney specialist during a healthcare visit is crucial, especially when dealing with a diagnosis like kidney disease. It empowers you to actively participate in your healthcare journey, gain a deeper understanding of your condition, and make informed decisions. Sample questions for someone newly diagnosed with kidney disease might include:
- "Can you explain my kidney disease and its stage in simpler terms?"
- "What are the potential causes or risk factors specific to my case?"
- "What lifestyle changes, like diet and exercise, should I consider?"
- "Are there any medications I need to take, and what are their potential side effects?"
- "How often should I have kidney function tests, and what should I expect from these tests?"
- "Can you recommend any support groups or resources for people with kidney disease?"
Being prepared with such questions fosters a constructive doctor-patient dialogue, ensures your concerns are addressed, and aids in developing a personalized care plan.
Support Person Involvement
Having a strong support network or a dedicated support person involved in your care when you have Chronic Kidney Disease is important. CKD can be physically and emotionally taxing, and having someone to lean on can make a world of difference. They offer emotional support during challenging times, accompany you to medical appointments, help you remember vital information, and provide practical assistance in adhering to dietary and medication plans.
Furthermore, they can serve as advocates for your healthcare needs, ensuring that you receive the best care possible. Whether it's a family member, friend, or support group, their presence enhances your overall well-being, easing the burden of CKD management and improving your quality of life. Having that dependable support system can positively impact your journey toward kidney health.
The Impact of Medications on Kidney Health
Medications play a pivotal role in managing Chronic Kidney Disease and its associated complications. However, not all medications are kidney-friendly, and some can pose significant risks. In this section, we'll explore the impact of medications on kidney health, both the vital role they play in CKD management and the potential harm they can cause.
We'll delve into the importance of medication management, with a focus on harmful substances like nonsteroidal anti-inflammatory drugs (NSAIDs), and how making informed choices about medications can significantly influence your kidney health.
NSAIDs and Kidney Damage
Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used for pain relief and reducing inflammation, but they can be especially harmful to kidney health, particularly for individuals with kidney disease.
NSAIDs work by inhibiting enzymes that produce substances involved in pain and inflammation. Unfortunately, this inhibition can lead to decreased blood flow to the kidneys, potentially causing acute kidney injury or worsening pre-existing kidney conditions.
Moreover, NSAIDs can disrupt the delicate balance of electrolytes and fluids in the body, which is crucial for proper kidney function. For those with kidney disease, the risk of kidney damage is heightened because their kidneys already struggle to filter waste and maintain equilibrium.
It's essential for individuals with kidney disease to avoid NSAIDs and opt for safer pain management alternatives under the guidance of their health care providers to protect their kidney health.
Other Medications Harmful To Kidneys
Beyond NSAIDs, several other drugs pose risks to kidney health, particularly for individuals with chronic kidney disease:
- Certain Antibiotics: Aminoglycoside antibiotics like gentamicin and tobramycin can be nephrotoxic and require careful dose adjustments for people with kidney disease.
- Antiviral Medications: Some antiviral drugs, including acyclovir and tenofovir, can affect kidney function and demand dose modifications for CKD individuals.
- Antifungal Agents: Medications like amphotericin B, used to treat severe fungal infections, have the potential to harm the kidneys and necessitate cautious use.
- ACE Inhibitors and ARBs: These blood pressure medications can influence kidney function and electrolyte balance, necessitating monitoring.
- Contrast Agents: Contrast dyes used in medical imaging tests can stress the kidneys and require careful consideration in CKD patients.
Careful medication selection and frequent kidney function monitoring are vital to safeguard kidney health in CKD patients. Consulting with healthcare providers helps in choosing medications with minimal kidney-related risks.
Medication Management Importance
The management of chronic kidney disease often involves a combination of medications to address various aspects of the condition. Here are some common medications used and their importance:
- ACE Inhibitors and ARBs: These medications help control blood pressure and reduce proteinuria (excessive protein in the urine), slowing the progression of CKD and protecting the kidneys.
- Diuretics: They help remove excess fluid and manage blood pressure, which is crucial in CKD, where fluid and blood pressure control is vital.
- Phosphate Binders: These drugs are essential to control high phosphorus levels in CKD patients, preserving bone health and preventing cardiovascular complications.
- Erythropoiesis-Stimulating Agents (ESAs): ESAs stimulate red blood cell production, addressing anemia common in CKD patients, improving overall quality of life.
- Iron Supplements: Often used in conjunction with ESAs, iron supplements help correct iron deficiency anemia, a prevalent issue in CKD.
- Statins: These drugs help manage cholesterol levels, reducing the risk of cardiovascular disease, a significant concern for CKD patients.
Medications play a crucial role in the comprehensive management of CKD, addressing not only kidney-related issues but also associated complications to enhance patients' well-being and slow disease progression. Regular monitoring and adherence to prescribed regimens are essential.
Adopting Lifestyle Changes for Better Kidney Health
Achieving better kidney health is not solely reliant on medications; lifestyle changes play a crucial role. In this section, we delve into essential modifications that individuals with chronic kidney disease can adopt to enhance their well-being.
From adopting a kidney-friendly diet to incorporating regular exercise, these lifestyle changes are integral to managing CKD effectively and improving overall quality of life. Embracing these adjustments empowers individuals to take an active role in preserving kidney function and mitigating complications associated with this condition.
Implementing Healthy Dietary Habits
Implementing healthy dietary habits is paramount for individuals with chronic kidney disease to manage their condition effectively. A kidney-friendly diet aims to reduce the burden on compromised kidneys while providing essential nutrients.
Key principles include controlling protein intake to lessen the workload on kidneys, limiting sodium to manage blood pressure, and monitoring phosphorus and potassium levels. Emphasizing fresh fruits and vegetables while avoiding processed foods is vital.
Consulting a registered dietitian is essential for personalized meal planning, as dietary restrictions vary based on CKD stage. Patients must adhere to dietary recommendations and monitor their fluid intake and weight. A well-balanced, kidney-conscious diet supports overall health, slows CKD progression, and reduces the risk of complications.
Exercise's Role in Management
Regular exercise plays a vital role in the management of chronic kidney disease. While CKD can pose certain challenges, maintaining an active lifestyle offers numerous benefits for kidney health and overall well-being.
Exercise helps improve cardiovascular health, control blood pressure, and manage diabetes, all of which are critical for CKD patients. It also assists in maintaining a healthy weight, which can reduce the risk of kidney disease progression.
Engaging in physical activity can boost energy levels, reduce symptoms like fatigue, and improve mental health, enhancing the quality of life for CKD patients. Exercise also promotes better sleep and helps combat depression and anxiety, which are common among those with chronic conditions.
However, it's essential for CKD patients to consult their healthcare providers before starting any exercise regimen, as individual limitations and considerations may apply. Exercise plans should be tailored to a patient's specific condition and capabilities, with a focus on low-impact activities like walking, swimming, or gentle yoga.
Regular exercise, when done safely and under professional guidance, can be a valuable tool in managing CKD and improving overall health.
The Crucial Role of Diet Control in Managing Kidney Disease
For renal disease and a host of other chronic medical issues, understand that the importance of diet control could not be stressed enough. As frustrating as it might be, in order to keep yourself as healthy and comfortable as possible you will need to keep your diet under control. Not only could diet control be potentially lifesaving, but you will feel more comfortable and you could even slow the progression of your renal disease.
Dietary Restrictions in Renal Disease
The renal diet, a special diet designed for individuals with renal disease, is a vital tool in managing chronic kidney disease. It aims to reduce stress on the kidneys, slow disease progression, and maintain overall health. Key components of the renal diet include:
- Controlled Protein Intake: Limiting protein helps reduce the accumulation of waste products in the bloodstream, lessening the strain on compromised kidneys.
- Sodium Restriction: Lowering salt intake helps manage blood pressure and prevent fluid retention, common concerns in CKD.
- Phosphorus and Potassium Control: Regulating these minerals is crucial to prevent imbalances that can harm bone health and the cardiovascular system.
- Fluid Management: Monitoring fluid intake prevents fluid overload and edema.
- Calorie Balance: Maintaining a healthy weight is vital since obesity can exacerbate kidney issues.
- Personalized Plans: The renal diet is tailored to individual CKD stages, nutritional requirements, and medical history.
Regular nutritional counseling and lab monitoring are essential. By adhering to prescribed dietary restrictions while ensuring adequate nutrition, CKD patients can enhance their quality of life and decelerate kidney disease progression, making the renal diet a cornerstone of renal care.
Benefits of Diet Control
Adhering to the renal diet offers numerous benefits for individuals with chronic kidney disease. Here are some key advantages:
- Slowed Disease Progression: The renal diet can help slow the progression of CKD by reducing the workload on the kidneys, preserving their function, and delaying the need for dialysis or transplantation.
- Blood Pressure Management: By controlling sodium intake, the renal diet helps regulate blood pressure, reducing the risk of hypertension-related complications.
- Electrolyte Balance: Managing potassium and phosphorus levels promotes bone health and prevents dangerous imbalances that can lead to heart and muscle problems.
- Symptom Relief: Following dietary restrictions can alleviate symptoms such as fluid retention, swelling, and fatigue, leading to an improved quality of life.
- Prevention of Complications: The renal diet minimizes the risk of complications like cardiovascular disease and bone disorders commonly associated with CKD.
- Better Nutritional Status: With guidance from healthcare providers and dietitians, patients can achieve balanced nutrition despite dietary restrictions.
Incorporating the renal diet into daily life is essential for managing CKD effectively, enhancing overall health, and improving long-term outcomes.
The Challenge of Resistance and the Power of Embracing Change
Some people have a hard time in the beginning because they are resistant to change. You have been living your life a certain way this entire time, and now someone is asking you to change everything. That can be understandably frustrating, but in order to help yourself you will have to come around eventually. As the saying goes, “Try it, you might like it”.
Overcoming Resistance Challenges
Adapting to lifestyle changes due to kidney disease can be challenging, but it's essential for managing the condition effectively. Overcoming resistance to change often involves a combination of strategies.
Education is key. Understanding why these changes are necessary can reduce resistance. Learn about how they can improve your health and quality of life.
Consider a gradual transition instead of abrupt shifts. Make gradual changes to your diet and routines. This makes the adjustment more manageable.
Set achievable goals. Establish realistic goals and celebrate your successes along the way. Small victories can boost motivation.
Seek support from your healthcare team, friends, and family. Their guidance and encouragement can make a significant difference.
Consider professional guidance. Consult a registered dietitian or counselor for tailored advice and coping strategies.
Maintain a positive focus. Concentrate on the benefits of change, such as better health and increased energy.
Practice mindfulness. Use stress-reduction techniques to manage anxiety related to change.
By approaching lifestyle adjustments with patience, support, and a positive mindset, individuals with kidney disease can ease resistance and improve their overall well-being.
Benefits of Embracing Change
Embracing lifestyle changes following a CKD diagnosis can yield substantial benefits for overall health and well-being. First and foremost, these changes are crucial for slowing the progression of kidney disease, preserving kidney function, and avoiding complications. By adhering to dietary restrictions, individuals can manage blood pressure, control phosphorus and potassium levels, and reduce the strain on their kidneys.
Additionally, lifestyle changes contribute to improved cardiovascular health, reducing the risk of heart-related issues that often accompany CKD. Healthy dietary habits can lead to better weight management, enhanced energy levels, and improved quality of life.
Moreover, embracing these changes fosters a sense of empowerment and control over one's health, which can boost confidence and mental well-being. It allows individuals to actively participate in their healthcare and make informed choices. Ultimately, these changes pave the way for a higher quality of life while living with CKD.
The Importance of Seeking Support From Loved Ones
Sometimes, making big changes to your lifestyle can be done more easily if you rally the people around you for support. Let the people closest to you know what is going on and help them understand the importance of managing your renal disease. This way, when people come over or invite you over for tea or dinner, they will hopefully be less likely to encourage you to eat things that you shouldn't.
Building Strong Support Systems
It's crucial to establish a strong support system when dealing with kidney disease. You're not just battling the physical symptoms; emotional coping is equally essential, and you can't do it alone.
A robust network of caregivers, family members, and friends can significantly reduce the stress associated with managing your kidney disease. Consider these options:
- Joining Support Groups: Here, you'll find people who understand exactly what you're going through.
- Seeking Family Counseling: It helps everyone involved cope better and strengthens collective resilience.
- Engaging in Therapeutic Activities: These activities contribute to your overall well-being and provide a distraction from constant worry.
Communication With Loved Ones
Having open and honest conversations with those close to you is a necessity when enduring health struggles. The emotional impact of managing your kidney disease can be overwhelming, altering relationship dynamics in unexpected ways. It's important for you to initiate supportive conversations about these changes, fostering understanding and empathy.
But don't forget, it's not just about sharing; it's also about listening. Understanding the emotional resilience of others as they react to your condition can offer insight into their coping strategies. This mutual exchange helps build stronger bonds and provides an emotional cushion during difficult times.
Everyone copes differently, so remember to be patient and kind with yourself and those around you. Communication isn't always easy, but it's key in serving others while navigating health challenges together.
The Importance of Following Medical Advice in Managing Kidney Disease
Above any other inspirations or suggestions, it is very important that you follow the directions of your physicians and nutritionists. Not only are they medical professionals that have experience with this disease, but they are knowledgeable of your particular case and needs. Listen to their advice, and always discuss any changes with them first.
Trusting Professional Guidance
Relying on your doctor's advice can greatly help in managing your kidney disease effectively. However, it's essential to approach this with professional skepticism - not undermining their expertise, but ensuring you fully understand the advice given. Trust building shouldn't be one-sided; as a patient, feel empowered to ask questions and seek expert consultation when needed.
Particularly in today's digital age where misinformation is rampant:
- Always fact-check before believing anything concerning your health.
- Keep open lines of communication with healthcare professionals for any queries.
- Utilize reliable sources for additional information.
Personalized Medications Plan and Dietary Recommendations
A personalized medication plan and dietary recommendations are indispensable for effective CKD management. Kidney disease is highly variable, with individual differences in its progression and complications. A tailored medication plan ensures that patients receive the right medications at the appropriate dosages, addressing specific needs like hypertension, anemia, or phosphate control.
Likewise, personalized dietary recommendations are vital. The renal diet is not one-size-fits-all; it must be customized to a patient's stage of CKD, comorbidities, and nutritional requirements.
Personalization helps control blood pressure, minimize the burden on the kidneys, and regulate electrolyte imbalances. It also takes into account patients' preferences and cultural factors, increasing adherence.
Together, personalized medication and dietary plans optimize CKD management, slowing progression, reducing complications, and enhancing overall well-being for those living with this condition. Regular monitoring and adjustments by healthcare professionals are essential components of this individualized approach.
Frequently Asked Questions
Kidney disease can have far-reaching effects on overall health. Since the kidneys play a central role in filtering waste and regulating fluids and electrolytes, their dysfunction can lead to numerous complications. These may include high blood pressure, fluid retention, electrolyte imbalances, anemia, bone problems, cardiovascular disease, and weakened immunity. Kidney disease can also impact mental health, causing stress and depression. Timely management, including medication, dietary changes, and lifestyle adjustments, is crucial to mitigate these effects and maintain overall well-being.
Kidney disease can lead to various psychological impacts, including stress, anxiety, depression, and feelings of isolation. Managing these effects is essential for overall well-being. Seeking support from friends, family, or support groups can help. Additionally, mental health professionals can provide counseling or therapy. Adopting stress-reduction techniques like mindfulness or meditation can be beneficial. Staying informed about your condition and following treatment plans can provide a sense of control. Remember that addressing the psychological aspects of kidney disease is vital for maintaining a positive outlook and quality of life.
Chronic Kidney Disease Can Be Managed
In managing your kidney disease, it's crucial to understand the influencing factors and take proactive steps.
Managing your renal disease diet might seem difficult right now, but with these tips and some understanding, you might feel better about it. Use these tips to find help and help yourself with managing your renal disease diet.