CKD Diet Guidelines
When you have chronic kidney disease or CKD, you need to follow a special type of diet to ensure that your body will continue to function well despite your kidney disease. A CKD diet or renal diet will control the amount of protein, phosphorus, calcium, sodium, and potassium in your diet, since your kidneys can no longer remove the toxins and waste products in your body.
If you have CKD, you need to have a CKD diet in order to decrease the workload of your kidney and maintain its function. You will need a nutritionist to help you plan your CKD diet. But for the meantime, here are the guidelines that you need to remember if you are planning to have a CKD diet.

Jump to:
- Key Takeaways
- Understanding the Role of Nutrition in CKD
- Overview of Diets for CKD
- The Importance of Carbohydrate Management in CKD
- Managing Protein Intake in CKD
- Controlling Phosphorus Intake for CKD Patients
- Reducing Sodium Intake for Better Kidney Health
- Managing Potassium Intake in a CKD Diet
- The Role of Fluid Intake in Managing CKD
- Guidelines for Dining Out With CKD
- Frequently Asked Questions
- By Following The CKD Diet, You Can Live Your Best Life Quality
Key Takeaways
- Managing nutrition in CKD, including protein balance, phosphorus, potassium, sodium, and fluid control, is crucial for kidney health.
- Proper CKD nutrition can slow disease progression, control blood pressure, and alleviate symptoms while preventing complications.
- The renal diet emphasizes protein restriction, mineral control, sodium reduction, and balanced nutrition, tailored to CKD stages.
- Dialysis patients have higher protein needs but must still manage minerals, sodium, and fluid, while the DASH diet offers heart-healthy principles.
- Plant-based diets can benefit CKD patients, but they require careful planning, carbohydrate management is vital, and consulting healthcare professionals is essential.
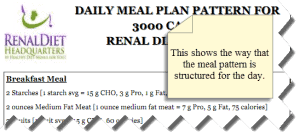
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding the Role of Nutrition in CKD
In the complex landscape of Chronic Kidney Disease, understanding the pivotal role of nutrition is paramount. This section looks into the intricate interplay between diet and CKD, shedding light on common nutritional challenges faced by individuals with this condition.
From the delicate balance of protein intake to the management of phosphorus, potassium, and sodium, we explore the nuanced world of renal nutrition. Moreover, we unveil the profound benefits of a well-structured diet in CKD management, showcasing how proper nutrition can be a powerful ally in preserving kidney health and enhancing overall well-being.
Nutritional Issues in CKD
Chronic Kidney Disease presents a range of nutritional challenges that require careful management.
One primary concern is protein intake. CKD patients often need to restrict protein to lessen the burden on compromised kidneys, but inadequate protein can lead to malnutrition and muscle wasting.
Phosphorus control is equally vital. Damaged kidneys struggle to excrete excess phosphorus, leading to elevated levels in the blood, which can weaken bones and harm cardiovascular health.
Potassium regulation is another issue. High potassium foods like bananas and potatoes can be problematic, as hyperkalemia (high potassium levels) can disrupt heart rhythm.
Sodium restriction is crucial to manage fluid balance and blood pressure, so avoiding foods high in sodium is paramount.
Additionally, CKD patients must pay attention to fluid intake, vitamin and mineral deficiencies, and caloric intake to prevent weight loss or gain.
Balancing these nutritional issues is key to managing CKD effectively and slowing disease progression. Regular monitoring and guidance from healthcare professionals and dietitians are essential for tailored dietary plans.
Balancing Diet With CKD
A proper diet plays an important role in managing Chronic Kidney Disease (CKD) and offers numerous benefits for individuals grappling with this condition:
- Slowed Disease Progression: A well-structured renal diet can slow down the progression of CKD, preserving kidney function over time.
- Blood Pressure Control: Proper diet helps manage blood pressure, a common complication in CKD. Reduced sodium intake and balanced nutrition support better blood pressure regulation.
- Phosphorus and Potassium Control: Dietary modifications help maintain optimal levels of these minerals in the blood, preventing complications such as bone disease and heart arrhythmias.
- Protein Balance: Proper protein intake helps prevent muscle wasting and malnutrition, two issues CKD patients are vulnerable to. It ensures that the body receives essential amino acids without overburdening the kidneys.
- Symptom Management: A suitable diet can alleviate CKD symptoms like edema (fluid retention), fatigue, and anemia, leading to an improved quality of life.
- Prevention of Other Health Complications: A well-managed diet can lower the risk of complications like cardiovascular disease and diabetes, which often accompany CKD.
In essence, a proper diet tailored to individual needs is an essential tool in managing CKD, enhancing overall health, and improving the patient's quality of life. Consulting with a healthcare provider or dietitian is critical to create a personalized dietary plan.
Overview of Diets for CKD
Navigating the dietary landscape with Chronic Kidney Disease involves a spectrum of tailored nutritional approaches. This article section delves into four specific diets crucial in CKD management: the renal diet, designed to alleviate the strain on compromised kidneys; the dialysis diet, fine-tuned for those undergoing renal replacement therapy; the DASH diet, renowned for its heart-healthy principles; and the plant-based diet, which offers a sustainable approach to renal nutrition.
Exploring the nuances of these CKD-specific diets unveils a diverse toolkit for individuals seeking optimal kidney health and overall well-being.
Renal Diet
The renal diet, also known as the kidney diet, is a specialized nutritional plan designed to support individuals with Chronic Kidney Disease. Its primary goal is to alleviate the workload on the kidneys while maintaining overall health. Key principles of the renal diet include:
- Protein Restriction: Limiting high-protein foods to reduce the production of waste products, such as urea and creatinine, which damaged kidneys struggle to filter.
- Phosphorus and Potassium Control: Managing intake of foods rich in these minerals, as elevated levels can harm bone health and heart function.
- Sodium Reduction: Lowering sodium to regulate blood pressure and fluid balance.
- Fluid Management: Monitoring fluid intake to prevent fluid overload and edema.
- Balanced Nutrition: Ensuring adequate calorie intake and intake of essential vitamins and minerals to prevent malnutrition.
- Regular Monitoring: Ongoing assessment and adjustment of the diet based on kidney function and individual needs.
A well-structured renal diet helps slow CKD progression, manages complications, and enhances the overall quality of life for those with kidney disease.
Dialysis Diet
The Dialysis diet is a specialized nutritional plan tailored for individuals undergoing renal replacement therapy, such as hemodialysis or peritoneal dialysis.
It differs significantly from the pre-dialysis renal diet due to the additional challenges and considerations brought about by dialysis.
In the Dialysis diet:
- Increased Protein: Dialysis removes protein waste products, so protein intake is often higher compared to the pre-dialysis renal diet to prevent muscle wasting.
- Phosphorus Control: Dialysis is less effective at removing phosphorus, so strict phosphorus restriction continues, along with the use of phosphate binders.
- Potassium Management: Dietary potassium may be less restricted than in pre-dialysis, but careful monitoring is essential.
- Sodium and Fluid Control: Sodium and fluid intake are still regulated to manage blood pressure and prevent fluid overload.
- Caloric Needs: Dialysis may increase calorie needs due to metabolic changes.
The Dialysis diet is more flexible regarding protein but still focuses on controlling phosphorus, potassium, sodium, and fluid, tailored to individual patient needs.
DASH Diet Benefits
The DASH (Dietary Approaches to Stop Hypertension) diet is a heart-healthy eating plan with potential benefits for individuals with Chronic Kidney Disease, particularly those managing hypertension, a common complication of CKD. The DASH diet emphasizes:
- Sodium Reduction: It prioritizes a lower sodium intake, which helps control blood pressure, a key concern in CKD.
- Rich in Fruits and Vegetables: The diet encourages ample consumption of fruits and vegetables, which provide essential nutrients and antioxidants, supporting overall health.
- Moderate Protein: While not specifically designed for CKD, the DASH diet includes moderate protein intake, aligning with general renal diet recommendations.
- Whole Grains: It promotes whole grains, which are beneficial for sustained energy and dietary fiber.
- Limitation of Processed Foods: DASH advises against processed and high-sodium foods, which is consistent with CKD dietary guidelines.
While not explicitly designed for CKD, the DASH diet's focus on heart-healthy, whole foods aligns with many renal diet principles and can be adapted to support kidney health in individuals with CKD, especially those with hypertension.
Plant-Based Diets Impact
Plant-based diets, such as vegetarian or vegan diets, have gained recognition as viable options for individuals with Chronic Kidney Disease. These diets emphasize:
- Lower Protein Content: Plant-based diets naturally contain less protein compared to animal-based diets, which can be beneficial for CKD patients who need to restrict protein intake.
- Reduced Phosphorus and Potassium: Many plant-based foods are lower in phosphorus and potassium, which are critical considerations in CKD to manage mineral imbalances.
- Heart Health: Plant-based diets can improve cardiovascular health, a significant concern for CKD patients, by reducing blood pressure and cholesterol levels.
- Antioxidants and Fiber: They are rich in antioxidants and dietary fiber, supporting overall health and potentially reducing inflammation.
However, a plant-based diet requires careful planning to ensure adequate protein intake and prevent nutritional deficiencies.
CKD patients considering this diet should work closely with a dietitian to create a balanced and kidney-friendly plant-based eating plan tailored to their specific needs.
The Importance of Carbohydrate Management in CKD
Now, let’s delve into the often-overlooked yet critical aspect of carbohydrate intake in the context of Chronic Kidney Disease and renal diabetes management.
Carbohydrates play a pivotal role in the nutritional well-being of CKD patients, impacting blood glucose control, energy levels, and overall health. Understanding the intricacies of carbohydrate intake and learning how to control it effectively is essential for individuals navigating the complex terrain of CKD, particularly those with renal diabetes.
Discover how thoughtful carbohydrate management can be a powerful ally in optimizing kidney health and enhancing the quality of life for those facing these multifaceted challenges.
Importance of Carbohydrate Intake in CKD
Balanced carbohydrate intake is of paramount importance in the management of Chronic Kidney Disease for several reasons.
Firstly, carbohydrates are a primary source of energy, crucial for overall well-being and maintaining energy levels, which CKD patients often struggle with due to fatigue.
Secondly, controlling carbohydrate intake helps regulate blood glucose levels. Many CKD patients also have diabetes or are at risk of developing it, making blood sugar management critical to prevent further kidney damage and complications.
Furthermore, well-distributed carbohydrates can help prevent muscle wasting and malnutrition, which are common concerns in CKD.
Balancing carbohydrates also involves choosing the right types, favoring complex carbohydrates like whole grains, fruits, and vegetables over simple sugars. This supports heart health and minimizes the risk of cardiovascular complications, which often accompany CKD.
Managing carbohydrate intake in CKD ensures energy, blood sugar control, muscle preservation, and overall health, making it a fundamental aspect of renal nutrition and disease management.
Carbohydrate Counting Benefits
Carbohydrate control is particularly crucial in the renal diet, especially for individuals with Renal Diabetes (or Diabetic Kidney Disease). This specialized dietary approach focuses on managing blood glucose levels to prevent further kidney damage while also addressing the unique nutritional needs of CKD patients.
Carbohydrates from high-fiber sources like whole grains, fruits, and vegetables are encouraged as they have a gentler impact on blood sugar levels. Portion control and consistent carbohydrate intake throughout the day help stabilize glucose levels, reducing the risk of hyperglycemia.
Monitoring carbohydrate intake, along with phosphorus, potassium, and sodium content, is vital in managing renal diabetes. A registered dietitian can help individuals with CKD and Renal Diabetes create a personalized meal plan that balances carbohydrates while supporting kidney function and blood glucose control, optimizing overall health outcomes.
Managing Protein Intake in CKD
Managing protein intake is a pivotal aspect of Chronic Kidney Disease management. Protein plays a dual role as a necessary nutrient and a potential burden on compromised kidneys. Understanding the impact of protein, and the differing requirements for pre-dialysis and dialysis patients.
Let us discover the nuanced world of protein management in CKD, providing insights into how tailored approaches can support kidney health and overall well-being for individuals at different stages of their renal journey.
Protein's Impact on Kidneys
Protein's impact on the kidneys is a critical consideration for individuals with Chronic Kidney Disease. While protein is essential for growth, repair, and overall health, its metabolism produces waste products, including urea and creatinine, which healthy kidneys efficiently eliminate.
However, in CKD, impaired kidney function can hinder the clearance of these waste products, leading to their accumulation in the bloodstream. Excessive protein intake can exacerbate this issue, overloading the kidneys and accelerating the progression of CKD.
On the other hand, inadequate protein intake can result in malnutrition and muscle wasting. Therefore, striking the right balance in protein intake is essential, often requiring careful monitoring and personalized guidance from healthcare professionals to support kidney health effectively.
Non Dialysis Chronic Kidney Disease Protein Requirements
Protein intake limits vary depending on the stage of Chronic Kidney Disease (CKD) to mitigate its impact on kidney function.
For individuals in CKD stages 1 and 2, the recommendation is to restrict dietary protein to no more than 0.8 grams per kilogram of their ideal body weight. This conservative approach aims to reduce the burden on the kidneys while maintaining overall health.
As CKD progresses to stages 3, 4, and 5 (Non Dialysis-CKD), the 2020 KDOQI guidelines advise further protein reduction, with recommended intake ranging from 0.55 to 0.60 grams per kilogram per day for stable patients. These lower limits are designed to slow the advancement of kidney disease and minimize the accumulation of waste products in the bloodstream.
Individual protein requirements may still vary, emphasizing the importance of personalized dietary plans and regular monitoring under the guidance of healthcare professionals to manage CKD effectively.
Dialysis Protein Needs
For individuals undergoing dialysis, whether peritoneal dialysis or hemodialysis, protein intake recommendations are notably different compared to those with Non Dialysis Chronic Kidney Disease. The dietary guidelines suggest a higher protein intake ranging from 1.0 to 1.2 grams per kilogram of body weight per day.
This elevated protein allowance is essential because dialysis effectively removes waste products, including urea and creatinine, from the bloodstream. Consequently, dialysis patients experience higher protein loss and an increased risk of malnutrition and muscle wasting.
By increasing protein intake within this range, patients can help counteract these effects, supporting muscle maintenance, overall nutrition, and a better quality of life. However, precise protein requirements may vary among individuals, warranting personalized dietary plans and ongoing monitoring to optimize their health during dialysis treatment.
Controlling Phosphorus Intake for CKD Patients
Controlling phosphorus intake is a critical component of managing Chronic Kidney Disease. Here, we delve into the intricacies of dietary phosphorus management for CKD patients, emphasizing the importance of limiting high-phosphorus foods.
Excessive phosphorus can disrupt mineral balance, particularly calcium, which may weaken bones and contribute to renal osteodystrophy, a common complication of advanced CKD. Understanding how to navigate phosphorus-rich dietary choices and the potential consequences of excessive phosphorus on bone health is essential for individuals seeking to preserve their overall well-being while dealing with the challenges of CKD.
Limiting High-Phosphorus Foods
Limiting high-phosphorus foods is a fundamental dietary strategy for managing Chronic Kidney Disease.
In CKD, impaired kidney function leads to difficulties in excreting excess phosphorus from the body, resulting in its accumulation in the bloodstream. This excess phosphorus can disrupt calcium balance, weakening bones and potentially causing vascular calcification, a serious cardiovascular risk.
To address this issue, CKD patients are typically advised to limit their daily phosphorus intake to a specific range, often falling between 800 to 1,000 milligrams. This involves avoiding or minimizing foods rich in phosphorus, such as dairy products, nuts, seeds, processed meats, and dark colored sodas and other carbonated beverages.
Instead, patients are encouraged to opt for lower-phosphorus alternatives and to carefully read food labels for phosphorus content.
Balancing phosphorus intake plays a crucial role in preserving bone health, minimizing the risk of vascular calcification, and supporting overall well-being for individuals with CKD, making it an integral part of renal nutrition. Regular monitoring and guidance from healthcare professionals or dietitians are vital for effective management.
Phosphorus Impact on Bones
Phosphorus is a mineral vital for bone health, but its balance in the body is delicate. In Chronic Kidney Disease, impaired kidney function leads to difficulty in excreting excess phosphorus, and elevated blood phosphorus levels can have severe consequences for bones, often resulting in a condition called renal osteodystrophy.
Excess phosphorus disrupts the body's calcium-phosphorus balance, prompting the release of calcium from bones into the bloodstream. Over time, this leaching of calcium can weaken bones, causing them to become brittle and prone to fractures.
Renal osteodystrophy encompasses a range of bone abnormalities, including osteoporosis (reduced bone density), osteitis fibrosa (bone softening), and vascular calcification (calcium buildup in blood vessels).
Managing phosphorus intake and adhering to prescribed phosphorus binders are critical for CKD patients to prevent or mitigate the impact of renal osteodystrophy on bone health and overall well-being. Regular monitoring and guidance from healthcare professionals are essential components of effective management.
Reducing Sodium Intake for Better Kidney Health
The effects of sodium on kidney function are profound, particularly for individuals with Chronic Kidney Disease. Sodium plays a crucial role in regulating fluid balance and blood pressure, both of which are critically important for kidney health. However, excessive sodium intake can lead to elevated blood pressure and fluid retention, increasing the strain on already compromised kidneys.
In your CKD diet, you need to limit your sodium intake to 1500 milligrams per day. Let’s now tackle the intricate relationship between sodium and CKD, emphasizing the benefits of a low-sodium diet.
Discover how reducing sodium intake can alleviate stress on the kidneys, support blood pressure control, and enhance overall renal well-being for individuals navigating the complexities of CKD.
Sodium's Impact on Kidneys
Sodium, a crucial electrolyte, significantly impacts kidney function and overall health, particularly in the context of Chronic Kidney Disease. The kidneys play a central role in regulating sodium levels in the body. Excessive sodium intake can have detrimental effects on kidney health.
In CKD, compromised kidneys struggle to filter excess sodium from the bloodstream, leading to sodium retention and fluid buildup. This can result in edema, hypertension (high blood pressure), and increased cardiovascular risk. Elevated blood pressure, in turn, accelerates the progression of CKD, creating a vicious cycle.
Moreover, high sodium intake is associated with an increased risk of heart disease and stroke, which are common comorbidities in CKD. Reducing sodium intake is essential for CKD patients to manage blood pressure, alleviate the strain on the kidneys, and reduce the risk of fluid overload.
A low-sodium diet is a key component of renal nutrition and plays a pivotal role in preserving kidney function and overall well-being in CKD.
Implementing Low-sodium Diets
Implementing low-sodium diets for individuals with Chronic Kidney Disease is essential to manage hypertension, minimize fluid retention, and support kidney health. Here are key steps in implementing such diets:
- Consultation with a Dietitian: CKD patients should work closely with a registered dietitian specializing in renal nutrition. A dietitian can assess the patient's specific needs, develop a tailored meal plan, and provide ongoing guidance.
- Limit Processed Foods: Processed and restaurant foods often contain high sodium levels. Reducing or eliminating these items from the diet is crucial. Opt for fresh, whole foods whenever possible.
- Read Food Labels: CKD patients should become adept label readers, looking for terms like sodium chloride, monosodium glutamate (MSG), and baking soda (sodium bicarbonate). Foods with high sodium content should be avoided.
- Use Herbs and Spices: To enhance flavor without adding sodium, use herbs, spices, and salt substitutes. These can make low-sodium meals enjoyable.
- Monitor Fluid Intake: Controlling fluid intake is another aspect of sodium management. A dietitian can provide guidance on how much fluid is appropriate for each patient.
- Regular Monitoring: Frequent monitoring of blood pressure, sodium levels, and overall health status is essential. Adjustments to the diet may be necessary based on these assessments.
By diligently implementing low-sodium diets under the guidance of healthcare professionals, CKD patients can effectively manage their condition, alleviate kidney stress, and reduce the risk of related complications.
Managing Potassium Intake in a CKD Diet
Managing potassium intake is a critical aspect of maintaining kidney health in individuals with Chronic Kidney Disease. This section looks into the intricacies of potassium management within a CKD diet, focusing on potassium-rich foods to avoid.
Elevated potassium levels, known as hyperkalemia, can pose severe health risks, including heart rhythm disturbances. By understanding which foods to limit or avoid and how to maintain a balanced potassium intake, CKD patients can effectively protect their heart and overall well-being while navigating the complexities of renal nutrition.
Potassium-rich Foods to Avoid
A renal diet necessitates vigilance in avoiding potassium-rich foods to maintain proper potassium balance in individuals with Chronic Kidney Disease. High-potassium levels, or hyperkalemia, can lead to heart rhythm disturbances and pose severe health risks. Foods that should be limited or avoided include:
- Bananas: Known for their potassium content, they top the list of high-potassium foods.
- Oranges and Orange Juice: These citrus fruits are potassium-rich and should be consumed in moderation.
- Tomatoes: Fresh tomatoes, tomato sauce, and tomato-based products are potassium-packed.
- Potatoes: Especially when baked or mashed, they are high in potassium.
- Spinach: Leafy greens like spinach are a potent source of potassium.
- Avocado: While nutritious, avocados are potassium-dense and should be restricted.
- Beans and Lentils: These protein-rich foods are also potassium-rich.
- Dairy Products: Milk, yogurt, and cheese can contribute to potassium intake.
- Processed Foods: Many processed foods, canned soups, and fast food items contain hidden potassium.
By carefully monitoring and restricting these high-potassium foods, CKD patients can effectively manage their potassium levels and minimize the risk of complications associated with hyperkalemia. Consulting with a dietitian is essential for creating a personalized meal plan that balances nutrition and potassium intake.
Consulting Healthcare for Guidance
Excessive potassium, or hyperkalemia, poses significant complications for individuals with Chronic Kidney Disease. The impaired kidney function in CKD makes it challenging for the body to regulate potassium levels effectively, leading to a buildup of this mineral in the bloodstream.
One of the most critical complications of hyperkalemia is the risk of irregular heart rhythms. High potassium levels can disrupt the electrical signals in the heart, leading to arrhythmias, palpitations, or even cardiac arrest. This is a potentially life-threatening situation, especially for those with pre-existing heart conditions.
Hyperkalemia can also affect muscle function, causing weakness and, in severe cases, paralysis. This can significantly impact a person's mobility and overall quality of life, making it important to manage potassium levels carefully.
Gastrointestinal symptoms are another consequence of high potassium levels, with nausea, vomiting, and abdominal pain being common. These symptoms can further contribute to malnutrition and dehydration in CKD patients.
Tingling sensations or numbness, particularly in the extremities, can also occur due to hyperkalemia, further adding to the discomfort experienced by CKD patients.
Preventing and managing hyperkalemia through dietary restrictions, medications, and close medical monitoring is essential for CKD patients to protect their cardiovascular health and overall well-being. Proper management can mitigate the risk of these complications and improve the quality of life for those living with CKD.

The Role of Fluid Intake in Managing CKD
As previously mentioned, kidney disease makes you retain fluid since your kidneys cannot excrete excess fluid in your body. This could lead to swelling, or worse, fluid buildup in your lungs, thus making it hard for you to breathe.
Your suggested fluid intake in your CKD diet will depend on your urine output, fluid buildup, and blood pressure. You should also remember that foods also contain fluids, and that these should be taken into account in your CKD diet.
Fluid Retention Dangers
Fluid retention, or edema, is a common and potentially serious complication for individuals with Chronic Kidney Disease (CKD), particularly those undergoing dialysis treatment. CKD impairs the kidneys' ability to effectively regulate fluid balance, leading to the accumulation of excess fluids in the body.
Complications of fluid retention in CKD include:
- Hypertension (High Blood Pressure): Edema increases blood volume, putting additional strain on the heart and blood vessels, which can lead to hypertension, further exacerbating kidney damage.
- Shortness of Breath: Excess fluid can accumulate in the lungs, causing difficulty in breathing, especially when lying down.
- Swelling: Edema commonly causes swelling in the legs, ankles, and around the eyes, making mobility uncomfortable and limiting daily activities.
- Pulmonary Edema: Severe fluid retention can result in pulmonary edema, a life-threatening condition where fluid fills the lungs, leading to breathing difficulties and a risk of respiratory failure.
- Cardiovascular Complications: Fluid overload can increase the risk of heart failure and contribute to other cardiovascular issues, such as arrhythmias.
Managing fluid retention in CKD, often through dietary restrictions and careful monitoring of fluid intake, is essential to prevent these complications, particularly for dialysis patients who are more susceptible due to the nature of their treatment.
Managing Daily Fluid Intake
Managing daily fluid intake is crucial for preventing fluid retention in Chronic Kidney Disease patients. Here are key strategies:
- Fluid Restriction: CKD patients, especially those on dialysis, may have specific daily fluid allowances. Adhering to these restrictions is vital.
- Monitor Thirst: Pay attention to your body's signals of thirst and drink only when genuinely thirsty.
- Limit High-Fluid Foods: Reduce consumption of high-fluid foods like soups, ice cream, and juicy fruits.
- Measure Fluids: Use measuring cups to monitor fluid intake accurately.
- Choose Ice Chips: Sucking on ice chips can help relieve dry mouth without excessive fluid consumption.
- Limit Sodium: High-sodium foods can lead to thirst. Avoiding excessive salt can help control fluid intake.
- Consult a Dietitian: Work with a renal dietitian to develop a personalized fluid management plan tailored to your specific needs and CKD stage.
By carefully managing daily fluid intake and seeking guidance from healthcare professionals, CKD patients can prevent fluid retention, reduce the risk of complications, and support their overall kidney health.
Guidelines for Dining Out With CKD
As you navigate your journey with chronic kidney disease, it's essential to understand that dining out doesn't have to be off-limits. You can still enjoy meals at restaurants, but the key lies in choosing kidney-friendly establishments and understanding how to decipher menu wording.
In this discussion, we'll guide you on how to make informed decisions about where to eat and what dishes align best with your dietary needs, based on scientific evidence and expert recommendations.
Choosing Kidney-Friendly Restaurants
Dining out with Chronic Kidney Disease requires thoughtful choices to ensure your meal aligns with renal dietary restrictions. When selecting kidney-friendly restaurants:
- Research Ahead: Look for restaurants with online menus, nutritional information, or specific dietary sections, making it easier to assess meal options.
- Call Ahead: Contact the restaurant to discuss your dietary needs and inquire if they can accommodate special requests.
- Choose Wisely: Opt for restaurants offering lean protein sources like grilled chicken or fish and plenty of vegetable options. Avoid dishes with high sodium, potassium, or phosphorus content.
- Customize Your Order: Don't hesitate to ask for substitutions or modifications to fit your dietary requirements. Most restaurants are willing to accommodate.
- Portion Control: CKD patients often need smaller portions. Consider sharing an entree or taking leftovers home.
- Beverage Selection: Limit fluids by choosing water or herbal tea over high-sugar or high-sodium beverages.
- Sauce on the Side: Request sauces and dressings on the side to control sodium and phosphorus intake.
- Dessert Alternatives: Fresh fruit or sorbet can be suitable, kidney-friendly dessert options.
Choosing kidney-friendly restaurants and making informed menu choices can make dining out an enjoyable experience while prioritizing your kidney health. Always consult with a dietitian for personalized guidance on dining out with CKD.
Understanding Menu Wording
Understanding menu wording and food labels in restaurants is vital for individuals with Chronic Kidney Disease when dining out. Here are some tips and tricks:
- Ask Questions: Don't hesitate to ask your server about ingredients, preparation methods, and potential modifications to meet your dietary needs.
- Beware of Trigger Words: Watch for words like "grilled," "roasted," or "steamed," which often indicate healthier cooking methods with fewer added fats and salt.
- Avoid High-Sodium Terms: Be cautious of menu items described as "brined," "pickled," "smoked," or "in broth," as they tend to be higher in sodium.
- Look for Kidney-Friendly Phrases: Seek out phrases like "low-sodium," "no-salt-added," or "freshly prepared," which suggest healthier options.
- Consider Side Dishes: Sometimes, side dishes or appetizers offer more kidney-friendly choices than the main courses.
- Review Food Labels: If available, review nutritional information on food labels or ask the restaurant for these details.
- Simplify Orders: Choose dishes with simpler ingredient lists to reduce the risk of hidden high-sodium, potassium, or phosphorus additives.
- Portion Control: Pay attention to portion sizes, as larger servings can contain more of certain nutrients.
By becoming savvy at interpreting menu wording and food labels, CKD patients can make more informed dining choices that align with their dietary restrictions, contributing to better kidney health while enjoying restaurant meals.
Frequently Asked Questions
Common misconceptions about the CKD diet include the belief that all protein should be restricted (when it should be controlled but not eliminated), that all fruits and vegetables are off-limits (when many can be enjoyed in moderation), and that simply reducing sodium is enough (while potassium and phosphorus also need monitoring).
Additionally, there's often a misunderstanding that dietary restrictions mean bland and unenjoyable meals, whereas with proper guidance, CKD patients can still savor flavorful, satisfying dishes that align with their nutritional needs.
In a CKD diet, it's crucial to avoid or strictly limit alcohol and fatty foods. Alcohol can burden the kidneys and interfere with medications, while fatty foods, especially those high in unhealthy trans fats, can contribute to heart disease, a significant risk for CKD patients.
Additionally, excessive alcohol intake can lead to dehydration, further stressing the kidneys. It's essential for CKD patients to prioritize hydration and choose heart-healthy fats over trans fats found in fried and processed foods to safeguard their kidney and overall health.
The CKD diet can impact medication absorption in patients due to dietary restrictions. For instance, certain phosphate binders, commonly prescribed for CKD patients to control phosphorus levels, must be taken with meals. However, if dietary restrictions result in reduced food intake, it can affect the medication's effectiveness.
Additionally, some medications interact with specific foods that CKD patients should limit or avoid, potentially altering their absorption. Therefore, it's crucial for CKD patients to coordinate their medication schedules and dietary choices with healthcare providers or pharmacists to ensure optimal treatment outcomes.
Yes, CKD patients with comorbid conditions like diabetes face unique dietary challenges. The CKD diet needs to strike a balance between managing both conditions. Diabetes requires blood sugar control, which often involves carbohydrate monitoring, while CKD necessitates restrictions on phosphorus, potassium, and sodium.
Coordinating these restrictions can be challenging, as some diabetes-friendly foods may be high in these restricted nutrients. CKD patients with diabetes require individualized dietary plans, often with the guidance of a registered dietitian, to manage both conditions effectively while maintaining overall health.
By Following The CKD Diet, You Can Live Your Best Life Quality
Managing your diet with CKD isn't easy, but it's crucial. Balancing protein and carbs, controlling phosphorus and sodium intake, and monitoring potassium and fluid can significantly impact your kidney health.
With careful planning and adherence to these guidelines, you'll not only manage your CKD symptoms better but also improve your overall health. Remember to always consult with a healthcare professional before making any dietary changes.
Remember to stick to your CKD diet so that you will be able to maintain the highest quality of living achievable for people with chronic kidney disease.
SEE MY RENAL DIET MEAL PLANNERS CLICK HERE!